Volume 13, Issue 3 (Summer 2025)
Iran J Health Sci 2025, 13(3): 247-252 |
Back to browse issues page
Ethics code: IR.KUMS.REC.1401.315
Clinical trials code: 0
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ziapour A. Recommendations to Address Sexual Dysfunction in Patients With Cardiovascular Diseases in Iran: A Policy Brief. Iran J Health Sci 2025; 13 (3) :247-252
URL: http://jhs.mazums.ac.ir/article-1-1014-en.html
URL: http://jhs.mazums.ac.ir/article-1-1014-en.html
Cardiovascular Research Center, Health Policy and Promotion Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran. , arashziapoor@gmail.com
Full-Text [PDF 654 kb]
(490 Downloads)
| Abstract (HTML) (1275 Views)
Full-Text: (334 Views)
Introduction
Cardiovascular diseases (CVDs), one of the leading causes of death, contribute to one-third of deaths globally [1]. In developing countries, the rate reaches 50% [2]. CVDs include ischemic heart disease, coronary heart disease, peripheral arterial disease, chronic hypertension, myocardial infarction, heart failure, and more cardiovascular conditions [3]. The CVD incidence increases for reasons such as having an unhealthy diet, smoking, having low or no physical activity, and exposure to excessive stress [4]. CVDs cause psychological and physical harms that reduce the patient’s quality of life (QoL) [1]. They can also cause sexual dysfunction, physically and mentally [5]. Patients with CVD have reported that their impaired sexual function has negatively affected their overall QoL [6]. Studies indicate that the prevalence of sexual dysfunction among CVD patients can be as high as 89% [2], which is three times greater than that observed in individuals without CVD [5]. Sexual dysfunction refers to difficulties in engaging in a satisfactory sexual activity among couples. Examples of sexual dysfunction include libido disorders, male erectile dysfunction (ED), female sexual arousal disorder, premature ejaculation, orgasm disorders in both males and females, and sexual pain conditions such as vaginismus and dyspareunia [6, 7]. The European Society of Urology defines ED as a persistent inability to attain and maintain an adequate erection for satisfactory sexual activity [6]. Patients with CVD often report symptoms of sexual dysfunction, which include a decrease in sexual desire, a tendency to avoid sexual activities, and feelings of sexual dissatisfaction [1]. Sexual dysfunction in patients with CVDs may result from physical, psychological, and medication-related factors [1, 2]. The physical and psychological effects of CVDs have proven to interfere with sexual activity, causing a reduction in patient QoL that comes from reduced self-esteem, depression, and isolation [8, 9]. Sexual dysfunction may predict CVD before other symptoms such as a cardiovascular event [10]. Patients with CVDs have sleep disorders 3-5 years prior to the emergence of other clinical signs of CVD. This timeframe may be leveraged in the future to implement therapeutic interventions aimed at addressing CVD risk factors at an earlier stage [8]. Epidemiological research indicates that both sexual dysfunction and CVDs are highly prevalent worldwide [1].
Despite its high prevalence, sexual dysfunction is often overlooked in care programs and health policies in Iran. The existing knowledge gap regarding the precise prevalence, contributing factors, and policies to enhance the condition of patients underscores the necessity of the present study. This study aims to determine the global prevalence of sexual dysfunction in patients with CVDs to inform policymakers, government health officials, and advisory organizations about the prevalence of sexual dysfunction in these patients. We also present solutions and policy recommendations to address the psychological and social implications of sexual dysfunction and help make informed decisions to enhance the QoL of CVD patients. Ultimately, this policy brief can serve as a valuable reference for designing clinical and policy interventions within the health system.
Materials and Methods
This research is a “policy brief” that utilizes data from a comprehensive 17-year systematic review and meta-analysis (2003–2023). Various databases, including Scientific Information Database (SID), Magiran, PubMed, Scopus, Web of Science (WOS) and Google Scholar databases, were searched to find the studies in English. The general search strategy was a follows: (Prevalence) OR (prevalence*) AND (“sexual dysfunctions, psychological”) OR (“disorders, sexual aversion”) OR (“orgasmic disorder”) AND (cardiac*) OR (“coronary artery bypass surgery”) OR (CABG) OR (“coronary artery bypass”) OR (“coronary artery bypass”) OR (cardiovascular*). The original research observational studies, including cross-sectional and cohort studies, that had available full texts and reported the prevalence of sexual disorders in patients with CVDs were included. The studies not relevant to the research objective, interventional studies (such as clinical trials and field trials), qualitative studies, case series, case reports, letters to the editor, conference proceedings, theses, and studies involving animal subjects were excluded from the review. The articles whose full texts were not accessible, even after contacting the corresponding authors, as well as duplicate studies, were also excluded. The initial search yielded 2,122 relevant studies. After removal of 792 duplicates and 1,006 studies by screening titles and abstracts, 324 full-text studies were assessed, of which 307 did not meet the inclusion criteria, resulting in 17 studies deemed suitable for the analysis [11-27].
Results
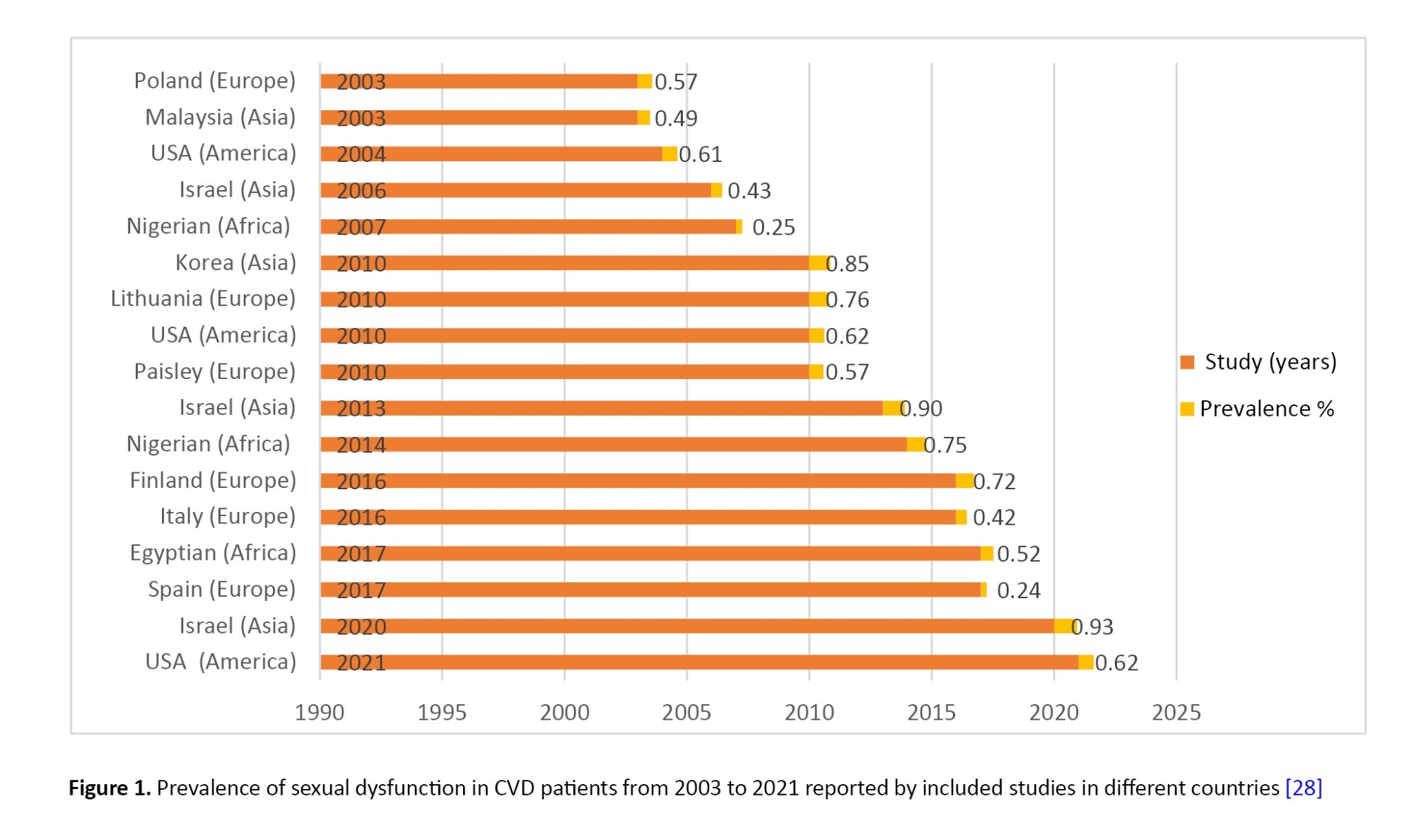
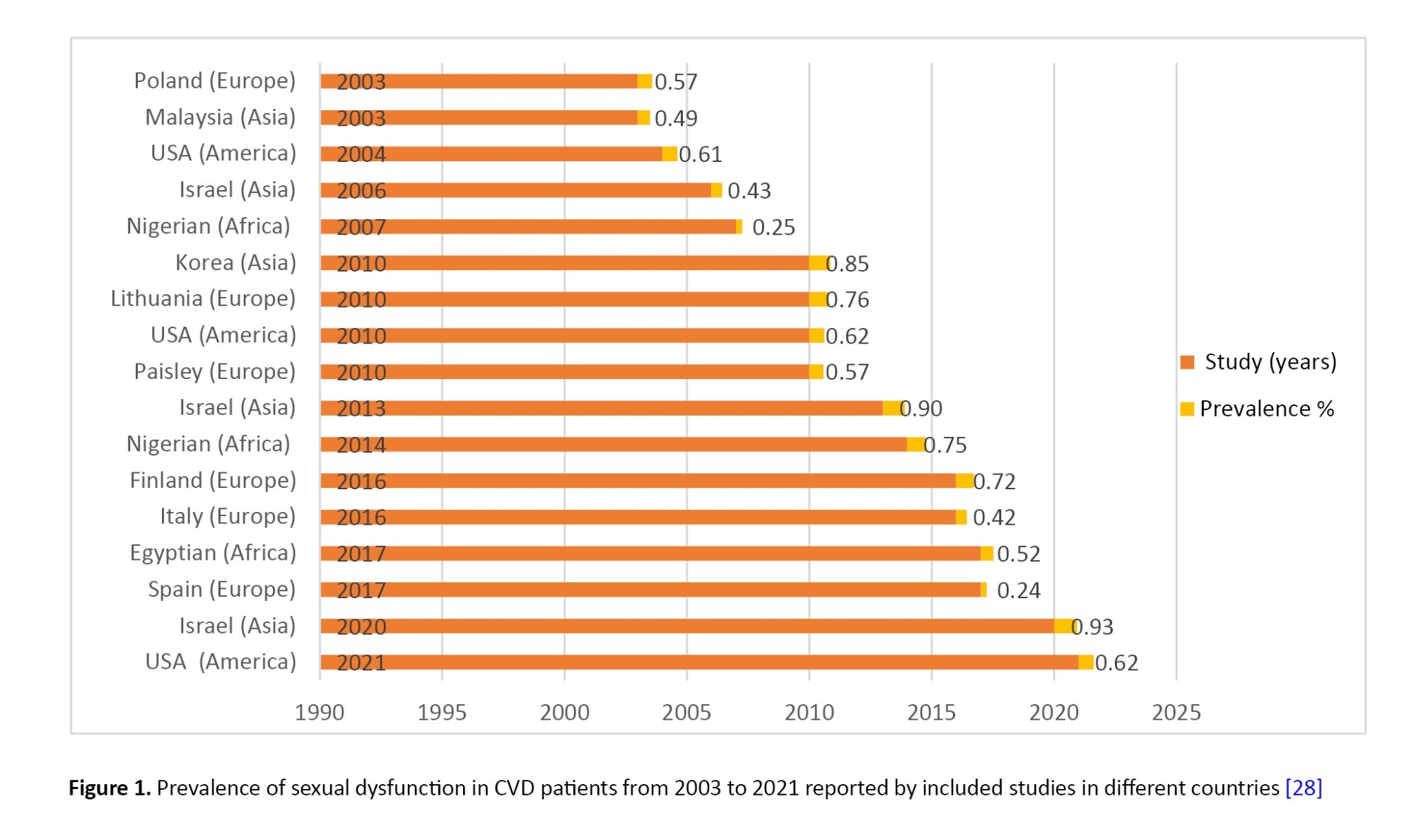
Figure 1 illustrates the prevalence of sexual dysfunction among CVD patients reported a meta-analysis of 17 studies conducted across various countries [28]. The findings indicate that the estimated global prevalence of sexual dysfunction among CVD patients is 62.6% (95% CI, 49.8%, 73.8%), revealing significant regional disparities. This underscores the need for targeted screening and culturally appropriate interventions and emphasizes the importance of region-specific health policies.
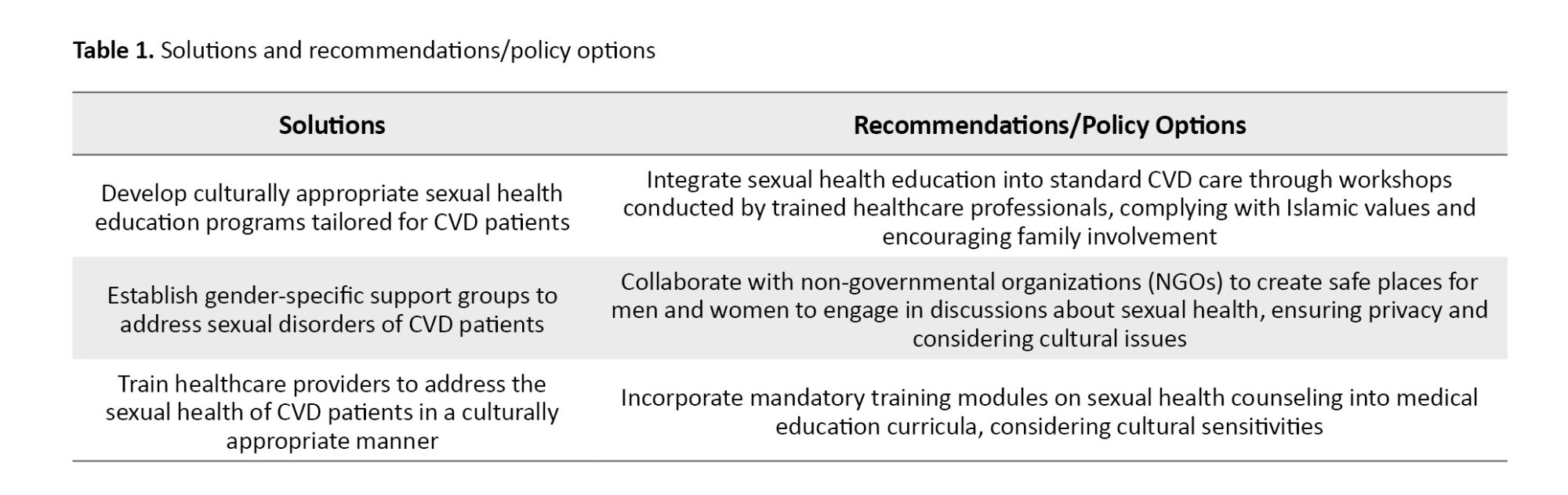
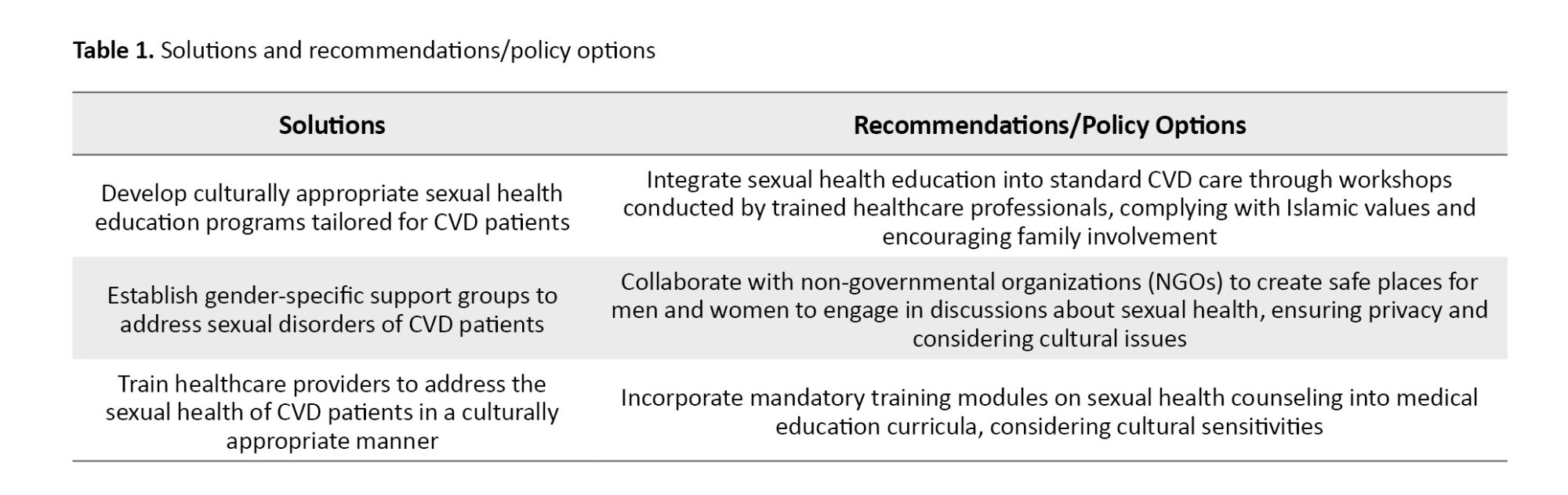
Cardiologists should be aware of the adverse effects of cardiac medications on sexual health. Knowing the side effects of prescribed medications on sexual function allows healthcare providers to take proactive measures to enhance patient health and QoL. Patients need to be adequately informed about the potential side effects of their prescribed medications, enabling them to make informed decisions regarding their treatment. Table 1 outlines the proposed solutions for enhancing sexual health in CVD patients based on the Iranian culture, accompanied by relevant recommendations and policy options.
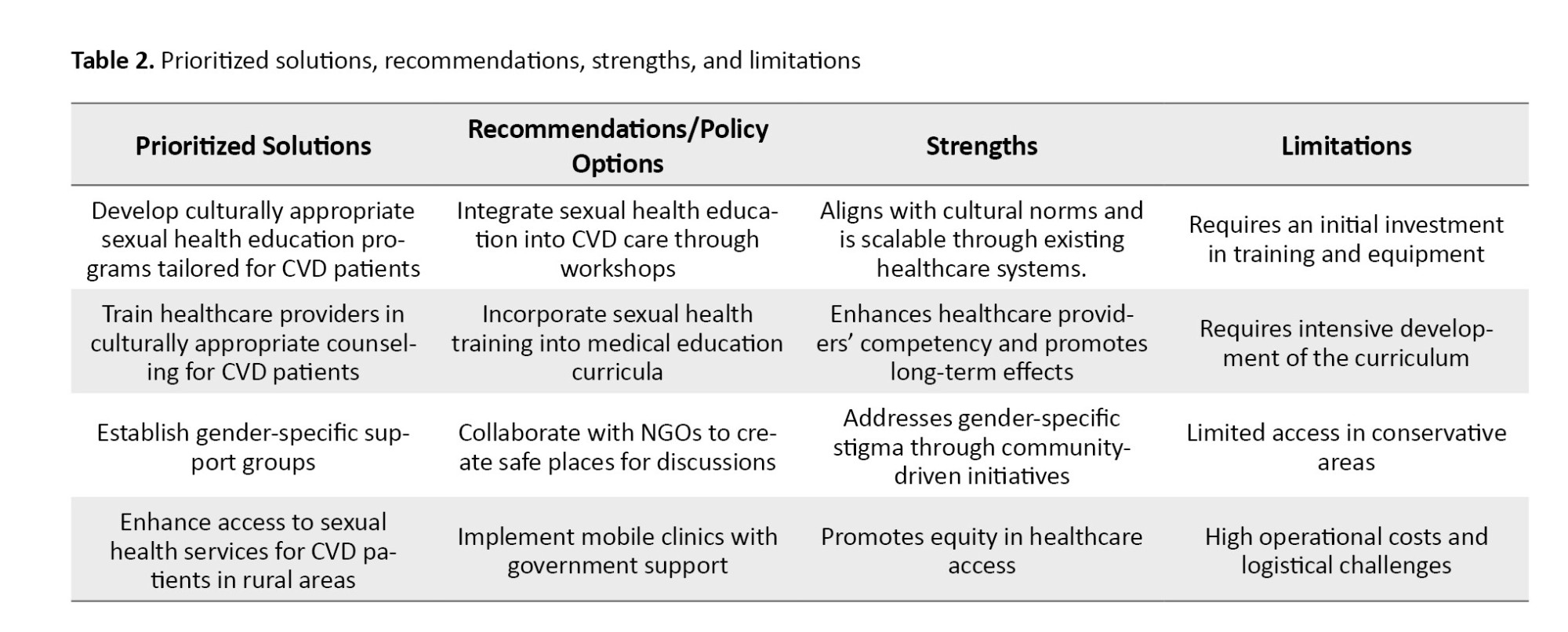
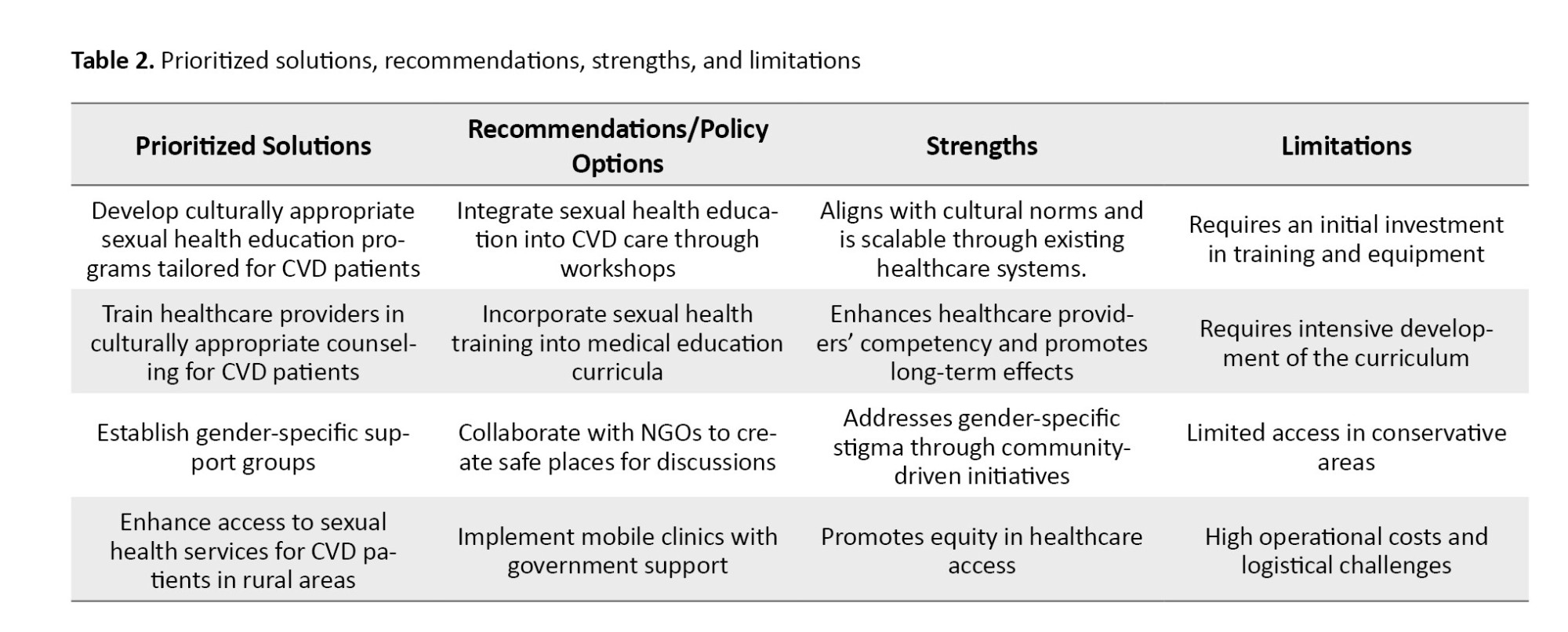
These solutions are prioritized in Table 2, along with policy recommendations, detailing their strengths and weaknesses.
Discussion
The solutions and policy recommendations outlined in this policy brief seek to help address the prevalent issue of sexual disorders among CVD patients in Iran. The first recommendation was the development of culturally appropriate sexual health education programs. Motamedi et al. indicated that community-based health education tailored to Islamic values can significantly enhance health-seeking behaviors in Iran [29]. By family engagement and emphasizing cultural acceptability, these programs have the potential to diminish the stigma associated with sexual discussion in Iran. However, as highlighted by Samadi et al. [30], resistance by conservative communities may pose challenges to their implementation. Therefore, it is essential to initiate pilot programs and engage community leaders to facilitate acceptance and promote effective integration.
Training healthcare providers to deliver culturally appropriate sexual health counseling was another recommendation. Gadari et al. found that targeted training significantly enhances healthcare providers’ competency in addressing sensitive health topics in Iran, resulting in improved patient outcomes. Integrating this training into medical education curricula is essential for ensuring long-term effects; however, the investment in curriculum development resources is challenging, particularly in underfunded areas. Collaboration with academic institutions can help overcome this barrier [31].
Establishing gender-specific support groups through partnerships with NGOs, as another recommendation, can address gender-related stigma, a significant barrier identified by Firoozabadi et al. in their study of Iranian CVD patients [32]. These support groups create safe places for discussion; however, their scalability in rural areas may be constrained by cultural limitations and logistical challenges. The deployment of mobile clinics to improve access to sexual health services in rural areas was another recommendation. Motamedi et al. [29] demonstrated that mobile units can enhance health equity in Iran. However, the high operational costs and logistical difficulties necessitate funding from the government and the establishment of public-private partnerships.
Conclusion
This policy brief outlines a series of solutions aimed at addressing sexual disorders among CVD patients in Iran. Proposed solutions include culturally appropriate educational programs, training for healthcare providers, and the establishment of gender-specific support groups and mobile clinics. These solutions can mitigate cultural barriers, such as stigma and limited access to healthcare in rural areas, while prioritizing health equity and cultural acceptability. Although these solutions are backed by substantial evidence, their successful implementation depends on multi-sectoral collaboration and a phased approach to effectively navigate logistical challenges and cultural conservatism.
Limitations
This policy brief acknowledges several limitations. Only the English-language articles published from 2003 to 2021 were reviewed to determine the global prevalence of sexual dysfunction, potentially omitting relevant studies in Persian or those outside this timeframe. The reliance on secondary data from a systematic review study constrained the in-depth examination of specific local variables, such as ethnic differences in Iran. Moreover, while the proposed solutions, including mobile clinics and gender-specific support groups, are supported by evidence, their implementation may encounter challenges due to logistical barriers and cultural conservatism in rural areas. Finally, the lack of long-term data regarding the effectiveness of the proposed interventions in Iran limits the generalizability of the findings.
Recommendations
1) Monitor the health outcomes of CVD patients to assess the quality of care received in both outpatient and inpatient settings; 2) address the sexual dysfunction issues experienced by patients with CVDs, including decreased libido, sex difficulties, challenges with orgasm, ED, and ejaculatory difficulties; 3) careful selection of counselors: Their openness to learning and commitment to changing perspectives related to sexual dysfunction in CVD patients should be evaluated; 4) intensive induction training that includes perspective building, conceptual knowledge, and skill building related to sexuality and sexual health counseling; 5) provide a wide range of services related to sexual health and sexual dysfunction: They should be scientific, gender sensitive, and tailored to the specific needs of different groups (e.g. younger and older patients); 6) provide sexual health counseling services for CVD patients in hospitals and clinics; 7) interventional studies using integrated sexual health education and counseling for CVD patients; 8) interview all patients with CVDs who have traditional risk factors for sexual dysfunction; 9) inform patients about the risk factors of sexual dysfunction, such as depression, anxiety, and stress, and improve their quality of sexual relationships; 10) prioritize the assessment and treatment of sexual dysfunction; 11) integrating various methods, including self-reports, partner feedback, and clinical evaluations, to better understand a patient’s sexual dysfunction; 12) pay attention to the side effects of medications prescribed for CVDs, including beta-blockers and certain antidepressants, which can impair sexual function, reduce libido, and cause ED and difficulties in achieving orgasm; 13) further research in this field to understand whether sexual dysfunction is an early indicator or risk factor for CVDs, or if it is a complication of CVDs; 14) implement evidence-based policies and strategies to address sexual dysfunction and help alleviate the long-term health and economic challenges associated with sexual disorders; 15) study the prevalence of sexual dysfunction in other populations, such as people with diabetes, those undergoing hemodialysis, and cancer patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences, Kermanshah, Iran (Code: IR.KUMS.REC.1402.472).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The author declared no conflict of interest.
References
Cardiovascular diseases (CVDs), one of the leading causes of death, contribute to one-third of deaths globally [1]. In developing countries, the rate reaches 50% [2]. CVDs include ischemic heart disease, coronary heart disease, peripheral arterial disease, chronic hypertension, myocardial infarction, heart failure, and more cardiovascular conditions [3]. The CVD incidence increases for reasons such as having an unhealthy diet, smoking, having low or no physical activity, and exposure to excessive stress [4]. CVDs cause psychological and physical harms that reduce the patient’s quality of life (QoL) [1]. They can also cause sexual dysfunction, physically and mentally [5]. Patients with CVD have reported that their impaired sexual function has negatively affected their overall QoL [6]. Studies indicate that the prevalence of sexual dysfunction among CVD patients can be as high as 89% [2], which is three times greater than that observed in individuals without CVD [5]. Sexual dysfunction refers to difficulties in engaging in a satisfactory sexual activity among couples. Examples of sexual dysfunction include libido disorders, male erectile dysfunction (ED), female sexual arousal disorder, premature ejaculation, orgasm disorders in both males and females, and sexual pain conditions such as vaginismus and dyspareunia [6, 7]. The European Society of Urology defines ED as a persistent inability to attain and maintain an adequate erection for satisfactory sexual activity [6]. Patients with CVD often report symptoms of sexual dysfunction, which include a decrease in sexual desire, a tendency to avoid sexual activities, and feelings of sexual dissatisfaction [1]. Sexual dysfunction in patients with CVDs may result from physical, psychological, and medication-related factors [1, 2]. The physical and psychological effects of CVDs have proven to interfere with sexual activity, causing a reduction in patient QoL that comes from reduced self-esteem, depression, and isolation [8, 9]. Sexual dysfunction may predict CVD before other symptoms such as a cardiovascular event [10]. Patients with CVDs have sleep disorders 3-5 years prior to the emergence of other clinical signs of CVD. This timeframe may be leveraged in the future to implement therapeutic interventions aimed at addressing CVD risk factors at an earlier stage [8]. Epidemiological research indicates that both sexual dysfunction and CVDs are highly prevalent worldwide [1].
Despite its high prevalence, sexual dysfunction is often overlooked in care programs and health policies in Iran. The existing knowledge gap regarding the precise prevalence, contributing factors, and policies to enhance the condition of patients underscores the necessity of the present study. This study aims to determine the global prevalence of sexual dysfunction in patients with CVDs to inform policymakers, government health officials, and advisory organizations about the prevalence of sexual dysfunction in these patients. We also present solutions and policy recommendations to address the psychological and social implications of sexual dysfunction and help make informed decisions to enhance the QoL of CVD patients. Ultimately, this policy brief can serve as a valuable reference for designing clinical and policy interventions within the health system.
Materials and Methods
This research is a “policy brief” that utilizes data from a comprehensive 17-year systematic review and meta-analysis (2003–2023). Various databases, including Scientific Information Database (SID), Magiran, PubMed, Scopus, Web of Science (WOS) and Google Scholar databases, were searched to find the studies in English. The general search strategy was a follows: (Prevalence) OR (prevalence*) AND (“sexual dysfunctions, psychological”) OR (“disorders, sexual aversion”) OR (“orgasmic disorder”) AND (cardiac*) OR (“coronary artery bypass surgery”) OR (CABG) OR (“coronary artery bypass”) OR (“coronary artery bypass”) OR (cardiovascular*). The original research observational studies, including cross-sectional and cohort studies, that had available full texts and reported the prevalence of sexual disorders in patients with CVDs were included. The studies not relevant to the research objective, interventional studies (such as clinical trials and field trials), qualitative studies, case series, case reports, letters to the editor, conference proceedings, theses, and studies involving animal subjects were excluded from the review. The articles whose full texts were not accessible, even after contacting the corresponding authors, as well as duplicate studies, were also excluded. The initial search yielded 2,122 relevant studies. After removal of 792 duplicates and 1,006 studies by screening titles and abstracts, 324 full-text studies were assessed, of which 307 did not meet the inclusion criteria, resulting in 17 studies deemed suitable for the analysis [11-27].
Results
Figure 1 illustrates the prevalence of sexual dysfunction among CVD patients reported a meta-analysis of 17 studies conducted across various countries [28]. The findings indicate that the estimated global prevalence of sexual dysfunction among CVD patients is 62.6% (95% CI, 49.8%, 73.8%), revealing significant regional disparities. This underscores the need for targeted screening and culturally appropriate interventions and emphasizes the importance of region-specific health policies.
Cardiologists should be aware of the adverse effects of cardiac medications on sexual health. Knowing the side effects of prescribed medications on sexual function allows healthcare providers to take proactive measures to enhance patient health and QoL. Patients need to be adequately informed about the potential side effects of their prescribed medications, enabling them to make informed decisions regarding their treatment. Table 1 outlines the proposed solutions for enhancing sexual health in CVD patients based on the Iranian culture, accompanied by relevant recommendations and policy options.
These solutions are prioritized in Table 2, along with policy recommendations, detailing their strengths and weaknesses.
Discussion
The solutions and policy recommendations outlined in this policy brief seek to help address the prevalent issue of sexual disorders among CVD patients in Iran. The first recommendation was the development of culturally appropriate sexual health education programs. Motamedi et al. indicated that community-based health education tailored to Islamic values can significantly enhance health-seeking behaviors in Iran [29]. By family engagement and emphasizing cultural acceptability, these programs have the potential to diminish the stigma associated with sexual discussion in Iran. However, as highlighted by Samadi et al. [30], resistance by conservative communities may pose challenges to their implementation. Therefore, it is essential to initiate pilot programs and engage community leaders to facilitate acceptance and promote effective integration.
Training healthcare providers to deliver culturally appropriate sexual health counseling was another recommendation. Gadari et al. found that targeted training significantly enhances healthcare providers’ competency in addressing sensitive health topics in Iran, resulting in improved patient outcomes. Integrating this training into medical education curricula is essential for ensuring long-term effects; however, the investment in curriculum development resources is challenging, particularly in underfunded areas. Collaboration with academic institutions can help overcome this barrier [31].
Establishing gender-specific support groups through partnerships with NGOs, as another recommendation, can address gender-related stigma, a significant barrier identified by Firoozabadi et al. in their study of Iranian CVD patients [32]. These support groups create safe places for discussion; however, their scalability in rural areas may be constrained by cultural limitations and logistical challenges. The deployment of mobile clinics to improve access to sexual health services in rural areas was another recommendation. Motamedi et al. [29] demonstrated that mobile units can enhance health equity in Iran. However, the high operational costs and logistical difficulties necessitate funding from the government and the establishment of public-private partnerships.
Conclusion
This policy brief outlines a series of solutions aimed at addressing sexual disorders among CVD patients in Iran. Proposed solutions include culturally appropriate educational programs, training for healthcare providers, and the establishment of gender-specific support groups and mobile clinics. These solutions can mitigate cultural barriers, such as stigma and limited access to healthcare in rural areas, while prioritizing health equity and cultural acceptability. Although these solutions are backed by substantial evidence, their successful implementation depends on multi-sectoral collaboration and a phased approach to effectively navigate logistical challenges and cultural conservatism.
Limitations
This policy brief acknowledges several limitations. Only the English-language articles published from 2003 to 2021 were reviewed to determine the global prevalence of sexual dysfunction, potentially omitting relevant studies in Persian or those outside this timeframe. The reliance on secondary data from a systematic review study constrained the in-depth examination of specific local variables, such as ethnic differences in Iran. Moreover, while the proposed solutions, including mobile clinics and gender-specific support groups, are supported by evidence, their implementation may encounter challenges due to logistical barriers and cultural conservatism in rural areas. Finally, the lack of long-term data regarding the effectiveness of the proposed interventions in Iran limits the generalizability of the findings.
Recommendations
1) Monitor the health outcomes of CVD patients to assess the quality of care received in both outpatient and inpatient settings; 2) address the sexual dysfunction issues experienced by patients with CVDs, including decreased libido, sex difficulties, challenges with orgasm, ED, and ejaculatory difficulties; 3) careful selection of counselors: Their openness to learning and commitment to changing perspectives related to sexual dysfunction in CVD patients should be evaluated; 4) intensive induction training that includes perspective building, conceptual knowledge, and skill building related to sexuality and sexual health counseling; 5) provide a wide range of services related to sexual health and sexual dysfunction: They should be scientific, gender sensitive, and tailored to the specific needs of different groups (e.g. younger and older patients); 6) provide sexual health counseling services for CVD patients in hospitals and clinics; 7) interventional studies using integrated sexual health education and counseling for CVD patients; 8) interview all patients with CVDs who have traditional risk factors for sexual dysfunction; 9) inform patients about the risk factors of sexual dysfunction, such as depression, anxiety, and stress, and improve their quality of sexual relationships; 10) prioritize the assessment and treatment of sexual dysfunction; 11) integrating various methods, including self-reports, partner feedback, and clinical evaluations, to better understand a patient’s sexual dysfunction; 12) pay attention to the side effects of medications prescribed for CVDs, including beta-blockers and certain antidepressants, which can impair sexual function, reduce libido, and cause ED and difficulties in achieving orgasm; 13) further research in this field to understand whether sexual dysfunction is an early indicator or risk factor for CVDs, or if it is a complication of CVDs; 14) implement evidence-based policies and strategies to address sexual dysfunction and help alleviate the long-term health and economic challenges associated with sexual disorders; 15) study the prevalence of sexual dysfunction in other populations, such as people with diabetes, those undergoing hemodialysis, and cancer patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences, Kermanshah, Iran (Code: IR.KUMS.REC.1402.472).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The author declared no conflict of interest.
References
- Park JJ, Doo SW, Kwon A, Kim DK, Yang WJ, Song YS, et al. Effects of sexual rehabilitation on sexual dysfunction in patients with cardiovascular disease: A systematic review and meta-analysis. The World Journal of Men’s Health. 2023; 41(2):330-41. [DOI:10.5534/wjmh.220124] [PMID] [PMCID]
- Tirgari B, Rafati F, Mehdipour Rabori R. Effect of sexual rehabilitation program on anxiety, stress, depression, and sexual function among men with coronary artery disease. Journal of Sex & Marital Therapy. 2019; 45(7):632-42. [DOI:10.1080/0092623X.2019.1599091] [PMID]
- Rehan R, Kotchetkova I, Cordina R, Celermajer D. Adult congenital heart disease survivors at age 50 years: Medical and psychosocial status. Heart, Lung and Circulation. 2021; 30(2):261-6. [DOI:10.1016/j.hlc.2020.05.114] [PMID]
- World Health Organization (WHO). Cardiovascular diseases (CVDs) [Internet]. 2009 [Updated 2025 July 31]. Available from: [Link]
- Palm P, Zwisler AO, Svendsen JH, Thygesen LC, Giraldi A, Jensen KG, et al. Sexual rehabilitation for cardiac patients with erectile dysfunction: A randomised clinical trial. Heart. 2019; 105(10):775-82. [DOI:10.1136/heartjnl-2018-313778] [PMID]
- Irfan M, Hussain NHN, Noor NM, Mohamed M, Sidi H, Ismail SB. Epidemiology of male sexual dysfunction in Asian and European regions: A systematic review. American Journal of Men's Health. 2020; 14(4):1557988320937200. [DOI:10.1177/1557988320937200] [PMID] [PMCID]
- McCabe MP, Sharlip ID, Atalla E, Balon R, Fisher AD, Laumann E, et al. Definitions of sexual dysfunctions in women and men: A consensus statement from the fourth international consultation on sexual medicine 2015. The Journal of Sexual Medicine. 2016; 13(2):135-43. [DOI:10.1016/j.jsxm.2015.12.019] [PMID]
- Diaconu CC, Manea M, Marcu DR, Socea B, Spinu AD, Bratu OG. The erectile dysfunction as a marker of cardiovascular disease: A review. Acta Cardiologica. 2020; 75(4):286-92. [DOI:10.1080/00015385.2019.1590498] [PMID]
- Karami N, Kazeminia M, Karami A, Salimi Y, Ziapour A, Janjani P. Global prevalence of depression, anxiety, and stress in cardiac patients: A systematic review and meta-analysis. Journal of Affective Disorders. 2023; 324:175-89. [DOI:10.1016/j.jad.2022.12.055] [PMID]
- Johansen PP, Zwisler AD, Hastrup-Svendsen J, Frederiksen M, Lindschou J, Winkel P, et al. The copenheartsf trial--comprehensive sexual rehabilitation programme for male patients with implantable cardioverter defibrillator or ischaemic heart disease and impaired sexual function: Protocol of a randomised clinical trial. BMJ Open. 2013; 3(11):e003967. [DOI:10.1136/bmjopen-2013-003967] [PMID] [PMCID]
- Fafiolu AS, Adebayo AM, Akande TO, Akinboboye OO. Erectile dysfunction among male hypertensives in a tertiary health facility in South-West Nigeria. Global Journal of Health Science. 2014; 7(1):154-60. [DOI:10.5539/gjhs.v7n1p154] [PMID] [PMCID]
- Koh KC. Prevalence of erectile dysfunction in men with ischemic heart disease in a tertiary hospital in malaysia. The Medical Journal of Malaysia. 2013; 68(4):301-4. [PMID]
- Herbert K, Lopez B, Castellano J, Palacio A, Tamari L, Arcemen LM. The prevalence of erectile dysfunction in heart failure patients by race and ethnicity. International Journal of Impotence Research. 2008; 20(5):507-11. [DOI:10.1038/ijir.2008.35] [PMID]
- Oshodi OY, Adeyemi JD, Oke DA, Seedat S. Sexual dysfunction among subjects with hypertension in a Nigerian teaching hospital. Nigerian Quarterly Journal of Hospital Medicine. 2010; 20(4):197-204. [PMID]
- Heikkilä A, Kaipia A, Venermo M, Kautiainen H, Korhonen P. Relationship of blood pressure and erectile dysfunction in men without previously diagnosed hypertension. The Journal of Sexual Medicine. 2017; 14(11):1336-41. [DOI:10.1016/j.jsxm.2017.09.007] [PMID]
- Heruti RJ, Steinvil A, Shochat T, Saar N, Mashav N, Arbel Y, et al. Screening for erectile dysfunction and associated cardiovascular risk factors in Israeli men. The Israel Medical Association Journal. 2008; 10:686. [Link]
- Hood S, Robertson I. Erectile dysfunction: A significant health need in patients with coronary heart disease. Scottish Medical Journal. 2004; 49(3):97-8. [DOI:10.1177/003693300404900308] [PMID]
- Mittawae B, El-Nashaar AR, Fouda A, Magdy M, Shamloul R. Incidence of erectile dysfunction in 800 hypertensive patients: A multicenter Egyptian national study. Urology. 2006; 67(3):575-8. [DOI:10.1016/j.urology.2005.09.040] [PMID]
- Montorsi F, Briganti A, Salonia A, Rigatti P, Margonato A, Macchi A, et al. Erectile dysfunction prevalence, time of onset and association with risk factors in 300 consecutive patients with acute chest pain and angiographically documented coronary artery disease. European Urology. 2003; 44(3):360-4. [DOI:10.1016/s0302-2838(03)00305-1] [PMID]
- Mulat B, Arbel Y, Mashav N, Saar N, Steinvil A, Heruti R, et al. Depressive symptoms and erectile dysfunction in men with coronary artery disease. Urology. 2010; 75(1):104-7. [DOI:10.1016/j.urology.2009.09.041] [PMID]
- Neiman A, Ginde S, Earing MG, Bartz PJ, Cohen S. The prevalence of sexual dysfunction and its association with quality of life in adults with congenital heart disease. International Journal of Cardiology. 2017; 228:953-957. [DOI:10.1016/j.ijcard.2016.11.192] [PMID]
- Ramírez R, Pedro-Botet J, García M, Corbella E, Merino J, Zambón D, et al. Erectile dysfunction and cardiovascular risk factors in a Mediterranean diet cohort. Internal Medicine Journal. 2016; 46(1):52-6. [DOI:10.1111/imj.12937] [PMID]
- Rinkūnienė E, Gimžauskaitė S, Badarienė J, Dženkevičiūtė V, Kovaitė M, Čypienė A. The prevalence of erectile dysfunction and its association with cardiovascular risk factors in patients after myocardial infarction. Medicina. 2021; 57(10):1103.[DOI:10.3390/medicina57101103] [PMID] [PMCID]
- Roth A, Kalter-Leibovici O, Kerbis Y, Tenenbaum-Koren E, Chen J, Sobol T, Raz I. Prevalence and risk factors for erectile dysfunction in men with diabetes, hypertension, or both diseases: A community survey among 1,412 Israeli men. Clinical Cardiology. 2003; 26(1):25-30. [DOI:10.1002/clc.4960260106] [PMID] [PMCID]
- Rusiecki L, Zdrojowy R, Gebala J, Rabijewski M, Sobieszczańska M, Smoliński R, et al. Sexual health in Polish elderly men with coronary artery disease: importance, expectations, and reality. Asian Journal of Andrology. 2020; 22(5):526-31. [DOI:10.4103/aja.aja_131_19] [PMID] [PMCID]
- Schwarz ER, Kapur V, Bionat S, Rastogi S, Gupta R, Rosanio S. The prevalence and clinical relevance of sexual dysfunction in women and men with chronic heart failure. International Journal of Impotence Research. 2008; 20(1):85-91. [DOI:10.1038/sj.ijir.3901613] [PMID]
- Son YJ, Jang M, Jun EY. Prevalence of Erectile Dysfunction and Associated Factors in Korean Older Adults With Coronary Artery Disease. Journal of Gerontological Nursing. 2016; 42(10):32-41. [DOI:10.3928/00989134-20160701-02] [PMID]
- Ziapour A, Kazeminia M, Rouzbahani M, Bakhshi S, Montazeri N, Yıldırım M, et al. Global prevalence of sexual dysfunction in cardiovascular patients: A systematic review and meta-analysis. Systematic Reviews. 2024; 13(1):136. [DOI:10.1186/s13643-024-02525-0] [PMID] [PMCID]
- Motamedi M, Shahbazi M, Merghati-Khoei E, Salehi M, Hajebi A, Rahimi-Naghani S, et al. Perceived barriers to implementing sexual health programs from the viewpoint of health policymakers in Iran: A qualitative study. Sexuality Research and Social Policy. 2022; 19:273-85. [DOI:10.1007/s13178-021-00540-7]
- Samadi P, Alipour Z, Maasoumi R. Perceived barriers and needs in accessing sexual health services for iranian couples: A qualitative research. Iranian Journal of Nursing and Midwifery Research. 2023; 28(4):461-7. [DOI:10.4103/ijnmr.ijnmr_96_21] [PMID] [PMCID]
- Gadari S, Jouparinejad S, Noori Farsangi S, Sabzi A, Jafari A, Farokhzadian J. Cultural capacity, self-efficacy, and humility of healthcare providers: A survey in Southeast Iran. BMC Primary Care. 2025; 26(1):188. [DOI:10.1186/s12875-025-02898-8] [PMID] [PMCID]
- Firoozabadi MG, Mirzaei M, Grace SL, Vafaeinasab M, Dehghani-Tafti M, Sadeghi A, et al. Sex differences in cardiac rehabilitation barriers among non-enrollees in the context of lower gender equality: A cross-sectional study. BMC Cardiovascular Disorders. 2023; 23(1):329. [DOI:10.1186/s12872-023-03331-7] [PMID] [PMCID]
Type of Study: Other |
Subject:
Social Medicine
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |