Volume 11, Issue 1 (Winter 2023)
Iran J Health Sci 2023, 11(1): 67-74 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahgosha P, Hadinezhad P, Hosseini S H. Comparison of Brooding and Reflection Rumination Between People With Depression and Obsessive-compulsive Disorder. Iran J Health Sci 2023; 11 (1) :67-74
URL: http://jhs.mazums.ac.ir/article-1-823-en.html
URL: http://jhs.mazums.ac.ir/article-1-823-en.html
Department of Psychology, Faculty of Human Sciences, Bandargaz Branch, Islamic Azad University, Bandargaz, Iran. , pouria_rahgosha@yahoo.com
Keywords: Emotional regulation, Cognition, Negative thinking, Depression, Obsessive-compulsive disorder
Full-Text [PDF 679 kb]
(478 Downloads)
| Abstract (HTML) (1049 Views)
Full-Text: (282 Views)
1. Introduction
An increasing interest exists in the transdiagnostic trait of rumination. Rumination is defined as passive and persistent thinking about negative content, usually associated with attentional bias and causing emotional distress [1]. Rumination, as a maladaptive type of emotion-regulation strategy, is also recognized as a symptom in people with major depressive disorder (MDD) and its detrimental effects are high in this population. To name a few, previous studies confirmed that the severity of depression is directly associated with the intensity of rumination [2, 3, 4, 5]. In addition, rumination is regarded as a predictor of depression, and this conclusion is obtained given the harmful effects of rumination on healthy individuals’ moods. [6, 7]. In people with MDD, the detrimental effects of rumination extend to poor social problem-solving which is one of the most significant symptoms of people with depression and anxiety disorders [8, 9].
Although rumination is significantly found in depressed populations, people with obsessive-compulsive disorder (OCD) are also prone to rumination. In the context of OCD, rumination is a compulsion. A compulsion, by definition, is intended to reduce the distress caused by an unwanted, intrusive thought or obsession. Compulsions may help reduce distress in the short term but often help maintain OCD in the long term [10]. The situation is compounded by the adverse effects of rumination on the severity of OCD symptoms. People with OCD who adopt rumination as a regulatory strategy either ruminate about their symptoms or about their mood, which is mostly affected due to experiencing their OCD-related symptoms. In both cases, rumination enhances the severity of their symptoms and makes them more prone to depression [11]
Although in many studies rumination has been examined without any subtype, two subtypes of rumination exist. Specifically, rumination is divided into brooding and reflection rumination, which are different. Brooding rumination is conceptualized as inactive and judgmental cognition regarding one’s mood. Conversely, reflection refers to a conscious inward focus that engages in cognitive problem-solving and intends to gain insight into one’s depressive symptoms [12].
Brooding rumination is more common among people with mood and anxiety disorders and usually has more detrimental effects on cognition, especially on memory [13]. This subtype of rumination influences working memory capacity and jeopardizes episodic memory recall since it influences inhibitory control. People with brooding usually have difficulty inhibiting irrelevant information during episodic memory recall, which in turn leads to the accumulation of information in working memory and makes retrieval problematic [14]. Since brooding is a tendency to focus on negative aspects of oneself or negative interpretations of life, implementing emotion regulation strategies, such as cognitive reappraisals which can alter the emotional valence of the events and assist people to cope with their problematic symptoms may be more difficult for people prone to brooding.
Unlike brooding, reflection engages cognitive mechanisms actively and purposefully. Imagine a situation when you made a mistake at work that led to some conflicts between you and your colleagues and then, you are trying to figure out whether the mistake was on your part or on the part of your colleagues. Even after figuring out this issue, you still seek solutions to tackle conflicts. This is exactly what reflection looks like. In other words, reflection is activated to gain insight, learn, and ultimately self-improvement [15].
Notwithstanding the difference between brooding and reflection, most investigations on many clinical groups have only examined rumination without elaborating on its subtypes. Numerous studies investigated rumination in individuals with anxiety disorders [10, 16, 17]. However, only a few studies discriminated between brooding and reflection rumination in these clinical populations. In addition, few studies examined rumination in people with OCD. In addition to these limitations in the literature, another limitation, to our knowledge, is that the comparison of brooding and reflection rumination between people with OCD and MDD has not yet been conducted. People with MDD and OCD have many overlaps in symptoms. Also, they often occur as a comorbid disorder. Nonetheless, a comparison of rumination, a common symptom, has not been precisely examined between these groups.
Addressing these limitations of the literature is crucial for treatment purposes. Brooding and reflections are predictors of different cognitive distortions and often conventional psychological treatments, such as cognitive behavioral therapy (CBT) center on addressing these cognitive distortions. In therapy sessions, patients’ resistance to adopting alternative perspectives and working on their cognitive distortions is more easily overcome if the clinician targets underlying mechanisms for this resistance-in this case, ruminative thoughts. As discussed earlier, brooding and reflection are different which means they should be treated using different strategies. This is exactly why there is a need to differentiate these subtypes of rumination in clinical groups, especially in clinical disorders that often occur as comorbid disorders. Without accurately determining the dominant subtype of rumination in each clinical disorder, and instead working on rumination can only waste the patient’s time and money and discourage them from proceeding with their therapy sessions.
Therefore we aim to compare brooding and reflection rumination in people with MDD and OCD. Conducting this paper can be of paramount importance since the results of this study can assist therapists to recognize rumination in these populations more efficiently and methodically. In light of our results, they can target and confront brooding and reflection rumination as a part of the therapy plan.
2. Materials and Methods
The statistical society included patients referred to a health clinic in Sari City, Iran (the capital of Mazandaran Province, Northern Iran), and our samples were determined by convenience sampling method. Patients aged 20 to 45 years who met the inclusion criteria of the diagnostic and statistical manual of mental disorders, fifth edition, for one of the relevant diagnoses were screened for inclusion during a certain period. Inclusion criteria were people with OCD and MDD and people aged between 20 and 45 years. The exclusion criteria included people with comorbidity, people younger than 20 or older than 45, people without a personality disorder, people without substance use, and people who did not agree to participate. A total of 50 and 45 patients met the MDD and OCD diagnostic criteria, respectively. For diagnosis purposes, two clinicians, a psychiatrist and a psychologist examined the patients and used the structured clinical interviews, the Yale-Brown obsessive-compulsive scale, and the second version of the Beck Depression Inventory (BDI) for diagnosis. Participants were solely recruited after precise diagnosis, then, interviewed in a specialized clinic in Sari City according to mentioned inclusion and exclusion criteria. This process was conducted for three months. All participants were informed and agreed to participate in the study, expecting no deal.
Yale-Brown Obsessive Compulsive Scale
For OCD diagnosis, we applied Yale-Brown Obsessive Compulsive Scale, devised in 1986. This is a semi-structured interview used to diagnose OCD and its severity. Any score above 8 indicates OCD and people who score between 30 and 40 suffer from severe OCD. The reliability of the test in Iran is reported between 0.69 and 0.91 which represents decent reliability. The validity is also reported as 0.58 [18].
The second version of the BDI
We also used the second version of the BDI, developed by Aaron T. Beck, to diagnose MDD. This scale is a self-report questionnaire that consists of 21 items and allows one to recognize the severity of depression in adults. In the questionnaire, items are measured on a 4-point Likert scale from low to intensive. Regarding previous studies, the questionnaire has decent validity, which makes it a reliable tool to evaluate depression in adults. Various studies have been conducted in the country that measured the psychometric properties of this tool. For instance, in Chegini’s research, the reliability coefficient of the questionnaire was estimated to be 0.90 through Cronbach’s alpha [19].
The Ruminative Response Scale (RRS)
The Ruminative Response Scale (RRS), a self-report scale to describe one’s response to a depressed mood, consists of 22 items and three factors (depression, brooding, and reflection). Each item is rated on a 4-point Likert scale ranging from 1 (never) to 4 (always). The total score ranges from 22 to 88, with higher scores indicating higher degrees of ruminative symptoms. Applying this scale enabled us to discriminate between brooding and reflection rumination. psychometric properties of this scale were measured in Iran and the validity of brooding and reflection were reported 0.79 and 0.69, respectively [20].
Our questionnaires were fully answered and no data was missed, which in turn enabled us to include the entire samples in the data analysis stage.
3. Results
In the first step, we calculated demographic information based on the demographic questionnaire that we distributed to the participants. These demographic data included the age, gender, and literacy status of the participants. Demographic information is presented in Table 1.

Then, we determined descriptive statistics of the research, including mean, standard deviation, and standard error of mean. Table 2 presents descriptive statistics for both brooding and reflection in two groups.
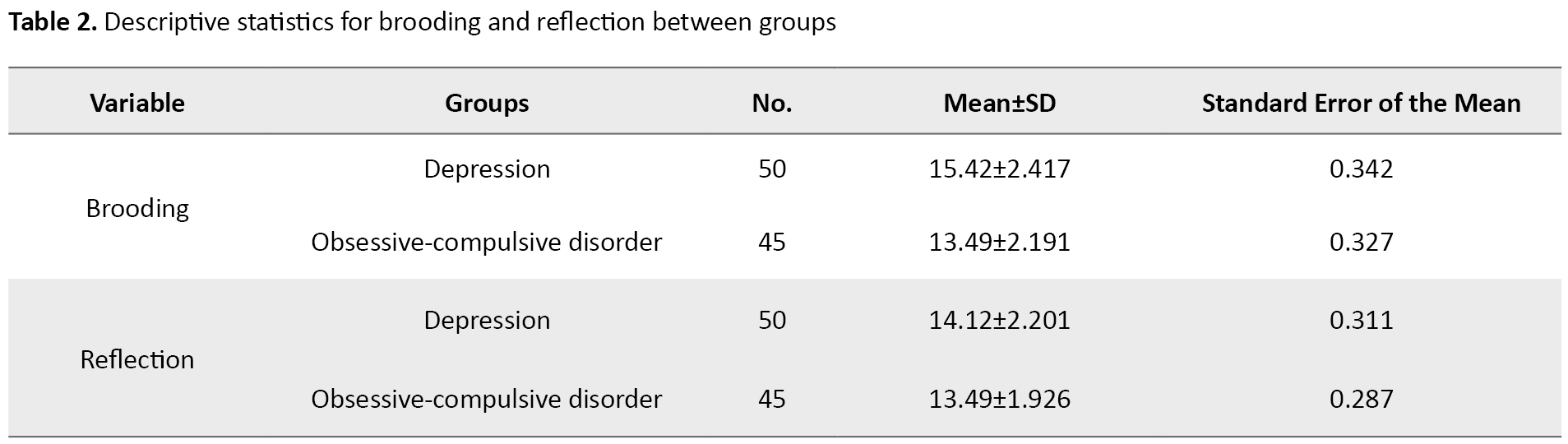
Scores obtained on the RRS scale reveals a mean difference in brooding score for the two groups. As seen in Table 2, individuals with MDD had a higher mean (M=15.42) compared to the group of people with OCD (M=13.49). The scores for reflection rumination also show the mean difference between groups. Similar to the brooding scores, people who suffered from MDD had a higher mean (M=14.12) compared to the individuals with OCD (13.49). Considering these figures, people with MDD showed more intense rumination regardless of its type.
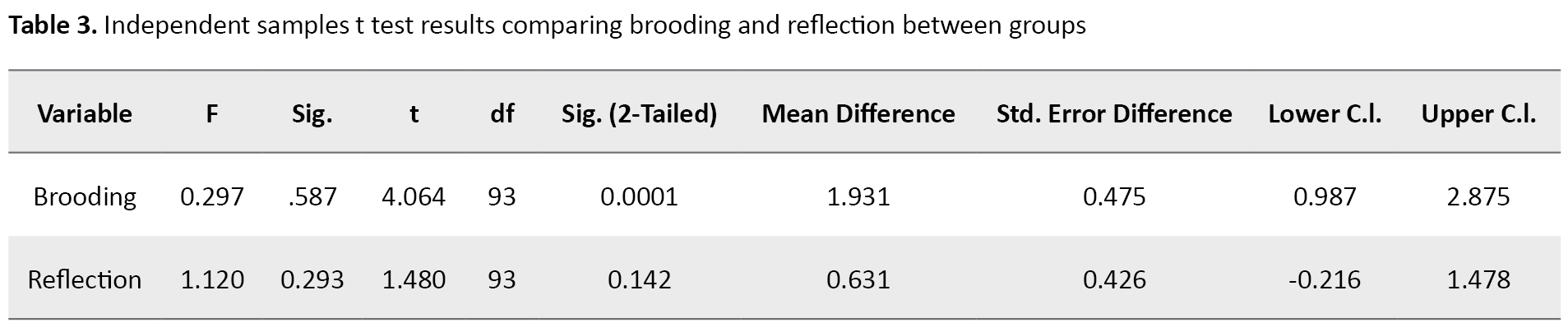
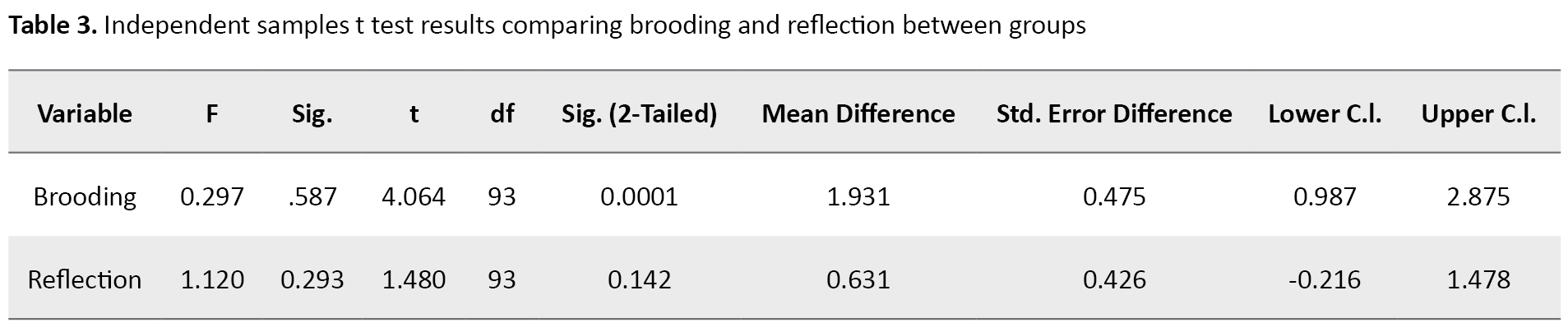
Independent samples t tests were conducted to determine whether people with MDD and OCD scored differently on brooding and reflection. According to t test, the groups performed differently in brooding rumination, t(93)=4.06, P=0.000, 95% CI: 0.987, 2.875. The mean of brooding rumination for the MDD group (M=15.42, SD=2.41) was significantly different from the OCD group (M=13.49, SD=2.19). These findings support the idea that a significant difference is observed in brooding rumination between the groups. We also conducted the same t test to determine whether people with MDD and OCD scored differently on reflection. However, in this test, the groups did not differ significantly, t(93)=1.48, P=0.14, 95% CI: -0.216, 1.478. The mean of the reflection rumination for the MDD group (M=14.12, SD=2.20) was not significantly different from the OCD group (M=13.49, SD=1.92). These findings do not support the idea that a difference is observed in reflection rumination between the MDD group and the OCD group. Table 3 demonstrates the inferential statistics of the research.
4. Discussion
This paper compared brooding and reflection rumination between individuals with MDD and OCD. According to the result of the study, the groups differed in brooding rumination. People with MDD had a higher mean meaning that these individuals show more intense brooding rumination. This result is consistent with several studies showing brooding rumination in individuals with MDD [21, 22, 23, 24]. The higher level of brooding rumination in people with MDD can lead to the persistence of their depressive symptoms by influencing attentional control. One study showed that clinically and non-clinically depressed people with high levels of brooding rumination show more sustained attention to sad faces compared to happy faces [25]. These results indicate a bias in the information processing of depressed populations by prioritizing the information related to depression. The detrimental effects of brooding on the persistency and severity of depression can be more pronounced by considering the results of a study that recognized brooding, but not reflection, as a predictor of the increases in depressive symptoms over time [26]. Aside from the psychological and cognitive effects of brooding, this subtype of rumination leads to physiological changes as well. Indeed, the sustained cognitive representation and anticipation of stressful events trigger a cascade of biological reactions that affect various functions from the brain to the autonomic nervous system. In this regard, one study determined that brooding can predict depression and heart rate is a mediator in this relationship. In this study, people with higher levels of brooding showed faster heart rates and subsequently higher levels of depression [27]. The physiological effects of brooding have also been demonstrated by a study showing that brooding influences cardiovascular reactivity to a laboratory-based stressor. The study indicated a direct relationship between levels of brooding and heart rate variability [28]. Depression and rumination are typically observed as symbiotic relationships. On the one hand, the cumulative effects of numerous depressive symptoms can result in higher levels of brooding in depressed populations compared to people with OCD. These determinants can be influential in both direct and indirect ways. For instance, the passive lifestyle that people with MDD adopt prevents them from pursuing goals and daily activities that give them a sense of accomplishment. This, in turn, can damage the self-esteem in these populations. Studies indicated that the levels of self-esteem predict the levels of brooding rumination [29]. On the other hand, the different levels of brooding between individuals with MDD and OCD can represent the fact that people with mood disorders are more prone to negative interpretations of their quality and life since the essence of brooding is to limit one’s mental capacity to passive thinking. This passive way of thinking and negative interpretation of one’s characteristics can cause a lower mood, which in turn enhances the level of depressive symptoms. Brain dysfunctions associated with rumination overlap with those found in depression at the neural level. For example, studies described patterns of decreased resting-state functional connectivity between prefrontal areas and the amygdala, suggesting weakened prefrontal inhibitory control over subcortical affective structures in rumination [30, 31]. This inseparable association between brooding and depression can account for diverse representation in many cognitive functions between MDD and OCD populations. For instance, the difference in the levels of brooding rumination may be the underlying mechanism for diverse qualities in problem-solving abilities between the group of people with MDD and anxiety disorders. Different stages of problem-solving exist and these two clinical groups have shown difficulties at different stages. One difficulty in problem-solving is the lack of access to potential solutions for problems. Individuals with MDD have trouble at this stage. Problem-solving disability also occurs as a result of failure to choose the most efficient strategy for addressing problems. This is a frequent challenge for people with anxiety disorders [32]. One possible reason for the first scenario, when potential solutions are out of reach, is that brooding can deter people with MDD from seeking ways to cope with problems since brooding depletes attentional resources and shifts them toward misinterpretation of self-qualities rather than encouraging people to become active and have a positive attitude regarding themselves. Furthermore, brooding leads to over generality of memories [12]. Exploring past events and applying experiences can assist people to find potential solutions to problems. By this reasoning, people with MDD fail to benefit from their experience and are more prone to problem-solving disabilities.
Apart from the results of the brooding test, the study groups did not show any difference in reflection. Mean reflection scores were almost the same, meaning that people with MDD and OCD tended to reflect at the same level. Previous studies determined that people with depressive and anxiety symptoms use less adaptive emotion regulation strategies and are more prone to maladaptive regulation strategies [33]. In a study, people with MDD were instructed to apply different regulatory strategies, including brooding, reflection, expressive suppression, and cognitive reappraisal. The study results showed that reflection predicts recovery from MDD episodes [34]. In another study, the mediating role of brooding and reflection in the relationship between negative affectivity and depression and anxiety was measured. The results indicated that in the group of people with depression, both brooding and reflection significantly mediated the relationship. Conversely, in the group of people with anxiety, neither brooding nor reflection mediated the relationship between negative affectivity and anxiety [35]. All these findings, with our results, justify the same levels of brooding and reflection between people with MDD and OCD. Future studies can determine how healthy populations differ in reflection with these two groups. By addressing this difference, future results, by relying on our results, can confront a misconception that rumination is common in many mental illnesses, including depression regardless of its subtypes. People with MDD mostly adopt passive regulatory strategies instead of using cognitive demanding strategies, such as reflection and cognitive reappraisal. This can indicate why we found the same level of reflection, while a significant difference was observed in brooding between the two groups.
To sum up, we clarified the difference between these two clinical populations in terms of rumination subtypes. However, this difference remains in question among other mental illnesses. Therefore, we encourage other researchers to investigate brooding and reflection on various mental illnesses. These studies will prove effective and will be very helpful in the clinical context. Rumination is one of the most significant symptoms of several mental illnesses. Thus, any study on rumination can enable clinical psychologists to address rumination more efficiently and have a better therapy plan. Several emotion regulation techniques can be applied instead of rumination. However, their use requires education about the detrimental effects of rumination and the probability of replacing efficient information-processing approaches. As a part of therapeutic interventions, emotion regulation strategies, such as cognitive reappraisal can be taught to people prone to rumination. Reinterpretation and cognitive distancing, as two reappraisal techniques, enable people with rumination to experience an active implementation of cognitive resources to re-interpret events, which in turn reduces ruminations over time.
Due to the COVID-19 pandemic, access to samples was limited. Some of the people whom we interviewed were reluctant to participate in the study and spend extra time at the health center due to COVID-19. This limitation prevented us from conducting our study with our desired sample size.
5. Conclusion
The results of this study indicate that depressed people are susceptible to higher levels of rumination as a whole. Although this difference is significant when rumination is considered as a single unit, studying the subtypes of rumination shines a light on the prevalence of brooding and reflection rumination and determines that this significant difference is confined to brooding rumination. People with MDD and OCD performed almost the same in the reflection test. These results justify why depressed people are more prone to low mood compared with people with OCD given that brooding contributes to low mood to a greater extent. Considering our results, clinicians are recommended to pay close attention to the prevalence of brooding and reflection in people with MDD and OCD. This will enable them to make more efficient therapeutic plans specific to each mental illness.
Ethical Considerations
Compliance with ethical guidelines
The approval of the Ethics Committee was obtained from the Mazandaran University of Medical Science (IR.MAZUMS..REC.1401.9319). We received informed consent from the participants by providing necessary information regarding the goals and the structure of the study.
Funding
No funding was received for the current study.
Authors contributions
Writing the paper, data analysis, studying the literature, idea development: Pouria Rahgosha; Data collection: Parmida Hadinezhad; Supervisory role, editing: Seyed Hamzeh Hosseini.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate all participants in the study. In addition, we are grateful to Professor Seyed Hamzeh Hosseini for providing a suitable environment for conducting research for all participants.
References
An increasing interest exists in the transdiagnostic trait of rumination. Rumination is defined as passive and persistent thinking about negative content, usually associated with attentional bias and causing emotional distress [1]. Rumination, as a maladaptive type of emotion-regulation strategy, is also recognized as a symptom in people with major depressive disorder (MDD) and its detrimental effects are high in this population. To name a few, previous studies confirmed that the severity of depression is directly associated with the intensity of rumination [2, 3, 4, 5]. In addition, rumination is regarded as a predictor of depression, and this conclusion is obtained given the harmful effects of rumination on healthy individuals’ moods. [6, 7]. In people with MDD, the detrimental effects of rumination extend to poor social problem-solving which is one of the most significant symptoms of people with depression and anxiety disorders [8, 9].
Although rumination is significantly found in depressed populations, people with obsessive-compulsive disorder (OCD) are also prone to rumination. In the context of OCD, rumination is a compulsion. A compulsion, by definition, is intended to reduce the distress caused by an unwanted, intrusive thought or obsession. Compulsions may help reduce distress in the short term but often help maintain OCD in the long term [10]. The situation is compounded by the adverse effects of rumination on the severity of OCD symptoms. People with OCD who adopt rumination as a regulatory strategy either ruminate about their symptoms or about their mood, which is mostly affected due to experiencing their OCD-related symptoms. In both cases, rumination enhances the severity of their symptoms and makes them more prone to depression [11]
Although in many studies rumination has been examined without any subtype, two subtypes of rumination exist. Specifically, rumination is divided into brooding and reflection rumination, which are different. Brooding rumination is conceptualized as inactive and judgmental cognition regarding one’s mood. Conversely, reflection refers to a conscious inward focus that engages in cognitive problem-solving and intends to gain insight into one’s depressive symptoms [12].
Brooding rumination is more common among people with mood and anxiety disorders and usually has more detrimental effects on cognition, especially on memory [13]. This subtype of rumination influences working memory capacity and jeopardizes episodic memory recall since it influences inhibitory control. People with brooding usually have difficulty inhibiting irrelevant information during episodic memory recall, which in turn leads to the accumulation of information in working memory and makes retrieval problematic [14]. Since brooding is a tendency to focus on negative aspects of oneself or negative interpretations of life, implementing emotion regulation strategies, such as cognitive reappraisals which can alter the emotional valence of the events and assist people to cope with their problematic symptoms may be more difficult for people prone to brooding.
Unlike brooding, reflection engages cognitive mechanisms actively and purposefully. Imagine a situation when you made a mistake at work that led to some conflicts between you and your colleagues and then, you are trying to figure out whether the mistake was on your part or on the part of your colleagues. Even after figuring out this issue, you still seek solutions to tackle conflicts. This is exactly what reflection looks like. In other words, reflection is activated to gain insight, learn, and ultimately self-improvement [15].
Notwithstanding the difference between brooding and reflection, most investigations on many clinical groups have only examined rumination without elaborating on its subtypes. Numerous studies investigated rumination in individuals with anxiety disorders [10, 16, 17]. However, only a few studies discriminated between brooding and reflection rumination in these clinical populations. In addition, few studies examined rumination in people with OCD. In addition to these limitations in the literature, another limitation, to our knowledge, is that the comparison of brooding and reflection rumination between people with OCD and MDD has not yet been conducted. People with MDD and OCD have many overlaps in symptoms. Also, they often occur as a comorbid disorder. Nonetheless, a comparison of rumination, a common symptom, has not been precisely examined between these groups.
Addressing these limitations of the literature is crucial for treatment purposes. Brooding and reflections are predictors of different cognitive distortions and often conventional psychological treatments, such as cognitive behavioral therapy (CBT) center on addressing these cognitive distortions. In therapy sessions, patients’ resistance to adopting alternative perspectives and working on their cognitive distortions is more easily overcome if the clinician targets underlying mechanisms for this resistance-in this case, ruminative thoughts. As discussed earlier, brooding and reflection are different which means they should be treated using different strategies. This is exactly why there is a need to differentiate these subtypes of rumination in clinical groups, especially in clinical disorders that often occur as comorbid disorders. Without accurately determining the dominant subtype of rumination in each clinical disorder, and instead working on rumination can only waste the patient’s time and money and discourage them from proceeding with their therapy sessions.
Therefore we aim to compare brooding and reflection rumination in people with MDD and OCD. Conducting this paper can be of paramount importance since the results of this study can assist therapists to recognize rumination in these populations more efficiently and methodically. In light of our results, they can target and confront brooding and reflection rumination as a part of the therapy plan.
2. Materials and Methods
The statistical society included patients referred to a health clinic in Sari City, Iran (the capital of Mazandaran Province, Northern Iran), and our samples were determined by convenience sampling method. Patients aged 20 to 45 years who met the inclusion criteria of the diagnostic and statistical manual of mental disorders, fifth edition, for one of the relevant diagnoses were screened for inclusion during a certain period. Inclusion criteria were people with OCD and MDD and people aged between 20 and 45 years. The exclusion criteria included people with comorbidity, people younger than 20 or older than 45, people without a personality disorder, people without substance use, and people who did not agree to participate. A total of 50 and 45 patients met the MDD and OCD diagnostic criteria, respectively. For diagnosis purposes, two clinicians, a psychiatrist and a psychologist examined the patients and used the structured clinical interviews, the Yale-Brown obsessive-compulsive scale, and the second version of the Beck Depression Inventory (BDI) for diagnosis. Participants were solely recruited after precise diagnosis, then, interviewed in a specialized clinic in Sari City according to mentioned inclusion and exclusion criteria. This process was conducted for three months. All participants were informed and agreed to participate in the study, expecting no deal.
Yale-Brown Obsessive Compulsive Scale
For OCD diagnosis, we applied Yale-Brown Obsessive Compulsive Scale, devised in 1986. This is a semi-structured interview used to diagnose OCD and its severity. Any score above 8 indicates OCD and people who score between 30 and 40 suffer from severe OCD. The reliability of the test in Iran is reported between 0.69 and 0.91 which represents decent reliability. The validity is also reported as 0.58 [18].
The second version of the BDI
We also used the second version of the BDI, developed by Aaron T. Beck, to diagnose MDD. This scale is a self-report questionnaire that consists of 21 items and allows one to recognize the severity of depression in adults. In the questionnaire, items are measured on a 4-point Likert scale from low to intensive. Regarding previous studies, the questionnaire has decent validity, which makes it a reliable tool to evaluate depression in adults. Various studies have been conducted in the country that measured the psychometric properties of this tool. For instance, in Chegini’s research, the reliability coefficient of the questionnaire was estimated to be 0.90 through Cronbach’s alpha [19].
The Ruminative Response Scale (RRS)
The Ruminative Response Scale (RRS), a self-report scale to describe one’s response to a depressed mood, consists of 22 items and three factors (depression, brooding, and reflection). Each item is rated on a 4-point Likert scale ranging from 1 (never) to 4 (always). The total score ranges from 22 to 88, with higher scores indicating higher degrees of ruminative symptoms. Applying this scale enabled us to discriminate between brooding and reflection rumination. psychometric properties of this scale were measured in Iran and the validity of brooding and reflection were reported 0.79 and 0.69, respectively [20].
Our questionnaires were fully answered and no data was missed, which in turn enabled us to include the entire samples in the data analysis stage.
3. Results
In the first step, we calculated demographic information based on the demographic questionnaire that we distributed to the participants. These demographic data included the age, gender, and literacy status of the participants. Demographic information is presented in Table 1.

Then, we determined descriptive statistics of the research, including mean, standard deviation, and standard error of mean. Table 2 presents descriptive statistics for both brooding and reflection in two groups.
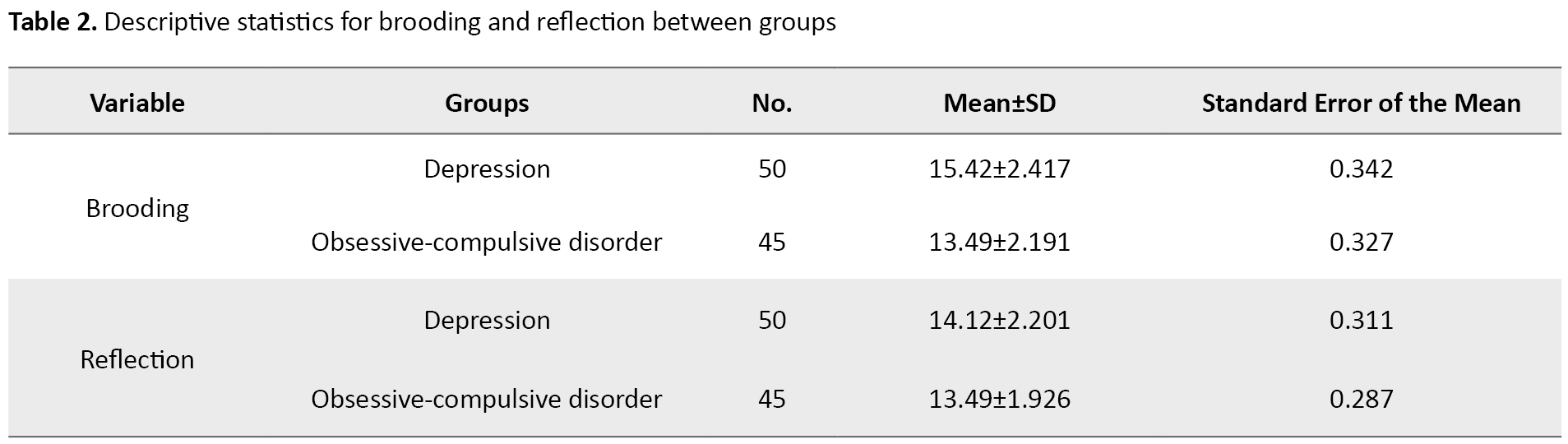
Scores obtained on the RRS scale reveals a mean difference in brooding score for the two groups. As seen in Table 2, individuals with MDD had a higher mean (M=15.42) compared to the group of people with OCD (M=13.49). The scores for reflection rumination also show the mean difference between groups. Similar to the brooding scores, people who suffered from MDD had a higher mean (M=14.12) compared to the individuals with OCD (13.49). Considering these figures, people with MDD showed more intense rumination regardless of its type.
Independent samples t tests were conducted to determine whether people with MDD and OCD scored differently on brooding and reflection. According to t test, the groups performed differently in brooding rumination, t(93)=4.06, P=0.000, 95% CI: 0.987, 2.875. The mean of brooding rumination for the MDD group (M=15.42, SD=2.41) was significantly different from the OCD group (M=13.49, SD=2.19). These findings support the idea that a significant difference is observed in brooding rumination between the groups. We also conducted the same t test to determine whether people with MDD and OCD scored differently on reflection. However, in this test, the groups did not differ significantly, t(93)=1.48, P=0.14, 95% CI: -0.216, 1.478. The mean of the reflection rumination for the MDD group (M=14.12, SD=2.20) was not significantly different from the OCD group (M=13.49, SD=1.92). These findings do not support the idea that a difference is observed in reflection rumination between the MDD group and the OCD group. Table 3 demonstrates the inferential statistics of the research.
4. Discussion
This paper compared brooding and reflection rumination between individuals with MDD and OCD. According to the result of the study, the groups differed in brooding rumination. People with MDD had a higher mean meaning that these individuals show more intense brooding rumination. This result is consistent with several studies showing brooding rumination in individuals with MDD [21, 22, 23, 24]. The higher level of brooding rumination in people with MDD can lead to the persistence of their depressive symptoms by influencing attentional control. One study showed that clinically and non-clinically depressed people with high levels of brooding rumination show more sustained attention to sad faces compared to happy faces [25]. These results indicate a bias in the information processing of depressed populations by prioritizing the information related to depression. The detrimental effects of brooding on the persistency and severity of depression can be more pronounced by considering the results of a study that recognized brooding, but not reflection, as a predictor of the increases in depressive symptoms over time [26]. Aside from the psychological and cognitive effects of brooding, this subtype of rumination leads to physiological changes as well. Indeed, the sustained cognitive representation and anticipation of stressful events trigger a cascade of biological reactions that affect various functions from the brain to the autonomic nervous system. In this regard, one study determined that brooding can predict depression and heart rate is a mediator in this relationship. In this study, people with higher levels of brooding showed faster heart rates and subsequently higher levels of depression [27]. The physiological effects of brooding have also been demonstrated by a study showing that brooding influences cardiovascular reactivity to a laboratory-based stressor. The study indicated a direct relationship between levels of brooding and heart rate variability [28]. Depression and rumination are typically observed as symbiotic relationships. On the one hand, the cumulative effects of numerous depressive symptoms can result in higher levels of brooding in depressed populations compared to people with OCD. These determinants can be influential in both direct and indirect ways. For instance, the passive lifestyle that people with MDD adopt prevents them from pursuing goals and daily activities that give them a sense of accomplishment. This, in turn, can damage the self-esteem in these populations. Studies indicated that the levels of self-esteem predict the levels of brooding rumination [29]. On the other hand, the different levels of brooding between individuals with MDD and OCD can represent the fact that people with mood disorders are more prone to negative interpretations of their quality and life since the essence of brooding is to limit one’s mental capacity to passive thinking. This passive way of thinking and negative interpretation of one’s characteristics can cause a lower mood, which in turn enhances the level of depressive symptoms. Brain dysfunctions associated with rumination overlap with those found in depression at the neural level. For example, studies described patterns of decreased resting-state functional connectivity between prefrontal areas and the amygdala, suggesting weakened prefrontal inhibitory control over subcortical affective structures in rumination [30, 31]. This inseparable association between brooding and depression can account for diverse representation in many cognitive functions between MDD and OCD populations. For instance, the difference in the levels of brooding rumination may be the underlying mechanism for diverse qualities in problem-solving abilities between the group of people with MDD and anxiety disorders. Different stages of problem-solving exist and these two clinical groups have shown difficulties at different stages. One difficulty in problem-solving is the lack of access to potential solutions for problems. Individuals with MDD have trouble at this stage. Problem-solving disability also occurs as a result of failure to choose the most efficient strategy for addressing problems. This is a frequent challenge for people with anxiety disorders [32]. One possible reason for the first scenario, when potential solutions are out of reach, is that brooding can deter people with MDD from seeking ways to cope with problems since brooding depletes attentional resources and shifts them toward misinterpretation of self-qualities rather than encouraging people to become active and have a positive attitude regarding themselves. Furthermore, brooding leads to over generality of memories [12]. Exploring past events and applying experiences can assist people to find potential solutions to problems. By this reasoning, people with MDD fail to benefit from their experience and are more prone to problem-solving disabilities.
Apart from the results of the brooding test, the study groups did not show any difference in reflection. Mean reflection scores were almost the same, meaning that people with MDD and OCD tended to reflect at the same level. Previous studies determined that people with depressive and anxiety symptoms use less adaptive emotion regulation strategies and are more prone to maladaptive regulation strategies [33]. In a study, people with MDD were instructed to apply different regulatory strategies, including brooding, reflection, expressive suppression, and cognitive reappraisal. The study results showed that reflection predicts recovery from MDD episodes [34]. In another study, the mediating role of brooding and reflection in the relationship between negative affectivity and depression and anxiety was measured. The results indicated that in the group of people with depression, both brooding and reflection significantly mediated the relationship. Conversely, in the group of people with anxiety, neither brooding nor reflection mediated the relationship between negative affectivity and anxiety [35]. All these findings, with our results, justify the same levels of brooding and reflection between people with MDD and OCD. Future studies can determine how healthy populations differ in reflection with these two groups. By addressing this difference, future results, by relying on our results, can confront a misconception that rumination is common in many mental illnesses, including depression regardless of its subtypes. People with MDD mostly adopt passive regulatory strategies instead of using cognitive demanding strategies, such as reflection and cognitive reappraisal. This can indicate why we found the same level of reflection, while a significant difference was observed in brooding between the two groups.
To sum up, we clarified the difference between these two clinical populations in terms of rumination subtypes. However, this difference remains in question among other mental illnesses. Therefore, we encourage other researchers to investigate brooding and reflection on various mental illnesses. These studies will prove effective and will be very helpful in the clinical context. Rumination is one of the most significant symptoms of several mental illnesses. Thus, any study on rumination can enable clinical psychologists to address rumination more efficiently and have a better therapy plan. Several emotion regulation techniques can be applied instead of rumination. However, their use requires education about the detrimental effects of rumination and the probability of replacing efficient information-processing approaches. As a part of therapeutic interventions, emotion regulation strategies, such as cognitive reappraisal can be taught to people prone to rumination. Reinterpretation and cognitive distancing, as two reappraisal techniques, enable people with rumination to experience an active implementation of cognitive resources to re-interpret events, which in turn reduces ruminations over time.
Due to the COVID-19 pandemic, access to samples was limited. Some of the people whom we interviewed were reluctant to participate in the study and spend extra time at the health center due to COVID-19. This limitation prevented us from conducting our study with our desired sample size.
5. Conclusion
The results of this study indicate that depressed people are susceptible to higher levels of rumination as a whole. Although this difference is significant when rumination is considered as a single unit, studying the subtypes of rumination shines a light on the prevalence of brooding and reflection rumination and determines that this significant difference is confined to brooding rumination. People with MDD and OCD performed almost the same in the reflection test. These results justify why depressed people are more prone to low mood compared with people with OCD given that brooding contributes to low mood to a greater extent. Considering our results, clinicians are recommended to pay close attention to the prevalence of brooding and reflection in people with MDD and OCD. This will enable them to make more efficient therapeutic plans specific to each mental illness.
Ethical Considerations
Compliance with ethical guidelines
The approval of the Ethics Committee was obtained from the Mazandaran University of Medical Science (IR.MAZUMS..REC.1401.9319). We received informed consent from the participants by providing necessary information regarding the goals and the structure of the study.
Funding
No funding was received for the current study.
Authors contributions
Writing the paper, data analysis, studying the literature, idea development: Pouria Rahgosha; Data collection: Parmida Hadinezhad; Supervisory role, editing: Seyed Hamzeh Hosseini.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate all participants in the study. In addition, we are grateful to Professor Seyed Hamzeh Hosseini for providing a suitable environment for conducting research for all participants.
References
- Sansone RA, Sansone LA. Rumination: relationships with physical health. Innovations in Clinical Neuroscience. 2012; 9(2):29-34. [PMCID]
- Zhou HX, Chen X, Shen YQ, Li L, Chen NX, Zhu ZC, et al. Rumination and the default mode network: Meta-analysis of brain imaging studies and implications for depression. Neuroimage. 2020; 206:116287. [DOI:10.1016/j.neuroimage.2019.116287] [PMID]
- Bartoskova M, Sevcikova M, Durisko Z, Maslej MM, Barbic SP, Preiss M, et al. The form and function of depressive rumination. Evolution and Human Behavior. 2018; 39(3):277-89. [DOI:10.1016/j.evolhumbehav.2018.01.005]
- McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 2011; 49(3):186-93. [DOI:10.1016/j.brat.2010.12.006] [PMID] [PMCID]
- Berman MG, Peltier S, Nee DE, Kross E, Deldin PJ, Jonides J. Depression, rumination and the default network. Social Cognitive and Affective Neuroscience. 2011; 6(5):548-55. [DOI:10.1093/scan/nsq080] [PMID] [PMCID]
- Di Schiena R, Luminet O, Chang B, Philippot P. Why are depressive individuals indecisive? Different modes of rumination account for indecision in non-clinical depression. Cognitive Therapy and Research. 2013; 37:713-24. [DOI:10.1007/s10608-012-9517-9]
- Mori M, Tanno Y. Mediating role of decentering in the associations between self-reflection, self-rumination, and depressive symptoms. Psychology. 2015; 6(5):613-21. [DOI:10.4236/psych.2015.65059]
- Kleiboer A, Donker T, Seekles W, van Straten A, Riper H, Cuijpers P. A randomized controlled trial on the role of support in Internet-based problem solving therapy for depression and anxiety. Behaviour research and therapy. 2015; 72:63-71.[DOI:10.1016/j.brat.2015.06.013] [PMID]
- Hasegawa A, Yoshida T, Hattori Y, Nishimura H, Morimoto H, Tanno Y. Depressive rumination and social problem solving in Japanese university students. Journal of Cognitive Psychotherapy. 2015; 29(2):134-52. [DOI:10.1891/0889-8391.29.2.134] [PMID]
- Raines AM, Vidaurri DN, Portero AK, Schmidt NB. Associations between rumination and obsessive-compulsive symptom dimensions. Personality and Individual Differences. 2017; 113:63-7. [DOI:10.1016/j.paid.2017.03.001]
- Wahl K, van den Hout M, Heinzel CV, Kollárik M, Meyer A, Benoy C, et al. Rumination about obsessive symptoms and mood maintains obsessive-compulsive symptoms and depressed mood: An experimental study. Journal of Abnormal Psychology. 2021; 130(5):435-42. [DOI:10.1037/abn0000677] [PMID]
- Satyshur MD, Layden EA, Gowins JR, Buchanan A, Gollan JK. Functional connectivity of reflective and brooding rumination in depressed and healthy women. Cognitive, Affective, & Behavioral Neuroscience. 2018; 18(5):884-901.[DOI:10.3758/s13415-018-0611-7] [PMID]
- Ricarte JJ, Ros L, Latorre JM, Muñoz MD, Aguilar MJ, Hernandez JV. Role of anxiety and brooding in specificity of autobiographical recall. Scandinavian journal of psychology. 2016; 57(6):495-500. [DOI:10.1111/sjop.12323] [PMID]
- Ros L, Latorre JM, Serrano JP, Ricarte JJ. Overgeneral autobiographical memory in healthy young and older adults: Differential age effects on components of the capture and rumination, functional avoidance, and impaired executive control (CaRFAX) model. Psychology and Aging. 2017; 32(5):447-59. [DOI:10.1037/pag0000175] [PMID]
- Watkins ER, Roberts H. Reflecting on rumination: Consequences, causes, mechanisms and treatment of rumination. Behaviour Research and Therapy. 2020; 127:103573. [DOI:10.1016/j.brat.2020.103573] [PMID]
- Michl LC, McLaughlin KA, Shepherd K, Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology. 2013; 122(2):339-52. [DOI:10.1037/a0031994] [PMID] [PMCID]
- Ruscio AM, Gentes EL, Jones JD, Hallion LS, Coleman ES, Swendsen J. Rumination predicts heightened responding to stressful life events in major depressive disorder and generalized anxiety disorder. Journal of Abnormal Psychology. 2015; 124(1):17-26. [DOI:10.1037/abn0000025] [PMID] [PMCID]
- Ghanizadeh A, Mohammadi MR, Bahraini S, Keshavarzi Z, Firoozabadi A, Shoshtari AA. Efficacy of N-acetylcysteine augmentation on obsessive compulsive disorder: A multicenter randomized double blind placebo controlled clinical trial. Iranian Journal of Psychiatry. 2017; 12(2):134-41. [PMCID]
- Ahadi H, Asadzadeh H. Effectiveness of positive thinking skills training on depression in female students. Iranian journal of educational sociology. 2019; 2(2):90-9. [DOI:10.29252/ijes.2.2.90]
- Mohammadkhani S, Bahari A, Akbarian Firoozabadi M. [Attachment styles and depression symptoms: The mediating role of rumination (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2017; 23(3):320-35. [DOI:10.29252/nirp.ijpcp.23.3.320]
- Whitmer A, Gotlib IH. Brooding and reflection reconsidered: A factor analytic examination of rumination in currently depressed, formerly depressed, and never depressed individuals. Cognitive Therapy and Research. 2011; 35:99-107. [DOI:10.1007/s10608-011-9361-3]
- Watkins ER. Depressive rumination and co-morbidity: evidence for brooding as a transdiagnostic process. Journal of rational-emotive & cognitive-behavior therapy. 2009; 27(3):160-75.[DOI:10.1007/s10942-009-0098-9] [PMID] [PMCID]
- =Liu Y, Yu X, Yang B, Zhang F, Zou W, Na A, et al. Rumination mediates the relationship between overgeneral autobiographical memory and depression in patients with major depressive disorder. BMC psychiatry. 2017; 17(1):103.[DOI:10.1186/s12888-017-1264-8] [PMID] [PMCID]
- Kim S, Yu BH, Lee DS, Kim JH. Ruminative response in clinical patients with major depressive disorder, bipolar disorder, and anxiety disorders. Journal of Affective Disorders. 2012; 136(1-2):e77-81. [DOI:10.1016/j.jad.2011.06.034] [PMID]
- Owens M, Gibb BE. Brooding rumination and attentional biases in currently non-depressed individuals: An eye-tracking study. Cognition and Emotion. 2017; 31(5):1062-9. [DOI:10.1080/02699931.2016.1187116] [PMID] [PMCID]
- Olson ML, Kwon P. Brooding perfectionism: Refining the roles of rumination and perfectionism in the etiology of depression. Cognitive Therapy and Research. 2008; 32(6):788-802. [DOI:10.1007/s10608-007-9173-7]
- Dell'Acqua C, Dal Bo E, Benvenuti SM, Ambrosini E, Vallesi A, Palomba D. Depressed mood, brooding rumination and affective interference: The moderating role of heart rate variability. International Journal of Psychophysiology. 2021; 165:47-55.[DOI:10.1016/j.ijpsycho.2021.03.011] [PMID]
- Woody ML, Burkhouse KL, Birk SL, Gibb BE. Brooding rumination and cardiovascular reactivity to a laboratory-based interpersonal stressor. Psychophysiology. 2015; 52(5):722-5. [DOI:10.1111/psyp.12397] [PMID] [PMCID]
- Kun B, Urbán R, Bőthe B. Griffiths MD, Demetrovics Z, Kökönyei G. Maladaptive rumination mediates the relationship between self-esteem, perfectionism, and work addiction: A largescale survey study. International Journal of Environmental Research. 2020; 17(19):7332. [DOI:10.3390/ijerph17197332] [PMID] [PMCID]
- Connolly CG, Ho TC, Blom EH, LeWinn KZ, Sacchet MD, Tymofiyeva O, et al. Resting-state functional connectivity of the amygdala and longitudinal changes in depression severity in adolescent depression. Journal of Affective Disorders. 2017; 207:86-94. [DOI:10.1016/j.jad.2016.09.026] [PMID] [PMCID]
- Makovac E, Meeten F, Watson DR, Herman A, Garfinkel SN, Critchley HD, et al. Alterations in amygdala-prefrontal functional connectivity account for excessive worry and autonomic dysregulation in generalized anxiety disorder. Biological Psychiatry. 2016; 80(10):786-95. [DOI:10.1016/j.biopsych.2015.10.013] [PMID]
- Hartley CA, Phelps EA. Anxiety and decision-making. Biological Psychiatry. 2012; 72(2):113-8. [DOI:10.1016/j.biopsych.2011.12.027] [PMID] [PMCID]
- Schäfer JÖ, Naumann E, Holmes EA, Tuschen-Caffier B, Samson AC. Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta-analytic review. Journal of Youth and Adolescence. 2017; 46(2):261-76. [DOI:10.1007/s10964-016-0585-0] [PMID]
- Arditte KA, Joormann J. Emotion regulation in depression: Reflection predicts recovery from a major depressive episode. Cognitive Therapy and Research. 2011; 35(6):536-43. [DOI:10.1007/s10608-011-9389-4]
- Iqbal N, Dar KA. Negative affectivity, depression, and anxiety: Does rumination mediate the links? Journal of Affective Disorders. 2015; 181:18-23. [DOI:10.1016/j.jad.2015.04.002] [PMID]
Type of Study: Original Article |
Subject:
Health
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








