Volume 11, Issue 2 (Spring 2023)
Iran J Health Sci 2023, 11(2): 109-116 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Valikhani M, Mazlum S R, Dehghani J, Eshraghi A, Mahdizadeh S M. The Effect of Sandbag and Ice Bag on the Pain After Percutaneous Coronary Intervention: A Randomized Clinical Trial. Iran J Health Sci 2023; 11 (2) :109-116
URL: http://jhs.mazums.ac.ir/article-1-846-en.html
URL: http://jhs.mazums.ac.ir/article-1-846-en.html
Department of Medical-surgical Nursing, Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. , mahdizadeh2671@gmail.com
Full-Text [PDF 704 kb]
(352 Downloads)
| Abstract (HTML) (704 Views)
Full-Text: (244 Views)
1. Introduction
Percutaneous coronary intervention (PCI) is used to treat and diagnose chronic coronary artery disease [1]. the femoral arterial site is commonly used for PCI [2]. Currently, almost 600 000 PCI cases are conducted in the United States, and about 95% of them are performed through femoral arteries [3]. Coronary heart diseases impose a significant economic burden of $4715 to $ 4908 billion upon Iran’s economic system [4]. Nonetheless, many patients experience discomfort and pain during femoral artery interventions when the catheters previously inserted into the femoral site are removed [5]. Despite good care, access-site (A-S) complications, like hematoma, bleeding, pseudoaneurysm, artery spasm, or thrombosis, can occur along with pain and possibly need urgent intervention [6].
Local vascular complications and vasovagal responses can be developed when the pain caused by catheter removal is not controlled effectively; hence, reducing the pain in patients undergoing this procedure is necessary [5]. Pharmacological treatment is one way to control pain after PCI [7]. Non-pharmacological methods are other ways of pain control after PCI. These methods are patient-specific and aimed at establishing empathic communication with healthcare staff [8, 9]. Non-pharmacological approaches for pain control provided positive effects, like decreased anxiety and psychological support. Patients reported satisfaction with these non-pharmacological methods [5]. Using the sandbag is currently the conventional non-pharmacological method to control PCI’s local complications and pain. In this procedure, patients have to rest entirely on the bed (for 6-24 hours, depending on the treatment protocol), have absolute immobility of foot, and use of sandbag weighing 2.5 to 4 kg for about 6 hours after sheath removal [10]. Total resting of the patients immediately after angiography causes intolerance, discomfort, and hemodynamic instability. Patients’ non-cooperation in compliance with absolute resting on the bed after the procedure has been reported as a significant factor in femoral complications [10]. Other pain reduction methods are using ice and cold. Ice therapy has been employed since the old days as a non-invasive technique to control bleeding and reduce pain. One of the physiological effects of ice therapy is the reduction of nerve conduction, vascular contraction, and lowering of histamine release, thus reducing inflammation, muscle spasm, and pain [11]. The use of ice and cold therapy after orthopedic and maxillofacial surgeries has been associated with reduced pain and inflammation in some cases [12]. As angioplasty is used increasingly in the treatment of heart disease and complications and due to the lack of information about the more effective methods to reduce pain after this procedure, this research was conducted to compare the effect of sandbag alone with sandbag plus ice bag in reducing the pain after PCI.
2. Materials and Methods
This study was designed according to CONSORT guidelines for randomized clinical trials [13] in the Angiography Ward of Imam Reza Hospital, Mashhad City, Iran, in 2018.
The sample size was determined based on a pilot study involving 10 individuals in each group. The estimation was based on the formula for comparing the means of the two populations in terms of pain variable while taking into account the type I (α=0.05) and type II error (β=0.20). The highest estimated sample size was associated with the mean scores of pain (27 in each group). At least 30 subjects were included in each group to ensure adequate statistical power.
Sixty patients who were candidates for angiography and referred to Imam Reza Hospital were randomly assigned to the intervention and control groups after obtaining the approval of the Ethics Committee from the Mashhad University of Medical Sciences and obtaining the written consent of patients. The researchers selected the subjects based on the inclusion and exclusion criteria using a convenient sampling method in coordination with hospital authorities. The inclusion criteria were age over 18 years, a body mass index between 18 and 30 kg/m2, no history of addiction, only one catheter puncture for insertion, and alertness. The exclusion criteria comprised the use of sedatives, dysphoria, sudden changes in blood pressure, and undergoing cardiopulmonary resuscitation. They randomly assigned the patients into the sandbag group (control) and the sandbag combined with the ice bag group (intervention). We used simple randomization based on a lottery.
In the control group (sandbag), the patients were transferred to the unit in the supine position and placed on the bed without moving their legs. The pain intensity was checked and recorded at the beginning of the study. Then, the arterial sheath was removed 4 hours after completing the procedure. After initial coagulation, a transparent dressing was placed on-site with hand pressure, and the patient was placed in position again for up to 4 hours, and a sandbag with a fixed weight of 3 kg was placed on the angiography site. Then, the bag was removed, and the patient rested for 3 hours in the direction of his or her healthy foot.
In the intervention group (sandbag and ice bag), the arterial sheath was removed 4 hours after completing the procedure. After initial coagulation, a transparent dressing was placed on the site, and an ice bag with a cloth cover (weighed less than 100 g) and a sandbag weighing 3 kg were placed on it for 15 minutes. After 15 minutes, the ice bag was removed gently, and the sandbag was placed alone on the site for 45 minutes. This cycle was repeated 4 times (a total of 4 hours). Then, the sandbag was removed, and the patient rested for three hours without moving toward his or her healthy foot. The pain was checked and recorded in both groups at the beginning of sheath removal (before) and 3, 6, and 12 hours after the intervention.
The data collection tool included two sections. The first section consisted of a demographic questionnaire obtained through interviews with patients and their medical records, including age, gender, marital status, education, history of angiography, weight, and height of patients, and drugs used. The second section included a numerical rating scale (NRS) for measuring the pain of the patients [14]. The validity of the subjects’ selection checklist, the demographic and clinical characteristics of the subjects, and the physiological characteristics recording questionnaire were determined using content validity. Accordingly, it was developed by studying the latest books and articles on research under the guidance of supervisors and advisors. Then, it was given to 7 experts and faculty members of The Department of Nursing and Midwifery of Mashhad University of Medical Sciences to be evaluated. After considering the required suggestions and reforms, the final tool was developed.
The numeric rating scale is an 11-point scale ranging from 0 through 10, where 0 represents “No pain” and 10 represents “Worst imaginable pain”. Participants are asked to choose the number that best describes their pain intensity [14]. The NRS has demonstrated validity and sensitivity to change [15, 16], with good construct validity reported in experimental settings and individuals with rheumatic disease [16]. In the current study, the reliability of the NRS was confirmed by test-retest, yielding a coefficient of 0.86.
The obtained data were analyzed by descriptive (mean±SD) and inferential statistics using SPSS software, version 11.5 (SPSS, Inc. Chicago, IL, USA). The Kolmogorov-Smirnov test was used to check the normality of the data. To compare two groups in terms of the homogeneity of contextual, intervening, and dependent variables, in the case of quantitative variables with normal distribution, independent t-test and in the case of quantitative variables with non-normal distribution, the Mann-Whitney test and in nominal and rank qualitative variables Fisher exact test, Chi-square, and exact Chi-square tests were used. The researchers employed the Mann-Whitney and Friedman test to compare the mean changes of the pain immediately, 3, 6, and 12 hours after sheath removal compared to the baseline between groups. The significance level was considered less than 0.05.
3. Results
In this study, 30 patients in both groups completed the study (Figure 1). The statistical analyses revealed that both groups were comparable in all underlying and confounding variables, with no significant differences observed (Table 1).

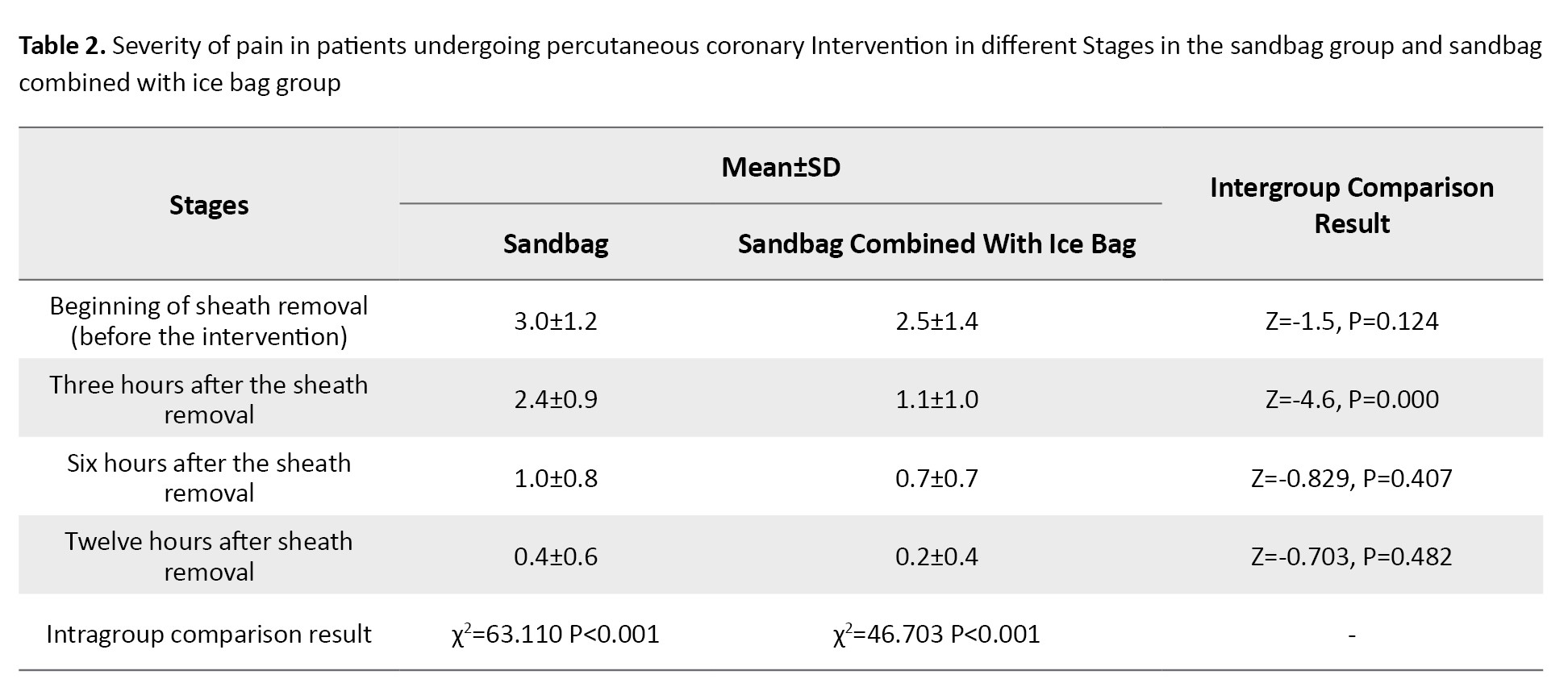
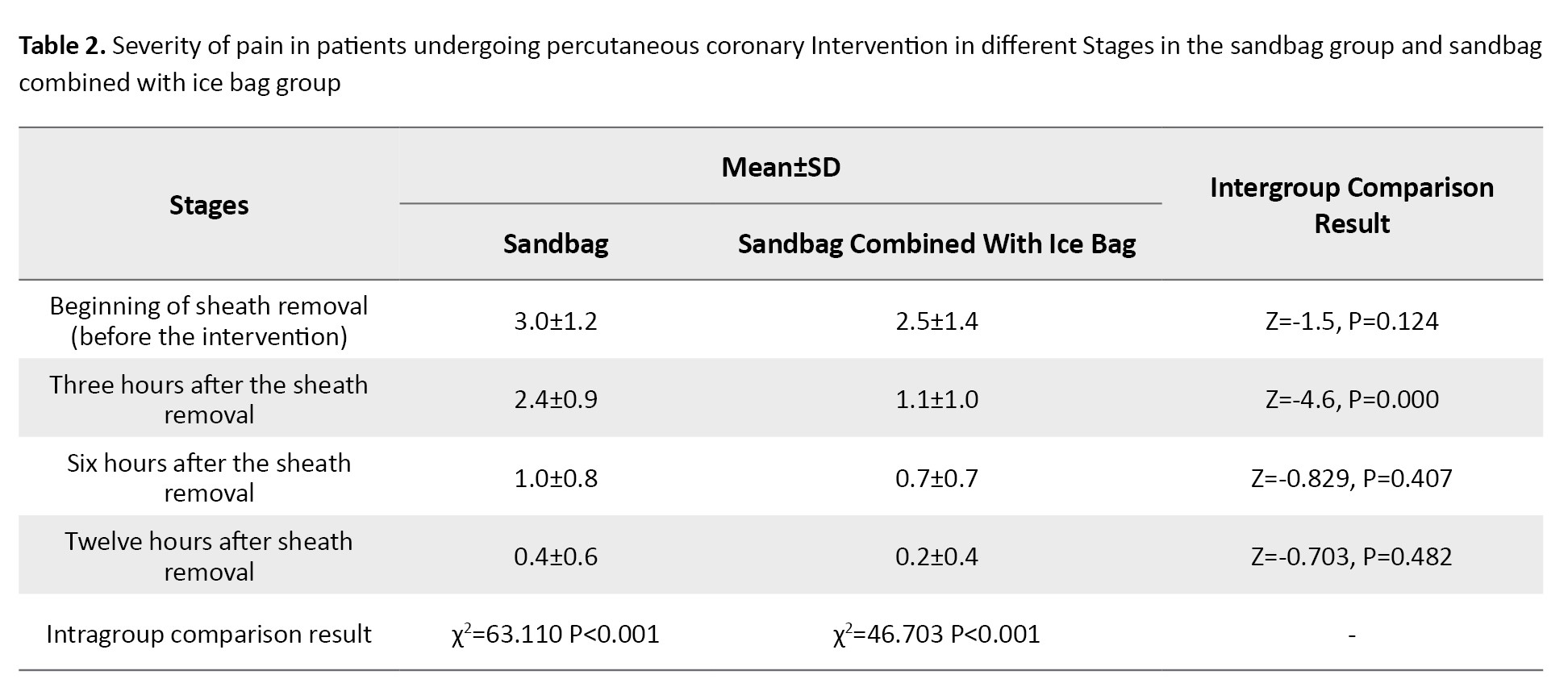
The Kolmogorov-Smirnov statistical test result showed that the pain variable was only normal at the beginning of sheath removal (before the intervention). The results of the Mann-Whitney test showed that at the beginning of sheath removal, the difference between the two groups was not significant in terms of pain (P=0.124). However, the mean pain severity in the sandbag combined with the ice bag group was significantly lower than that of the other group at 3 hours after the sheath removal (P<0.001). However, the difference between the two groups was not significant at the 6 (P=0.407) and 12 hours (P=0.482) after sheath removal.
The Friedman test results showed a significant difference regarding the pain intensity in different stages of measurement in both groups (P<0.001). The post hoc test showed these differences were significant in the ice bag group between the beginning of sheath removal and 3, 6, and 12 hours after the intervention (P<0.001), between the 3 hours and 12 hours (P<0.001), and between 6 and 12 hours (P<0.001). In contrast, the difference between the 3 and 6 hours was not significant (P=0.084). However, a significant difference was found in the mean pain in the sandbag combined with the ice bag group at the beginning of sheath removal and 3, 6, and 12 hours after the intervention (P<0.001) (Table 2).
4. Discussion
This research compared the effect of sandbag alone and ice bag plus sandbag in reducing patients’ pain after angiography. Results showed that the simultaneous sand-ice bag use reduced post-PCI pain better than the sandbag alone: sandbag as an agent for creating external pressure, and ice bag as an agent for lowering neurotransmission conduction to minimize pain after coronary angioplasty. Another study reported that ice bag use at the femoral site effectively decreased pain caused by femoral catheter removal in cases receiving the percutaneous coronary intervention [5]. A study showed that ice application before arterial puncture was well tolerated and reduced procedure-related pain [17]. Therefore, the cold application can be used as an essential non-pharmacological nursing initiative for pain management.
Non-pharmacological methods, like cold application, should be regarded to reduce analgesic use by the patient [5]. Pain relief using the cold application is done by many mechanisms, such as inhibition of nociceptors, altered nerve conduction velocity, reduced muscle spasms, and decreased metabolic enzyme activity [18].
A clinical trial compared sandbag and air cushion methods on post-angioplasty complications in Mazandaran Province, Iran, in 80 patients. In this study, the low back and groin pain were significantly higher in the sandbag group than in the air cushion group (P=0.001). In the air cushion group, 10% of patients needed opioids, and 30% required opioids [19]. In the mentioned study, pain in the groin area was reported with the presence of a sandbag. Therefore, the researcher of this study tried to maintain sandbags on the site (due to their necessity in preventing vascular complications). Another applied method is the combination with ice to reduce the patient’s pain rate in the groin caused by catheter insertion and the presence of a sandbag [19]. Another study was conducted on 51 patients undergoing heart surgery at Imam Reza Hospital in Mashhad City with at least two chest tubes. Patients were divided into three groups: ice bag, placebo, and control. The bags were inserted around the tube for 20 minutes before removing the chest tube. In this study, cold therapy was used once for each patient [20] but 4 times for each patient in the current study. In addition, the visual analog scale was used as a pain measurement tool in the mentioned study, while the numerical pain measurement scale was used in the current research.
This study was consistent with our investigation and showed a positive effect of ice and sandbags in reducing patients’ pain. An important limitation of this study was the difference in pain threshold and patient’s perception of maximum pain according to the different experiences of each individual and the impossibility of eliminating its effect.
5. Conclusion
Although both interventions reduced the patient’s pain, the group with the combination of ice and sandbag tolerated less pain 3 and 6 hours after removing the sheath. Thus, this method can be applied as an available, effective, and cost-effective technique in angiography units of hospitals for reducing local pain.
Ethical Considerations
Compliance with ethical guidelines
We obtained the license of the Ethics Committee from the Mashhad University of Medical Sciences (Ethics No.: IR.MUMS.REC.1396.312) and obtained patients’ written consent.
Funding
The paper was extracted from the MSc. Thesis of Maryam Valikhani, Department of Medical-surgical Nursing, Faculty of Nursing and Midwifery, Mashhad University of Medical Sciences (Clinical trial Code: IRCT20180315039107N1).
Authors contributions
Conceptualization and Supervision: Seyad Mousa Mahdizadeh and Maryam Valikhani; Methodology: Seyed Reza Mazlum; Investigation, Writing-original draft, and Writing-review & editing: All authors; Data collection: Maryam Valikhani and Javad Dehghani; Data analysis: Seyed Reza Mazlum and Seyad Mousa Mahdizadeh; Funding acquisition and Resources: Maryam Valikhani and Seyad Mousa Mahdizadeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The researchers of this study thank the Research Deputy of Mashhad University of Medical Sciences for financial support and all patients and participants who helped us conduct this study.
References
Percutaneous coronary intervention (PCI) is used to treat and diagnose chronic coronary artery disease [1]. the femoral arterial site is commonly used for PCI [2]. Currently, almost 600 000 PCI cases are conducted in the United States, and about 95% of them are performed through femoral arteries [3]. Coronary heart diseases impose a significant economic burden of $4715 to $ 4908 billion upon Iran’s economic system [4]. Nonetheless, many patients experience discomfort and pain during femoral artery interventions when the catheters previously inserted into the femoral site are removed [5]. Despite good care, access-site (A-S) complications, like hematoma, bleeding, pseudoaneurysm, artery spasm, or thrombosis, can occur along with pain and possibly need urgent intervention [6].
Local vascular complications and vasovagal responses can be developed when the pain caused by catheter removal is not controlled effectively; hence, reducing the pain in patients undergoing this procedure is necessary [5]. Pharmacological treatment is one way to control pain after PCI [7]. Non-pharmacological methods are other ways of pain control after PCI. These methods are patient-specific and aimed at establishing empathic communication with healthcare staff [8, 9]. Non-pharmacological approaches for pain control provided positive effects, like decreased anxiety and psychological support. Patients reported satisfaction with these non-pharmacological methods [5]. Using the sandbag is currently the conventional non-pharmacological method to control PCI’s local complications and pain. In this procedure, patients have to rest entirely on the bed (for 6-24 hours, depending on the treatment protocol), have absolute immobility of foot, and use of sandbag weighing 2.5 to 4 kg for about 6 hours after sheath removal [10]. Total resting of the patients immediately after angiography causes intolerance, discomfort, and hemodynamic instability. Patients’ non-cooperation in compliance with absolute resting on the bed after the procedure has been reported as a significant factor in femoral complications [10]. Other pain reduction methods are using ice and cold. Ice therapy has been employed since the old days as a non-invasive technique to control bleeding and reduce pain. One of the physiological effects of ice therapy is the reduction of nerve conduction, vascular contraction, and lowering of histamine release, thus reducing inflammation, muscle spasm, and pain [11]. The use of ice and cold therapy after orthopedic and maxillofacial surgeries has been associated with reduced pain and inflammation in some cases [12]. As angioplasty is used increasingly in the treatment of heart disease and complications and due to the lack of information about the more effective methods to reduce pain after this procedure, this research was conducted to compare the effect of sandbag alone with sandbag plus ice bag in reducing the pain after PCI.
2. Materials and Methods
This study was designed according to CONSORT guidelines for randomized clinical trials [13] in the Angiography Ward of Imam Reza Hospital, Mashhad City, Iran, in 2018.
The sample size was determined based on a pilot study involving 10 individuals in each group. The estimation was based on the formula for comparing the means of the two populations in terms of pain variable while taking into account the type I (α=0.05) and type II error (β=0.20). The highest estimated sample size was associated with the mean scores of pain (27 in each group). At least 30 subjects were included in each group to ensure adequate statistical power.
Sixty patients who were candidates for angiography and referred to Imam Reza Hospital were randomly assigned to the intervention and control groups after obtaining the approval of the Ethics Committee from the Mashhad University of Medical Sciences and obtaining the written consent of patients. The researchers selected the subjects based on the inclusion and exclusion criteria using a convenient sampling method in coordination with hospital authorities. The inclusion criteria were age over 18 years, a body mass index between 18 and 30 kg/m2, no history of addiction, only one catheter puncture for insertion, and alertness. The exclusion criteria comprised the use of sedatives, dysphoria, sudden changes in blood pressure, and undergoing cardiopulmonary resuscitation. They randomly assigned the patients into the sandbag group (control) and the sandbag combined with the ice bag group (intervention). We used simple randomization based on a lottery.
In the control group (sandbag), the patients were transferred to the unit in the supine position and placed on the bed without moving their legs. The pain intensity was checked and recorded at the beginning of the study. Then, the arterial sheath was removed 4 hours after completing the procedure. After initial coagulation, a transparent dressing was placed on-site with hand pressure, and the patient was placed in position again for up to 4 hours, and a sandbag with a fixed weight of 3 kg was placed on the angiography site. Then, the bag was removed, and the patient rested for 3 hours in the direction of his or her healthy foot.
In the intervention group (sandbag and ice bag), the arterial sheath was removed 4 hours after completing the procedure. After initial coagulation, a transparent dressing was placed on the site, and an ice bag with a cloth cover (weighed less than 100 g) and a sandbag weighing 3 kg were placed on it for 15 minutes. After 15 minutes, the ice bag was removed gently, and the sandbag was placed alone on the site for 45 minutes. This cycle was repeated 4 times (a total of 4 hours). Then, the sandbag was removed, and the patient rested for three hours without moving toward his or her healthy foot. The pain was checked and recorded in both groups at the beginning of sheath removal (before) and 3, 6, and 12 hours after the intervention.
The data collection tool included two sections. The first section consisted of a demographic questionnaire obtained through interviews with patients and their medical records, including age, gender, marital status, education, history of angiography, weight, and height of patients, and drugs used. The second section included a numerical rating scale (NRS) for measuring the pain of the patients [14]. The validity of the subjects’ selection checklist, the demographic and clinical characteristics of the subjects, and the physiological characteristics recording questionnaire were determined using content validity. Accordingly, it was developed by studying the latest books and articles on research under the guidance of supervisors and advisors. Then, it was given to 7 experts and faculty members of The Department of Nursing and Midwifery of Mashhad University of Medical Sciences to be evaluated. After considering the required suggestions and reforms, the final tool was developed.
The numeric rating scale is an 11-point scale ranging from 0 through 10, where 0 represents “No pain” and 10 represents “Worst imaginable pain”. Participants are asked to choose the number that best describes their pain intensity [14]. The NRS has demonstrated validity and sensitivity to change [15, 16], with good construct validity reported in experimental settings and individuals with rheumatic disease [16]. In the current study, the reliability of the NRS was confirmed by test-retest, yielding a coefficient of 0.86.
The obtained data were analyzed by descriptive (mean±SD) and inferential statistics using SPSS software, version 11.5 (SPSS, Inc. Chicago, IL, USA). The Kolmogorov-Smirnov test was used to check the normality of the data. To compare two groups in terms of the homogeneity of contextual, intervening, and dependent variables, in the case of quantitative variables with normal distribution, independent t-test and in the case of quantitative variables with non-normal distribution, the Mann-Whitney test and in nominal and rank qualitative variables Fisher exact test, Chi-square, and exact Chi-square tests were used. The researchers employed the Mann-Whitney and Friedman test to compare the mean changes of the pain immediately, 3, 6, and 12 hours after sheath removal compared to the baseline between groups. The significance level was considered less than 0.05.
3. Results
In this study, 30 patients in both groups completed the study (Figure 1). The statistical analyses revealed that both groups were comparable in all underlying and confounding variables, with no significant differences observed (Table 1).

The Kolmogorov-Smirnov statistical test result showed that the pain variable was only normal at the beginning of sheath removal (before the intervention). The results of the Mann-Whitney test showed that at the beginning of sheath removal, the difference between the two groups was not significant in terms of pain (P=0.124). However, the mean pain severity in the sandbag combined with the ice bag group was significantly lower than that of the other group at 3 hours after the sheath removal (P<0.001). However, the difference between the two groups was not significant at the 6 (P=0.407) and 12 hours (P=0.482) after sheath removal.
The Friedman test results showed a significant difference regarding the pain intensity in different stages of measurement in both groups (P<0.001). The post hoc test showed these differences were significant in the ice bag group between the beginning of sheath removal and 3, 6, and 12 hours after the intervention (P<0.001), between the 3 hours and 12 hours (P<0.001), and between 6 and 12 hours (P<0.001). In contrast, the difference between the 3 and 6 hours was not significant (P=0.084). However, a significant difference was found in the mean pain in the sandbag combined with the ice bag group at the beginning of sheath removal and 3, 6, and 12 hours after the intervention (P<0.001) (Table 2).
4. Discussion
This research compared the effect of sandbag alone and ice bag plus sandbag in reducing patients’ pain after angiography. Results showed that the simultaneous sand-ice bag use reduced post-PCI pain better than the sandbag alone: sandbag as an agent for creating external pressure, and ice bag as an agent for lowering neurotransmission conduction to minimize pain after coronary angioplasty. Another study reported that ice bag use at the femoral site effectively decreased pain caused by femoral catheter removal in cases receiving the percutaneous coronary intervention [5]. A study showed that ice application before arterial puncture was well tolerated and reduced procedure-related pain [17]. Therefore, the cold application can be used as an essential non-pharmacological nursing initiative for pain management.
Non-pharmacological methods, like cold application, should be regarded to reduce analgesic use by the patient [5]. Pain relief using the cold application is done by many mechanisms, such as inhibition of nociceptors, altered nerve conduction velocity, reduced muscle spasms, and decreased metabolic enzyme activity [18].
A clinical trial compared sandbag and air cushion methods on post-angioplasty complications in Mazandaran Province, Iran, in 80 patients. In this study, the low back and groin pain were significantly higher in the sandbag group than in the air cushion group (P=0.001). In the air cushion group, 10% of patients needed opioids, and 30% required opioids [19]. In the mentioned study, pain in the groin area was reported with the presence of a sandbag. Therefore, the researcher of this study tried to maintain sandbags on the site (due to their necessity in preventing vascular complications). Another applied method is the combination with ice to reduce the patient’s pain rate in the groin caused by catheter insertion and the presence of a sandbag [19]. Another study was conducted on 51 patients undergoing heart surgery at Imam Reza Hospital in Mashhad City with at least two chest tubes. Patients were divided into three groups: ice bag, placebo, and control. The bags were inserted around the tube for 20 minutes before removing the chest tube. In this study, cold therapy was used once for each patient [20] but 4 times for each patient in the current study. In addition, the visual analog scale was used as a pain measurement tool in the mentioned study, while the numerical pain measurement scale was used in the current research.
This study was consistent with our investigation and showed a positive effect of ice and sandbags in reducing patients’ pain. An important limitation of this study was the difference in pain threshold and patient’s perception of maximum pain according to the different experiences of each individual and the impossibility of eliminating its effect.
5. Conclusion
Although both interventions reduced the patient’s pain, the group with the combination of ice and sandbag tolerated less pain 3 and 6 hours after removing the sheath. Thus, this method can be applied as an available, effective, and cost-effective technique in angiography units of hospitals for reducing local pain.
Ethical Considerations
Compliance with ethical guidelines
We obtained the license of the Ethics Committee from the Mashhad University of Medical Sciences (Ethics No.: IR.MUMS.REC.1396.312) and obtained patients’ written consent.
Funding
The paper was extracted from the MSc. Thesis of Maryam Valikhani, Department of Medical-surgical Nursing, Faculty of Nursing and Midwifery, Mashhad University of Medical Sciences (Clinical trial Code: IRCT20180315039107N1).
Authors contributions
Conceptualization and Supervision: Seyad Mousa Mahdizadeh and Maryam Valikhani; Methodology: Seyed Reza Mazlum; Investigation, Writing-original draft, and Writing-review & editing: All authors; Data collection: Maryam Valikhani and Javad Dehghani; Data analysis: Seyed Reza Mazlum and Seyad Mousa Mahdizadeh; Funding acquisition and Resources: Maryam Valikhani and Seyad Mousa Mahdizadeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The researchers of this study thank the Research Deputy of Mashhad University of Medical Sciences for financial support and all patients and participants who helped us conduct this study.
References
- Mert Boğa S, Öztekin SD. The effect of position change on vital signs, back pain and vascular complications following percutaneous coronary intervention. Journal of Clinical Nursing. 2019; 28(7-8):1135-47. [DOI:10.1111/jocn.14704] [PMID]
- Armendaris MK, Azzolin KDO, Alves FJMS, Ritter SG, de Moraes MAP. [Incidence of vascular complications in patients submitted to percutaneous transluminal coronary angioplasty by transradial and transfemoral arterial approach (Portuguese)]. Acta Paulista de Enfermagem. 2008; 21(1):107-11. [DOI:10.1590/S0103-21002008000100017]
- Amin AP, Pinto D, House JA, Rao SV, Spertus JA, Cohen MG, et al. Association of same-day discharge after elective percutaneous coronary intervention in the United States with costs and outcomes. JAMA Cardiology. 2018; 3(11):1041-9. [DOI:10.1001/jamacardio.2018.3029] [PMID] [PMCID]
- Raghfar H, Sargazi N, Mehraban S, Akbarzadeh MA, Vaez Mahdavi MR, Vahdati Manesh Z. [The economic burden of coronary heart disease in Iran: A bottom-up approach in 2014 (Persian)]. Journal of Ardabil University of Medical Sciences. 2018; 18(3):341-56. [DOI:10.29252/jarums.18.3.341]
- Bayındır SK, Çürük GN, Oguzhan A. Effect of ice bag application to femoral region on pain in patients undergoing percutaneous coronary intervention. Pain Research & Management. 2017; 2017:6594782. [DOI:10.1155/2017/6594782] [PMID] [PMCID]
- Brogiene L, Baksyte G, Klimaite A, Paliokas M, Macas A. Predictive factors for access-site pain chronicity after percutaneous coronary intervention via radial artery access. Pain Research & Management. 2020; 2020:8887499. [DOI:10.1155/2020/8887499] [PMID] [PMCID]
- Suh JW, Chung WY, Kim YS, Kim KI, Jeon EJ, Cho YS, et al. The effect of intravenous administration of erythropoietin on the infarct size in primary percutaneous coronary intervention. International Journal of Cardiology. 2011; 149(2):216-20. [DOI:10.1016/j.ijcard.2010.02.002] [PMID]
- Demir Y, Khorshid L. The effect of cold application in combination with standard analgesic administration on pain and anxiety during chest tube removal: A single-blinded, randomized, double-controlled study. Pain Management Nursing. 2010; 11(3):186-96.[DOI:10.1016/j.pmn.2009.09.002] [PMID]
- Ertuğ N, Ulker S. The effect of cold application on pain due to chest tube removal. Journal of Clinical Nursing. 2012; 21(5-6):784-90.[DOI:10.1111/j.1365-2702.2011.03955.x] [PMID]
- Yousefi AA, Madani M, Azimi HR, Farshidi H. [The factors relevant to the onset of vascular complications after coronary intervention in Shahid Rajaei Cardiovascular Center in Tehran, Iran (Persian)]. Tehran University Medical Journal. 2011;69(7):445-50. [Link]
- DeLaune SC, Ladner PK. Fundamentals of nursing. Boston: Cengage Learning; 2010. [Link]
- King NA, Philpott SJ, Leary A. A randomized controlled trial assessing the use of compression versus vasoconstriction in the treatment of femoral hematoma occurring after percutaneous coronary intervention. Heart & Lung. 2008; 37(3):205-10. [DOI:10.1016/j.hrtlng.2007.05.008] [PMID]
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ. 2010; 340:c332. [DOI:10.1136/bmj.c332] [PMID] [PMCID]
- Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011; 152(10):2399-404.[DOI:10.1016/j.pain.2011.07.005] [PMID]
- Breivik EK, Björnsson GA, Skovlund E. A comparison of pain rating scales by sampling from clinical trial data. The Clinical Journal of Pain. 2000; 16(1):22-8. [DOI:10.1097/00002508-200003000-00005] [PMID]
- Herr KA, Spratt K, Mobily PR, Richardson G. Pain intensity assessment in older adults: Use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. The Clinical Journal of Pain. 2004; 20(4):207-19. [DOI:10.1097/00002508-200407000-00002] [PMID]
- Haynes JM. Randomized controlled trial of cryoanalgesia (ice bag) to reduce pain associated with arterial puncture. Respiratory Care. 2015; 60(1):1-5. [DOI:10.4187/respcare.03312] [PMID]
- Algafly AA, George KP. The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. British Journal of Sports Medicine. 2007; 41(6):365-9. [DOI:10.1136/bjsm.2006.031237] [PMID] [PMCID]
- Ghods AA, Bagheri S, Ghorbani R, Asgari MR. [Comparison of two methods of air cushions and sand bags on complications after coronary artery angioplasty (Persian)]. Journal of Mazandaran University of Medical Sciences. 2014; 24(111):68-76. [Link]
- Mazloum SR, Abbasi Teshnizi M, Kianinejad A, Gandomkar F. [Effect of applying ice bag on pain intensity associated with chest tube removal after cardiac surgery (Persian)]. International Medicine Today. 2012; 18(3): 110-14. [Link]
Type of Study: Original Article |
Subject:
Nursing
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |