Volume 11, Issue 2 (Spring 2023)
Iran J Health Sci 2023, 11(2): 75-86 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salehnia N, Assari Arani A, Olyaeemanesh A, Sadeghi Saghdel H. Identifying and Prioritizing Social Determinants of Population Health in Iran: A Mixed Method Research. Iran J Health Sci 2023; 11 (2) :75-86
URL: http://jhs.mazums.ac.ir/article-1-855-en.html
URL: http://jhs.mazums.ac.ir/article-1-855-en.html
Department of Economic Development and Planning, Faculty of Management and Economics, Tarbiat Modares University, Tehran, Iran. , assari_a@modares.ac.ir
Full-Text [PDF 3078 kb]
(2146 Downloads)
| Abstract (HTML) (3298 Views)
Full-Text: (1312 Views)
1. Introduction
According to the World Health Organization (WHO), the social determinants of health (SDH) refer to the circumstances effective in individuals’ health outcomes, including the environmental, economic, social, and cultural factors that influence their experiences from birth to old age, as well as the societal structures and processes that shape these conditions [1]. These systems include economic system, culture and social values, governance, and policymaking, national policies and social environment [2], immigrant policies, laws, regulations, institutions, and agencies [3], economic stability, education, neighborhood, and living environment [4], perceived neighborhood crime [5], adjustable housing, sustainable employment, access to healthy food, and quality schools [6].
Public health focused on the physical environment in the late 19th and early 20th centuries. For example, people’s life expectancy increased dramatically by improving the safe drinking water supply, sanitary housing, sewage system, workplace safety, and healthy eating. In the later decades of the 20th century, the focus on access to healthcare led to the further extension of lifespan. In recent decades, studies have increasingly shown how economic and social conditions determine health and how the heterogeneity of health status in various groups is more related to economic and social health factors than health services [7].
In recent decades, empirical and conceptual studies have mainly concentrated on proximal social determinants such as individual traits. Although studying these factors is relatively easy, they are far less critical and controllable for policymakers than macrosocial factors such as tax policies [8, 9]. Public health interventions should address social determinants of health (SDH) to improve population health. Public health has both direct and indirect effects (through social determinants) on population health [10]. Hence, with the emergence of public health, researchers in this field have been more interested in studying the role of social health factors, investigating how social conditions affect health and how to arrange them to improve population health [11]. It is promising for policymakers to identify the social factors affecting health outcomes as their interventions control and change these factors [8]. Many of these health determinants depend on the other sectors outside the health system [2]. Thus, the main issue is the other sectors’ awareness of the effects of their decisions on health and the integration of health goals with other policies by addressing the health determinants in all sectors. Conceptual models can help policymakers better understand the situation and make more appropriate interventions. Despite numerous studies on the health of Iran’s population, they have insufficiently and inadequately examined health’s social and economic determinants. Developing a comprehensive map of the SDH could facilitate a coordinated government response to address health issues and disparities in society.
Determining the importance and prioritization of the determinants of population health can reveal the most important policy goals and help policymakers allocate resources optimally to promote population health. This study aims to answer the following two main questions:
What are the social determinants of population health?
What are the prioritizing social determinants of population health in Iran?
So, first, by analyzing the available scientific sources, the determinants of health at all levels and sections were identified and categorized. It represents a comprehensive picture of these factors via semantic mapping from different perspectives and levels. This semantic mapping allows decision-makers to effectively identify the determinants of population health. In the next stage, experts used the fuzzy Delphi method to determine the most important social determinants of population health in Iran. Determining the most important factors can help policymakers invest appropriately and allocate resources optimally to promote population health.
2. Materials and Methods
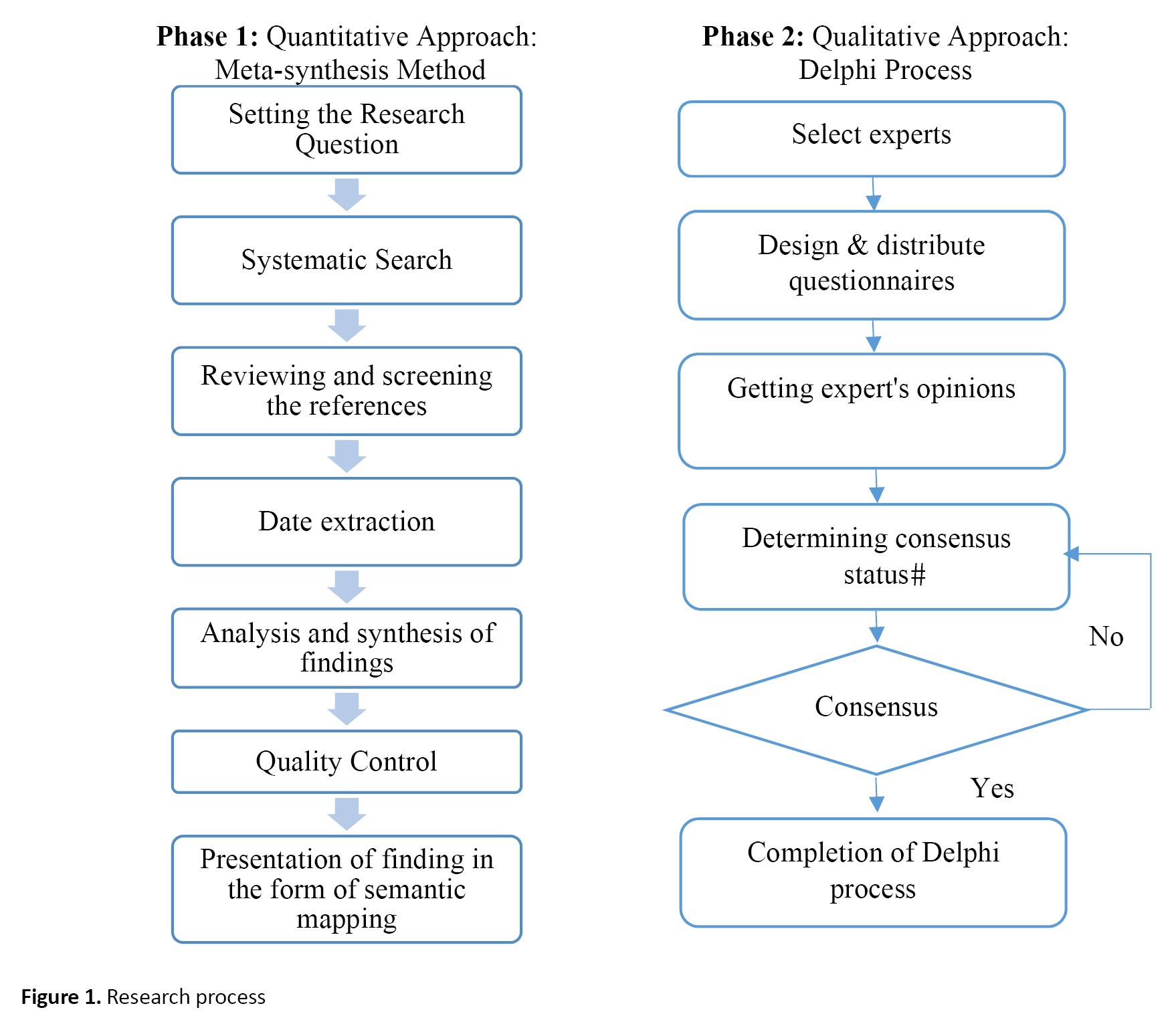
This study employs an explanatory-sequential mixed-method study, combining and integrating quantitative and qualitative approaches in a single model [12]. This mixed approach offers a more revealing insight into the research issues and complicated phenomena than either method separately [13]. The mixed method approach is used in this research. The research process is shown in Figure 1. Meta-synthesis
This research employs a meta-synthesis method to map the SDH. The meta-synthesis method is a qualitative research strategy that provides researchers with a systematic approach to combine study and identify hidden themes and analogies. Qualitative syntheses currently encompass a wide variety of methods without established guidelines since they are a relatively recent field of research [14]. We used Sandelowski and Barros’s 7-step approach [15] as follows:
Step 1. Formulating the research question
What are the social determinants of population health?
Step 2. Systematic search
This step searches the keywords including “social determinant of health”, “SDH”, “determinant of health”, and “socioeconomic factor” in the scientific databases, including Google Scholar, ScienceDirect, Springer, Emerald, PubMed, ProQuest, and Scopus published from 2000 to 2020. Searching the keywords offers us the first group of scientific sources, paving the way for searching other related references.
Step 3. Reviewing and screening the references
This step reviews and filters the resources derived in the previous step based on our criteria, including title, abstract, and content (including citation information, the use of other models in the research and repetitiveness, non-clarification of the detected components, and the lack of access to the content).
Step 4. Extracting information from the resources using the qualitative content analysis method
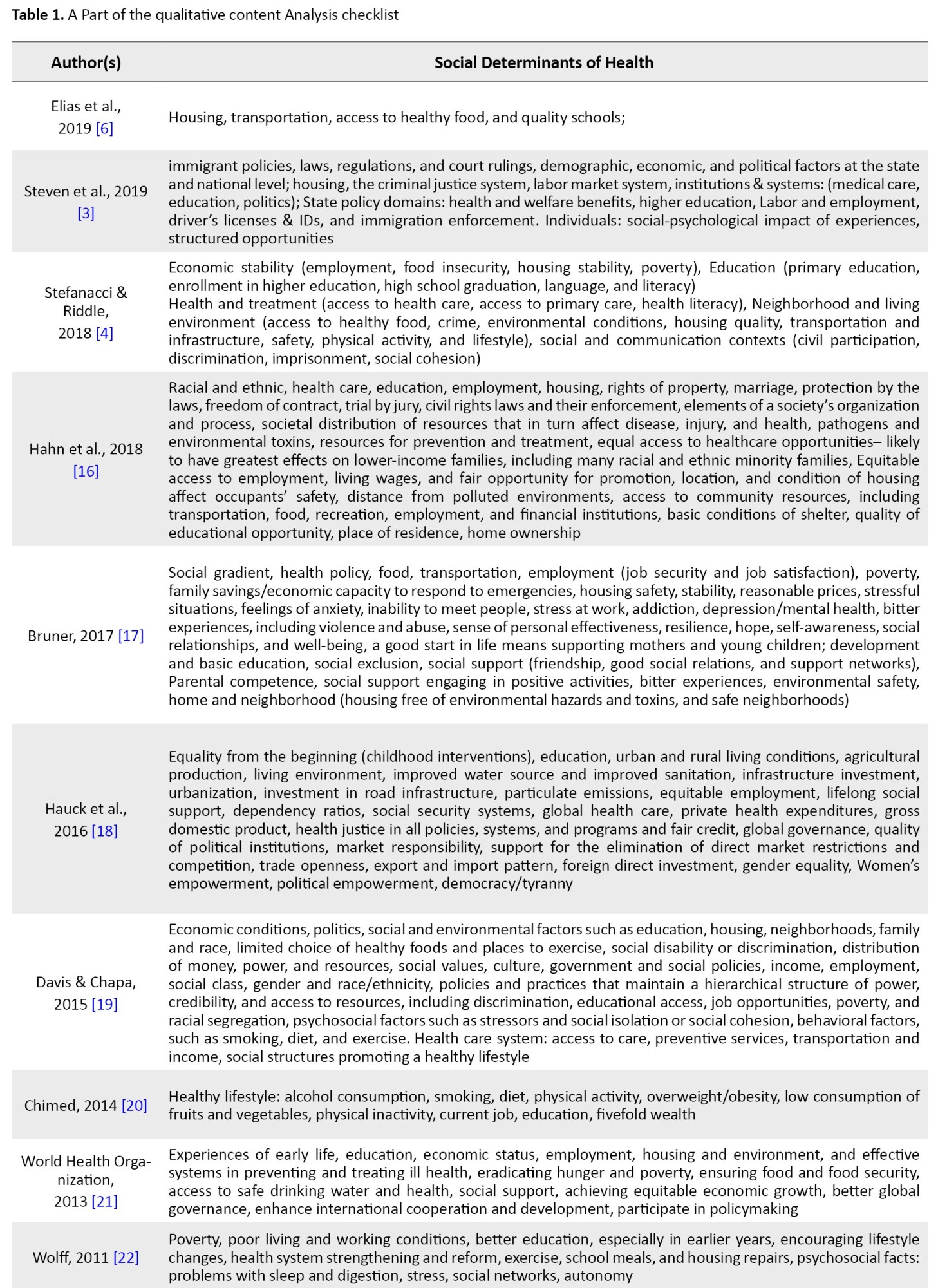
This step uses the qualitative content analysis method to extract the social determinants of health from 58 resources. Since this study aims to identify and categorize all social determinants of health cases, it first investigates the whole text to mark those sections related to social determinants of health according to our initial perception. Then, our predefined codes encrypt the marked parts. Also, new codes are assigned to parts of the text not encrypted according to this marking. Accordingly, this step reviews all the studies and selects the codes related to the keyword to form categories, themes, and subcategories. A part of the qualitative content analysis checklist is shown in Table 1.
Step 5. Analysis and composition of findings
After identifying the SDH, these factors were classified into 4 levels: individual, local, national, and global.
Step 6. Quality control
This stage evaluates the reliability of the results by calculating Cohen’s kappa coefficient. The results are reliable since the value of this index lies in the valid range (Equation 1, 2 and 3).
1. Agreements observed=(27+0)/31=0.87
2. Chance agreements=(27/31)×(31/31)×(4/31)×(0/31)=0.00
3. K=(0.87-0.00)/(1-0.00)=0.87
Step 7. Presentation of finding in the form of semantic mapping
The semantic mapping of social determinants of health is presented in Figure 2. The first level is the individual, whose social determinants have 7 subcategories (family status, start a healthy life, early childhood development, social gradient, personal behaviors, spiritual and mental health, and lifetime programs). At the second level, which is local, these factors are in 4 subcategories (biological and chemical environment, physical environment, urban resource infrastructure, and social environment). At the third level, SDH at the national level is categorized into 13 subcategories (health system, demographic factors, national rights, laws and regulations, national policies, economic system, governance and policymaking, historical-geographical conditions, political system, culture, and social values, social system, public security, external factors, and national capital). At the last level, these factors lie at the global level (global governance and management, international cooperation and financial assistance, and other world-class determinants).
Fuzzy delphi process
The Delphi method is an expert group decision-making model [23]. We used the fuzzy Delphi technique algorithm to screen social determinants of health and identify the most important determinants of population health in Iran.
Selecting experts is the first step of the Delphi technique. Based on various studies about the composition panel of the Delphi technique, an effective approach involves a mixture of individuals with diverse expertise [24, 25]. In this study, the expert group includes experts or professionals from the healthcare sector, academia, and government departments.
The panel size for the Delphi technique is a topic of some debate, with divergent views among scholars. Hogarth (1978) proposed that an optimal Delphi panel size ranges from 6 to 12 members, while Clayton (1997) suggested that a panel of 5 to 10 experts with diverse specialties can be adequate [24]. We selected 14 members for the Delphi technique.
Step 1. Collect and fuzzify expert opinions
Different types of Likert scales can be used for gathering experts’ opinions; we used a 7-point scale on the significance of criteria. We display any expert’s opinion as a triangular fuzzy number (l, m, u).
Step 2. Fuzzy aggregation of fuzzified values
In the second step, we calculate the fuzzy average of experts’ opinions. Following the theoretical framework, once a consensus is reached among the panelists in the final round of the Delphi process, the items are evaluated and screened based on their average score.
Step 3. Defuzzification
Defuzzification methods can be complex and numerous, with some simpler techniques, such as averaging fuzzy triangular numbers, being available. This study employs a more sophisticated defuzzification technique, explained as follows [24] (Equation 4):

Step 4. Screening criteria
A threshold should be calculated after the defuzzification of values for screening items. In this study, the threshold is 0.7. If the crisp value of defuzzification is larger than 0.7, the criterion is followed. If the criterion is less than 0.7, it is removed.
3. Results
After screening items, at the individual level: the number of children (0.625) and the number of people present at home (0.694); at the local level: access to fuel resources (0.669), aesthetic elements (0.67), local laws and standards (0.655), social solidarity and cohesion and collective efficiency (0.66), and urban structures such as border agreements (0.6); and at the national level: patent and intellectual property laws (0.694), legal and institutional factors (0.651), climate (0.67), the nature and role of religion (0.673), corporate social responsibility (0.691) and invest in social resources (0.697) are removed. For other items, if the crisp value of defuzzification is larger than 0.7, the criterion is conformed.
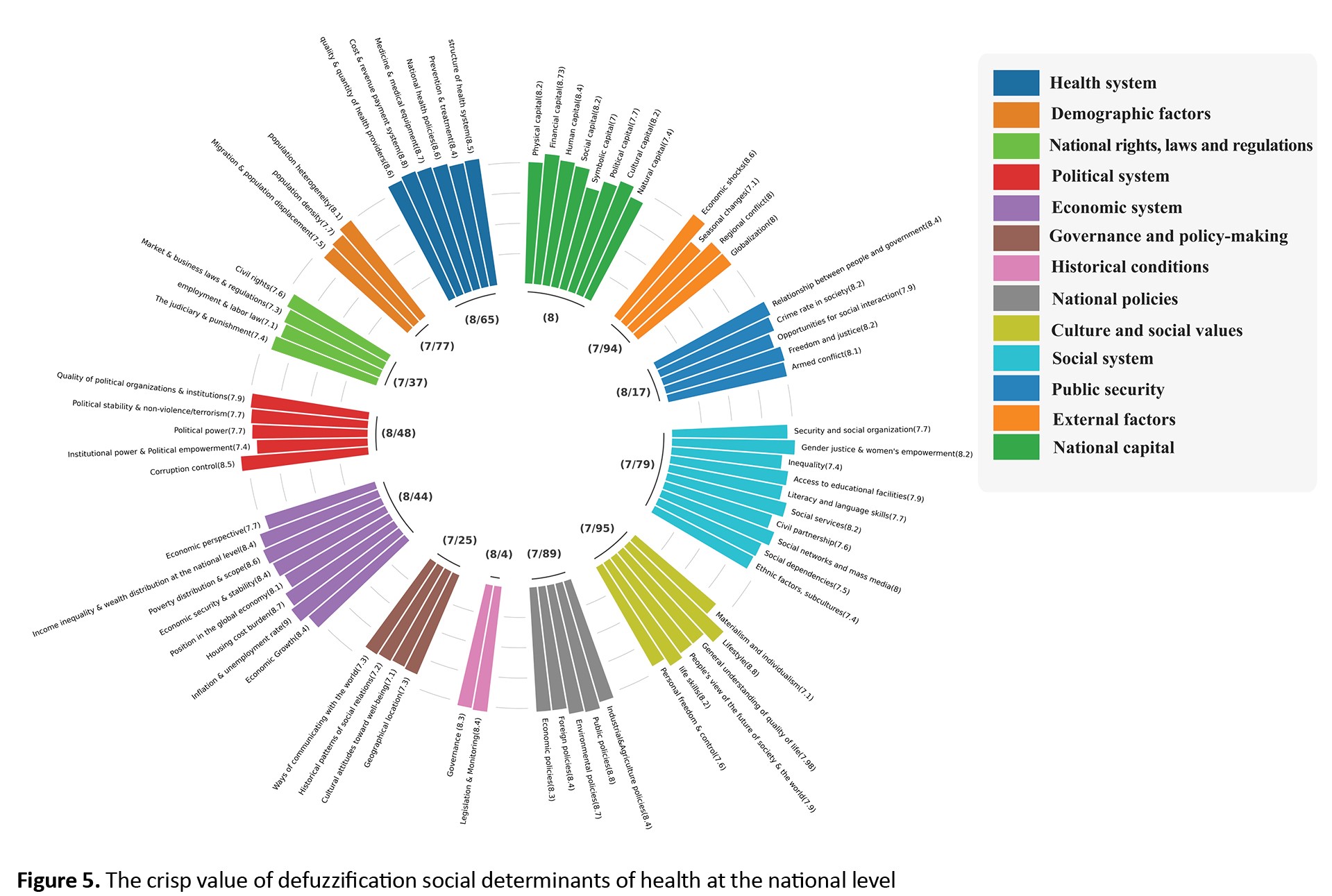
Figures 3, 4 and 5 show the priority of each social determinant of population health in Iran. As seen, social determinants at the individual level (8.2) and national level (8) are more important than the local and global levels. At the individual level, spiritual and mental health (8.48) and individual behaviors (8.45), and at the national level, health system (8.65), national policies (8.48), and economic system (8.44) have the largest crisp value of defuzzification.
Twenty of the most important social determinants of health in Iran are shown in Table 2.

4. Discussion
This study aims to identify the most important determinants of health in Iran. The health system, with its social determinants, is complex due to the many factors and causal relationships between them. In previous studies, qualitative research has been the predominant approach for mapping social determinants of health [26, 27]. Moreover, the complexity of analyzing a multitude of factors in a complex system has limited the scope of many quantitative studies to a single factor, such as immigration policies [5], human environment and habitat [28], and conflict [29]. This article has identified Iran’s most important social determinants of health by combining quantitative and qualitative methods. The results showed that the most important social determinants of health in Iran are as follows: family status (e.g. parental competence), biological and chemical (e.g. types of pollution), spiritual and mental health (e.g. hope, depression, suicide, stress, and anxiety), and social gradient (e.g. economic conditions, education, and training, food security: access to food, food quality). Many studies have been conducted on the influence of individual behaviors on health, and the results show that individual behaviors, such as addiction, diet and exercise, driving behaviors, and the quality of sexual relations, etc., are important factors that determine health [30, 31]. Iranian Legal Medicine Organization stated that addiction deaths in 2022 faced a 15.2% growth compared to the previous year; this year, 5342 people died due to addiction. In a study of 107 addicts whose death information was received, more than 70% had less than a diploma, and almost three-quarters were unemployed. About the housing situation, nearly one-fifth of these people were homeless. About 76% of these people were examined for other diseases during admission, more than half of them (70.4%) had no history of any physical illness, and 91% had no record of any mental illness [32]. Thus, addiction was the main reason for their death. According to the World Health Organization’s report, Iran has many deaths caused by traffic accidents. In general, 186146 people were killed in traffic accidents in the country during 2018-2019. Although the death rate due to traffic accidents has decreased during the study period, it is still unsuitable compared to the global average [33]. According to Erfanpour et al.’s study [34], most accidents leading to death happen to males aged 15-35 years, with low education, and illiterate. Therefore, a large part of traffic accidents occurs due to the individual behavior of drivers. Other factors identified in this research, such as social gradients (employment, housing, income, etc.), spiritual and mental health, and life-long plans (immigration, divorce, etc.), are also consistent with the results of previous studies [11, 35, 36, 37]. In the research of Zablei and Sanai Nasab [38], employment, psychological and community support, environmental factors such as urbanization and social gradients, and in another study by Zablei et al. [39], psychological factors, social environment, behavioral factors, and social gradients were identified as some of the most important determinants of health inequality.
In the field of environmental and chemical factors, previous research confirms the results of this study. For example, Moradi-asl et al. studied the poisoning and mortality rate using poisons, drugs, and chemicals in Meshkinshahr City, Iran. This study showed that more than 70% of mortality was due to pesticides, indicating their toxicity [40].
Identifying the determinants of population health can reveal the most important policy goals and help policymakers allocate resources optimally to promote population health. With the identification of the most important social determinants of health in this research, future research can assess the status of the social determinants of the population’s health in the model presented in this study, measure the gap between the desired situation and the current situation and identify the desired priorities to improve the situation.
5. Conclusions
Our review shows a considerable increase in the studies focusing on economic and social factors as health determinants. Policies and interventions in various sectors directly and immediately affect social determinants of health. Reviewing the literature on social determinants of health indicates the lack of focus on the effects of policies in different sectors at all levels on health. Thus, mapping the social determinants of health in this study provides policymakers with a comprehensive view of policy interventions that improve population health. The proposed mapping categorizes the most important social and economic determinants of population health into 4 levels (individual, local, national, and global) with different subcategories for each level to reveal the impact of other government sectors on the health sector.
Public health affects the population through social determinants of health, and policymakers can improve the health status by controlling and regulating these factors. Furthermore, identifying the determinants of population health can reveal the most important policy goals and help policymakers allocate resources optimally to promote population health. In this article, 20 factors were identified as the most important determinants of population health in Iran. Considering that the health condition and its determinants are different in each country, the determinants specified in the semantic mapping can be measured for other countries, and based on this, the social determinants with priority for policymakers can be determined.
Study limitations
Determining the importance of social determinants of health by experts can be one of the limitations of the present study. Some errors in data collection, registration, and reporting may have affected the finding, which could not be detected despite quality control efforts. Another serious issue is that an extensive list of factors can lead to longer sessions, potentially reducing participant engagement. This challenge is more significant when multiple participants are involved.
Ethical Considerations
Compliance with ethical guidelines
We received ethical clearance from Tarbiat Modares University (Code: IR.MODARES.REC.1398.223).
Funding
The study was self-funded.
Authors contributions
Conceptualization, methodology, writing, review, and editing: Nafiseh Salehnia and Abbas Assari Arani; Validation and supervision: Alireza Olyaemanesh and Hossein Sadeghi; Formal analysis, investigation, resources, writing-original draft preparation: Nafiseh Salehnia; Project administration: Abbas Assari Arani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to acknowledge and thank all the experts who participated in the study.
References
According to the World Health Organization (WHO), the social determinants of health (SDH) refer to the circumstances effective in individuals’ health outcomes, including the environmental, economic, social, and cultural factors that influence their experiences from birth to old age, as well as the societal structures and processes that shape these conditions [1]. These systems include economic system, culture and social values, governance, and policymaking, national policies and social environment [2], immigrant policies, laws, regulations, institutions, and agencies [3], economic stability, education, neighborhood, and living environment [4], perceived neighborhood crime [5], adjustable housing, sustainable employment, access to healthy food, and quality schools [6].
Public health focused on the physical environment in the late 19th and early 20th centuries. For example, people’s life expectancy increased dramatically by improving the safe drinking water supply, sanitary housing, sewage system, workplace safety, and healthy eating. In the later decades of the 20th century, the focus on access to healthcare led to the further extension of lifespan. In recent decades, studies have increasingly shown how economic and social conditions determine health and how the heterogeneity of health status in various groups is more related to economic and social health factors than health services [7].
In recent decades, empirical and conceptual studies have mainly concentrated on proximal social determinants such as individual traits. Although studying these factors is relatively easy, they are far less critical and controllable for policymakers than macrosocial factors such as tax policies [8, 9]. Public health interventions should address social determinants of health (SDH) to improve population health. Public health has both direct and indirect effects (through social determinants) on population health [10]. Hence, with the emergence of public health, researchers in this field have been more interested in studying the role of social health factors, investigating how social conditions affect health and how to arrange them to improve population health [11]. It is promising for policymakers to identify the social factors affecting health outcomes as their interventions control and change these factors [8]. Many of these health determinants depend on the other sectors outside the health system [2]. Thus, the main issue is the other sectors’ awareness of the effects of their decisions on health and the integration of health goals with other policies by addressing the health determinants in all sectors. Conceptual models can help policymakers better understand the situation and make more appropriate interventions. Despite numerous studies on the health of Iran’s population, they have insufficiently and inadequately examined health’s social and economic determinants. Developing a comprehensive map of the SDH could facilitate a coordinated government response to address health issues and disparities in society.
Determining the importance and prioritization of the determinants of population health can reveal the most important policy goals and help policymakers allocate resources optimally to promote population health. This study aims to answer the following two main questions:
What are the social determinants of population health?
What are the prioritizing social determinants of population health in Iran?
So, first, by analyzing the available scientific sources, the determinants of health at all levels and sections were identified and categorized. It represents a comprehensive picture of these factors via semantic mapping from different perspectives and levels. This semantic mapping allows decision-makers to effectively identify the determinants of population health. In the next stage, experts used the fuzzy Delphi method to determine the most important social determinants of population health in Iran. Determining the most important factors can help policymakers invest appropriately and allocate resources optimally to promote population health.
2. Materials and Methods
This study employs an explanatory-sequential mixed-method study, combining and integrating quantitative and qualitative approaches in a single model [12]. This mixed approach offers a more revealing insight into the research issues and complicated phenomena than either method separately [13]. The mixed method approach is used in this research. The research process is shown in Figure 1. Meta-synthesis
This research employs a meta-synthesis method to map the SDH. The meta-synthesis method is a qualitative research strategy that provides researchers with a systematic approach to combine study and identify hidden themes and analogies. Qualitative syntheses currently encompass a wide variety of methods without established guidelines since they are a relatively recent field of research [14]. We used Sandelowski and Barros’s 7-step approach [15] as follows:
Step 1. Formulating the research question
What are the social determinants of population health?
Step 2. Systematic search
This step searches the keywords including “social determinant of health”, “SDH”, “determinant of health”, and “socioeconomic factor” in the scientific databases, including Google Scholar, ScienceDirect, Springer, Emerald, PubMed, ProQuest, and Scopus published from 2000 to 2020. Searching the keywords offers us the first group of scientific sources, paving the way for searching other related references.
Step 3. Reviewing and screening the references
This step reviews and filters the resources derived in the previous step based on our criteria, including title, abstract, and content (including citation information, the use of other models in the research and repetitiveness, non-clarification of the detected components, and the lack of access to the content).
Step 4. Extracting information from the resources using the qualitative content analysis method
This step uses the qualitative content analysis method to extract the social determinants of health from 58 resources. Since this study aims to identify and categorize all social determinants of health cases, it first investigates the whole text to mark those sections related to social determinants of health according to our initial perception. Then, our predefined codes encrypt the marked parts. Also, new codes are assigned to parts of the text not encrypted according to this marking. Accordingly, this step reviews all the studies and selects the codes related to the keyword to form categories, themes, and subcategories. A part of the qualitative content analysis checklist is shown in Table 1.
Step 5. Analysis and composition of findings
After identifying the SDH, these factors were classified into 4 levels: individual, local, national, and global.
Step 6. Quality control
This stage evaluates the reliability of the results by calculating Cohen’s kappa coefficient. The results are reliable since the value of this index lies in the valid range (Equation 1, 2 and 3).
1. Agreements observed=(27+0)/31=0.87
2. Chance agreements=(27/31)×(31/31)×(4/31)×(0/31)=0.00
3. K=(0.87-0.00)/(1-0.00)=0.87
Step 7. Presentation of finding in the form of semantic mapping
The semantic mapping of social determinants of health is presented in Figure 2. The first level is the individual, whose social determinants have 7 subcategories (family status, start a healthy life, early childhood development, social gradient, personal behaviors, spiritual and mental health, and lifetime programs). At the second level, which is local, these factors are in 4 subcategories (biological and chemical environment, physical environment, urban resource infrastructure, and social environment). At the third level, SDH at the national level is categorized into 13 subcategories (health system, demographic factors, national rights, laws and regulations, national policies, economic system, governance and policymaking, historical-geographical conditions, political system, culture, and social values, social system, public security, external factors, and national capital). At the last level, these factors lie at the global level (global governance and management, international cooperation and financial assistance, and other world-class determinants).
Fuzzy delphi process
The Delphi method is an expert group decision-making model [23]. We used the fuzzy Delphi technique algorithm to screen social determinants of health and identify the most important determinants of population health in Iran.
Selecting experts is the first step of the Delphi technique. Based on various studies about the composition panel of the Delphi technique, an effective approach involves a mixture of individuals with diverse expertise [24, 25]. In this study, the expert group includes experts or professionals from the healthcare sector, academia, and government departments.
The panel size for the Delphi technique is a topic of some debate, with divergent views among scholars. Hogarth (1978) proposed that an optimal Delphi panel size ranges from 6 to 12 members, while Clayton (1997) suggested that a panel of 5 to 10 experts with diverse specialties can be adequate [24]. We selected 14 members for the Delphi technique.
Step 1. Collect and fuzzify expert opinions
Different types of Likert scales can be used for gathering experts’ opinions; we used a 7-point scale on the significance of criteria. We display any expert’s opinion as a triangular fuzzy number (l, m, u).
Step 2. Fuzzy aggregation of fuzzified values
In the second step, we calculate the fuzzy average of experts’ opinions. Following the theoretical framework, once a consensus is reached among the panelists in the final round of the Delphi process, the items are evaluated and screened based on their average score.
Step 3. Defuzzification
Defuzzification methods can be complex and numerous, with some simpler techniques, such as averaging fuzzy triangular numbers, being available. This study employs a more sophisticated defuzzification technique, explained as follows [24] (Equation 4):

Step 4. Screening criteria
A threshold should be calculated after the defuzzification of values for screening items. In this study, the threshold is 0.7. If the crisp value of defuzzification is larger than 0.7, the criterion is followed. If the criterion is less than 0.7, it is removed.
3. Results
After screening items, at the individual level: the number of children (0.625) and the number of people present at home (0.694); at the local level: access to fuel resources (0.669), aesthetic elements (0.67), local laws and standards (0.655), social solidarity and cohesion and collective efficiency (0.66), and urban structures such as border agreements (0.6); and at the national level: patent and intellectual property laws (0.694), legal and institutional factors (0.651), climate (0.67), the nature and role of religion (0.673), corporate social responsibility (0.691) and invest in social resources (0.697) are removed. For other items, if the crisp value of defuzzification is larger than 0.7, the criterion is conformed.
Figures 3, 4 and 5 show the priority of each social determinant of population health in Iran. As seen, social determinants at the individual level (8.2) and national level (8) are more important than the local and global levels. At the individual level, spiritual and mental health (8.48) and individual behaviors (8.45), and at the national level, health system (8.65), national policies (8.48), and economic system (8.44) have the largest crisp value of defuzzification.
Twenty of the most important social determinants of health in Iran are shown in Table 2.

4. Discussion
This study aims to identify the most important determinants of health in Iran. The health system, with its social determinants, is complex due to the many factors and causal relationships between them. In previous studies, qualitative research has been the predominant approach for mapping social determinants of health [26, 27]. Moreover, the complexity of analyzing a multitude of factors in a complex system has limited the scope of many quantitative studies to a single factor, such as immigration policies [5], human environment and habitat [28], and conflict [29]. This article has identified Iran’s most important social determinants of health by combining quantitative and qualitative methods. The results showed that the most important social determinants of health in Iran are as follows: family status (e.g. parental competence), biological and chemical (e.g. types of pollution), spiritual and mental health (e.g. hope, depression, suicide, stress, and anxiety), and social gradient (e.g. economic conditions, education, and training, food security: access to food, food quality). Many studies have been conducted on the influence of individual behaviors on health, and the results show that individual behaviors, such as addiction, diet and exercise, driving behaviors, and the quality of sexual relations, etc., are important factors that determine health [30, 31]. Iranian Legal Medicine Organization stated that addiction deaths in 2022 faced a 15.2% growth compared to the previous year; this year, 5342 people died due to addiction. In a study of 107 addicts whose death information was received, more than 70% had less than a diploma, and almost three-quarters were unemployed. About the housing situation, nearly one-fifth of these people were homeless. About 76% of these people were examined for other diseases during admission, more than half of them (70.4%) had no history of any physical illness, and 91% had no record of any mental illness [32]. Thus, addiction was the main reason for their death. According to the World Health Organization’s report, Iran has many deaths caused by traffic accidents. In general, 186146 people were killed in traffic accidents in the country during 2018-2019. Although the death rate due to traffic accidents has decreased during the study period, it is still unsuitable compared to the global average [33]. According to Erfanpour et al.’s study [34], most accidents leading to death happen to males aged 15-35 years, with low education, and illiterate. Therefore, a large part of traffic accidents occurs due to the individual behavior of drivers. Other factors identified in this research, such as social gradients (employment, housing, income, etc.), spiritual and mental health, and life-long plans (immigration, divorce, etc.), are also consistent with the results of previous studies [11, 35, 36, 37]. In the research of Zablei and Sanai Nasab [38], employment, psychological and community support, environmental factors such as urbanization and social gradients, and in another study by Zablei et al. [39], psychological factors, social environment, behavioral factors, and social gradients were identified as some of the most important determinants of health inequality.
In the field of environmental and chemical factors, previous research confirms the results of this study. For example, Moradi-asl et al. studied the poisoning and mortality rate using poisons, drugs, and chemicals in Meshkinshahr City, Iran. This study showed that more than 70% of mortality was due to pesticides, indicating their toxicity [40].
Identifying the determinants of population health can reveal the most important policy goals and help policymakers allocate resources optimally to promote population health. With the identification of the most important social determinants of health in this research, future research can assess the status of the social determinants of the population’s health in the model presented in this study, measure the gap between the desired situation and the current situation and identify the desired priorities to improve the situation.
5. Conclusions
Our review shows a considerable increase in the studies focusing on economic and social factors as health determinants. Policies and interventions in various sectors directly and immediately affect social determinants of health. Reviewing the literature on social determinants of health indicates the lack of focus on the effects of policies in different sectors at all levels on health. Thus, mapping the social determinants of health in this study provides policymakers with a comprehensive view of policy interventions that improve population health. The proposed mapping categorizes the most important social and economic determinants of population health into 4 levels (individual, local, national, and global) with different subcategories for each level to reveal the impact of other government sectors on the health sector.
Public health affects the population through social determinants of health, and policymakers can improve the health status by controlling and regulating these factors. Furthermore, identifying the determinants of population health can reveal the most important policy goals and help policymakers allocate resources optimally to promote population health. In this article, 20 factors were identified as the most important determinants of population health in Iran. Considering that the health condition and its determinants are different in each country, the determinants specified in the semantic mapping can be measured for other countries, and based on this, the social determinants with priority for policymakers can be determined.
Study limitations
Determining the importance of social determinants of health by experts can be one of the limitations of the present study. Some errors in data collection, registration, and reporting may have affected the finding, which could not be detected despite quality control efforts. Another serious issue is that an extensive list of factors can lead to longer sessions, potentially reducing participant engagement. This challenge is more significant when multiple participants are involved.
Ethical Considerations
Compliance with ethical guidelines
We received ethical clearance from Tarbiat Modares University (Code: IR.MODARES.REC.1398.223).
Funding
The study was self-funded.
Authors contributions
Conceptualization, methodology, writing, review, and editing: Nafiseh Salehnia and Abbas Assari Arani; Validation and supervision: Alireza Olyaemanesh and Hossein Sadeghi; Formal analysis, investigation, resources, writing-original draft preparation: Nafiseh Salehnia; Project administration: Abbas Assari Arani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to acknowledge and thank all the experts who participated in the study.
References
- Andvik C. Social determinants of health in very poor ruralities: Striving and thriving in dire conditions: Is it possible? A qualitative study with women in a poor rural district of Ghana [MSc. Thesis]. Bergen: University of Bergen; 2010. [Link]
- Salehnia N, Assari Arani A, Olyaeemanesh A, Sadeghi Saghdel H. Analysis of casual relationships between social determinants of health in Iran; using fuzzy cognitive map. Journal of Research in Health Sciences, 2022; 22(4):e00566. [Link]
- Wallace SP, Young MT, Rodríguez MA, Brindis CD. A social determinants framework identifying state-level immigrant policies and their influence on health. SSM - Population Health. 2018; 7:100316. [DOI:10.1016/j.ssmph.2018.10.016] [PMID] [PMCID]
- Stefanacci RG, Riddle A. Beyond the medical-assisting with social determinants of health in the drive to value-based care. Geriatric Nursing. 2018; 39(6):709-13. [DOI:10.1016/j.gerinurse.2018.10.011] [PMID]
- Yangyuen S, Songklang S, Mahaweerawat U, Mahaweerawat C. The perceived neighborhood crime and hazardous alcohol use among youth in university of the northeastern Thailand context. Journal of Research in Health Sciences. 2020; 20(4):e00493. [DOI:10.34172/jrhs.2020.33] [PMID] [PMCID]
- Elias RR, Jutte DP, Moore A. Exploring consensus across sectors for measuring the social determinants of health. SSM - Population Health. 2019; 7:100395. [DOI:10.1016/j.ssmph.2019.100395] [PMID] [PMCID]
- Los Angeles County Department of Public health. How social and economic factors affect health. Los Angeles: Los Angeles County Department of Public health; 2013.
- Putnam S, Galea S. Epidemiology and the macrosocial determinants of health. Journal of Public Health Policy. 2008; 29(3):275-89. [DOI:10.1057/jphp.2008.15] [PMID]
- Dean HD, Williams KM, Fenton KA. From theory to action: Applying social determinants of health to public health practice. Public Health Reports. 2013; 128(Suppl 3):1-4. [DOI:10.1177/00333549131286S301] [PMID] [PMCID]
- Shi L, Tsai J, Kao S. Public health, social determinants of health, and public policy. Journal of Medical Sciences, 2009; 29(2):43-59. [Link]
- Galea S. Macrosocial determinants of population health. New York: Springer; 2007. [Link]
- Molina-Azorin JF. Mixed methods research: An opportunity to improve our studies and our research skills. European Journal of Management and Business Economics, 2016; 25(2):37-8. [DOI:10.1016/j.redeen.2016.05.001]
- Mohammadpour A, Sadeghi R, Rezaei M. [Mixed methods research as third methodological movement: Theoretical foundations and practical procedures (Persian)]. Journal of Applied Sociology. 2010; 21(2):77-100. [Link]
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: Systematic analysis and synthesis of qualitative research. Health Technology Assessment, 2011; 15(43):1-164. [DOI:10.3310/hta15430] [PMID]
- Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. New York: Springer; 2007. [Link]
- Hahn RA, Truman BI, Williams DR. Civil rights as determinants of public health and racial and ethnic health equity: Health care, education, employment, and housing in the United States. SSM - Population Health. 2018; 4:17-24. [DOI:10.1016/j.ssmph.2017.10.006] [PMID] [PMCID]
- Bruner C. Screening for social determinants of health: A framework and cross-walk of select screening tools and questions. Social Determinants of Health Issue Brief Series. 2017. [Link]
- Hauck K, Martin S, Smith PC. Priorities for action on the social determinants of health: Empirical evidence on the strongest associations with life expectancy in 54 low-income countries, 1990-2012. Social Science & Medicine . 2016; 167:88-98. [DOI:10.1016/j.socscimed.2016.08.035] [PMID]
- Davis SL, Chapa DW. Social determinants of health: Knowledge to effective action for change. The Journal for Nurse Practitioners. 2015; 11(4):424-9. [DOI:10.1016/j.nurpra.2015.01.029]
- Chimed T. Socioeconomic determinants of noncommunicable disease risk factors in rapidly changing societies: Multi-country analysis of six countries of the former Soviet :union: [PhD dissertation]. Tampere: University of Tampere; 2014. [Link]
- World Health Organization (WHO). Rio political declaration on social determinants of health. Rio de Janeiro: World Conference on Social Determinant of Health; 2011. [Link]
- Wolff J. How should governments respond to the social determinants of health? Preventive Medicine. 2011; 53(4-5):253-5.[DOI:10.1016/j.ypmed.2011.07.008] [PMID]
- Hsueh SL. Assessing the effectiveness of community-promoted environmental protection policy by using a Delphi- uzzy method: A case study on solar power and plain afforestation in Taiwan. Renewable and Sustainable Energy Reviews, 2015; 49:1286-95. [DOI:10.1016/j.rser.2015.05.008]
- Habibi A, Firouzi Jahantigh F, Sarafrazi A. Fuzzy delphi technique for forecasting and screening items. Asian Journal of Research in Business Economics and Management, 2015; 5(2):130-43. [DOI:10.5958/2249-7307.2015.00036.5]
- Hsu YL, Lee CH, Kreng VB. The application of fuzzy delphi method and fuzzy AHP in lubricant regenerative technology selection. Expert Systems with Applications, 2010; 37(1):419-25. [DOI:10.1016/j.eswa.2009.05.068]
- Daghofer D, Edwards P. Toward health equity: A comparative analysis and framework for action. Ottawa: Public Health Agency of Canada; 2009.
- Canadian Council on Social Determinants of Health. A review of frameworks on the determinants of health. Ottawa: Canadian Council on Social Determinants of Health; 2015. [Link]
- Graham H, White PC. Social determinants and lifestyles: Integrating environmental and public health perspectives. Public Health. 2016; 141:270-8. [DOI:10.1016/j.puhe.2016.09.019] [PMID]
- Vahidi R, kousha A, kalantari H, Tabrizi JS. [Social determinants of health and their related organizations in East Azerbaijan (Persian)]. Journal of Health. 2012; 3(4):20-8. [Link]
- Victorian Health Promotion Foundation. Disability and health inequalities in Australia: Addressing the social and economic determinants of mental and physical Health. Carlton South: Victorian Health Promotion Foundation; 2013. [Link]
- Balvardi M, Dehdashti N, Imani Ghoghary Z, Bashiri H, Alavi Arjas F. Prevalence of sexual behaviors among medical students in southeast of Iran. Iranian Journal of Health Sciences, 2022; 10(3):32-43. [DOI:10.18502/jhs.v10i3.10520]
- Roshanpajouh M, Mirkazemi R, Asadi H, Hedayati B. [Assessment of the burden and causes of mortality in compulsory residential drug treatment centers under the supervision of state welfare organization (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology, 2019; 25(2):164-77. [DOI:10.32598/ijpcp.25.2.164]
- Rezazadeh Z, Askarishahi M, Vakili M. [Trend of fetal traffic injuries in Iran from 2009 to 2018 (Persian)]. The Journal of Toloo-e-Behdasht. 2021; 19(6):50-62. [DOI:10.18502/tbj.v19i6.5709]
- Erfanpoor S, Hashemi Nazari SS, Ghadirzadeh MR. [An epidemiology study of fatal road traffic accidents in Khorasan Razavi province in 2011 (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2017; 59(4):261-8. [Link]
- Hoffmann R, Kroger H, Pakpahan E. Pathways between socioeconomic status and health: Does health selection or social causation dominate in Europe? Advances in Life Course Research. 2018; 36:23-36. [DOI:10.1016/j.alcr.2018.02.002]
- Seligman B, Tuljapurkar S, Rehkopf D. Machine learning approaches to the social determinants of health in the health and retirement study. SSM - Population Health. 2017; 4:95-9. [DOI:10.1016/j.ssmph.2017.11.008] [PMID] [PMCID]
- Mahmoodi G, Jahani MA, Naghavian M, Nazari A, Ahmadi N. A study of health-promoting behaviors of medical sciences students of Islamic Azad University of Sari, Iran 2013. Iranian Journal of Health Sciences, 2014; 2(2):52-7. [DOI:10.18869/acadpub.jhs.2.2.52]
- Zaboli R, Sanaeinasab H. [The challenges and solutions for action of social determinants of health in Iran: A qualitative study (Persian)]. Iranian Journal of Health Education and Health Promotion, 2014; 2(1):5-16. [Link]
- Zaboli R, Malmoon Z, Seyedjavadi M, Seyedin H. [Developing a conceptual model of social determinants of health inequalities: A qualitative study (Persian)]. Journal of Health Promotion Management. 2014; 3(4):74-88. [Link]
- Moradi-asl E, Nikookar H, Danandehpor P, Vakili F, Asadyian M, Adham D. Study of mortality rate and poisoning status by using pesticides, drugs, and chemicals in Meshkinshahr, Ardabil province. Iranian Journal of Health Sciences, 2020; 8(1):11-8. [DOI:10.18502/jhs.v8i1.4021]
Type of Study: Original Article |
Subject:
Health
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |