Volume 12, Issue 1 (Winter 2024)
Iran J Health Sci 2024, 12(1): 1-8 |
Back to browse issues page
Ethics code: IR.IAU.B.REC.1399.012
Clinical trials code: 20180714040458N1
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Naghibeiranvand M, Mohseni R, Shafieian G. The Effect of Educational Religious Intervention on Improving Life Expectancy in Cancer Patients Undergoing Chemotherapy: A Randomized Controlled Clinical Trial. Iran J Health Sci 2024; 12 (1) :1-8
URL: http://jhs.mazums.ac.ir/article-1-876-en.html
URL: http://jhs.mazums.ac.ir/article-1-876-en.html
Student Research Committee, Faculty of Nursing and Midwifery, Lorestan University of Medical Sciences, Khorramabad, Iran. , mehranbeiranvandmsc@gmail.com
Full-Text [PDF 1099 kb]
(699 Downloads)
| Abstract (HTML) (2231 Views)
Full-Text: (543 Views)
Introduction
Cancer is one of the significant health problems and diseases in human societies [1]. Cancer is characterized by abnormal cells’ uninhibited and diffuse growth, leading to tumor formation [2]. The latest global statistics released by the World Health Organization (WHO) show that cancer is the second leading cause of death in the world and is responsible for 9.6 million annual deaths in 2018 [3]. The prevalence rates of cancer are 177 people per 10000 people and 140 women per 100000 people. The most prevalent cancers in Iran are breast (12.5%), gastric (10.6%), colon and rectal (9%), and lung (6.1%) [3]. Treatment of cancers includes chemotherapy, which is one of the most common methods of destroying cancer cells. Chemotherapy, along with its benefits, is often associated with toxicity and side effects that can affect the patient’s hope and quality of life [4]. Cancers and the challenges of preventing and treating them are the main issues in the health domain [5]. Medical models alone cannot be sufficient to care for these patients and increase the number of survivors [6]. Side effects of chemotherapy deprive a cancer patient of the ability to enjoy different aspects of life. In the meantime, hope enables people to see their situation and suffering more broadly [7]. Many experts believe that cancer is an incurable disease [8]. Therefore, cancer has adverse effects to different degrees in different aspects of the lives of cancer patients [9]. Although cancer affects mental health, the biggest issue for the patient at this time seems to be despair [10]. These patients often try to express their religious/spiritual needs [11]. Besides, attention to a spiritual/religious aspect of life is important [12].
On the other hand, inner strength, a crucial factor in improving life quality, well-being, and happiness, is associated with the primary sources of health [13]. Moreover, inner strength can facilitate adaptation to new situations, control depression symptoms, and increase disease management self-efficacy [14]. Hope as an inner force can enrich life and enable cancer patients to see beyond their current maladaptation and suffering [15]. Life expectancy is an essential criterion to see the impact of mortality and reflects disease status in a population [16]. Cancer has the most significant effect on life expectancy compared to other chronic diseases. Therefore, most research related to hope is also associated with cancer patients because this disease is a life-threatening factor. Consequently, cancer patients need to engage in a type of psychotherapy that focuses on hope [17].
Numerous studies have shown the positive effect of religion and spirituality on improving the mental health of individuals [18]. As a strong driver of motivation, religion has always played an essential role in human life. Religious interventions give life a purpose, save men from the sense of emptiness, and make them trust God as the best way to deal with stresses and diseases [19]. Other common problems in patients with incurable diseases such as cancer that are not diagnosed for a long time are denial, rejection of the disease, negativity, and despairing beliefs about the disease and life. In other words, cancer is associated with impaired attitudes [20]. According to the results of some studies, religion can be considered an important factor in modulating and reducing the psychological problems of cancer patients [21].
Jim et al. performed a meta-analysis on the effects of religion and physical and mental health on cancer patients. They concluded that religion affects physical and functional well-being and bodily symptoms in cancer patients. These findings demonstrate the importance of religion as part of a comprehensive cancer treatment and care program [22]. Zahra Estakhri et al. found a significant difference between religious beliefs, life expectancy, and quality of life of cancer and non-cancer patients (P<0.01) so that religious beliefs can strengthen the morale of cancer patients, increase their life expectancy and improve their quality of life [23].
Given the rising prevalence of cancer and the lack of research on this topic at the Shahid Rahimi Hospital Oncology Center in Khorramabad, which is a crucial hub for cancer chemotherapy in Lorestan Province, Iran, this study was conducted to determine the effect of religious interventions on life expectancy in patients undergoing chemotherapy.
Materials and Methods
Study participants
The present study was a clinical trial with intervention and control groups performed on 128 cancer patients (64 patients in each group) admitted to the oncology ward of Shahid Rahimi Hospital in Khorramabad during April and May 2017.
In April and May 2017, a clinical trial took place involving 128 cancer patients who were admitted to Shahid Rahimi Hospital’s Oncology Ward in Khorramabad. The study included an intervention group and a control group, each comprising 64 patients.
The researcher, the patients participating, and the data analyzer in the present study were kept blind. The research units were informed to participate in the study but were not informed whether they were in the intervention or control groups. Also, the researcher and the religious expert who held the religious intervention sessions did not know about the type of control or intervention groups of the patients. Finally, the person who analyzed the research data also did not know about the group of patients participating in the research, as coding, intervention, and control group data were provided to him.
Sample size calculation
The sample size was calculated based on the Equation 1:
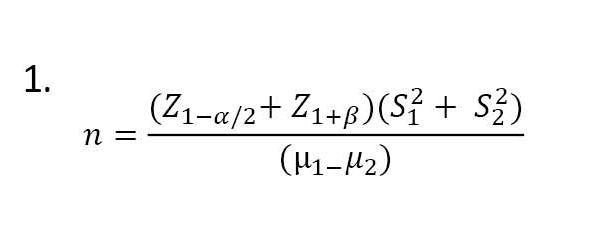
The confidence level was 95%, and the significance level was 0.05. The sampling method was simple random. Each patient who met the inclusion criteria was assigned a number, and the numbers were randomly selected (first, one person for the intervention group and then one person for the control group). The researchers started their research after obtaining permission from the Vice Chancellor for Research of the Islamic Azad University, Khorramabad Branch, receiving a code of ethics, and presenting a license to the relevant officials of Shahid Rahmi Hospital in Khorramabad.
Inclusion and exclusion criteria
The inclusion criteria included patients with cancer, knowledge of their disease, informed consent to participate in the study, performing at least one session of chemotherapy, being Shiite (the second-largest branch of Islam) and Iranian, having literacy and writing, and lacking mental illness and lack of blindness and hearing. The exclusion criteria included having a chronic physical illness other than cancer and a history of taking psychiatric and sedative drugs or other medications.
Data collection instruments
Data collection tools in this study were the demographic self-report questionnaire and Miller’s standard of living questionnaire [24]. The demographic questionnaire included 7 questions about age, sex, level of education, marital status, occupation, duration of illness, and number of chemotherapy sessions. Each person’s score will be between 48 and 240. Scores between 48 and 96 denote low individual hope; scores between 96 and 144 show a person’s average life expectancy, and scores above 144 show a person’s high life expectancy. This questionnaire does not have a cut-off score; the higher the person’s score, the more hope there is. In the study of Shirpoor and Ebrahimi Moghaddam, the total score of the questionnaire was correlated with the criterion score, and its validity coefficient was between 0.64 and 0.87 [25]. The present study used the Cronbach α method to determine the instrument’s reliability, which was 0.81.
Study intervention
Patients undergoing chemotherapy in the chemotherapy ward who met the inclusion criteria were selected and entered the study after providing the consent form. First, the necessary explanations about the purpose of the study, the method of the study, and the beneficial (possible) effects of religious programs on the patient’s motivation for the success of treatment were provided to patients according to information obtained from previous studies. After selecting the sample size, the patients were divided into intervention and control groups. The intervention group sessions were scheduled on Sundays each week (for 3 consecutive weeks) in two intervals (15.45 to 17 and 17 to 18.15). After determining the time of the sessions and conducting the pre-test with Miller’s life examination questionnaire for both intervention and control groups, religious sessions were held with the presence of a religious expert. For the intervention group, training sessions focused on trust in God, good morals, patience, gratitude, and remembrance of God. At the end of the meeting, a group discussion was held on the mentioned issues. After 3 weeks and 6 sessions (completing the intervention), the post-test was done. It should be noted that for the control group, the usual methods (routine medical and nursing care) and for the intervention group, in addition to the usual methods, the religious intervention method was used. To comply with ethical considerations, the prepared package was transferred to a CD and presented to the control group after the study.
Statistical analysis
The collected data were analyzed using SPSS software, version 23. The Kolmogorov-Smirnov test was employed for normal distribution of data. Descriptive and inferential statistical methods and covariance analysis were utilized in this research. Analysis of covariance was used to compare the life expectancy after the intervention in the experimental and control groups.
Results
The Mean±SD ages of the intervention and control groups were 43.46± 8.83 and 47.18±8.61 years, respectively. In both groups, 64 were males (50%) and 64 were females (50%). In the intervention group, 27 patients (42.2%) and in the control group, 24 (37.5%) had university education. In both groups, 111 patients (86.71%) were married. Also, 23 patients (35.9%) were in the intervention group. Economic status was good; in the control group, 25 patients (39.1%) had average economic status. A total of 60 patients (46.87%) had undergone 3-4 sessions of chemotherapy (Table 1).

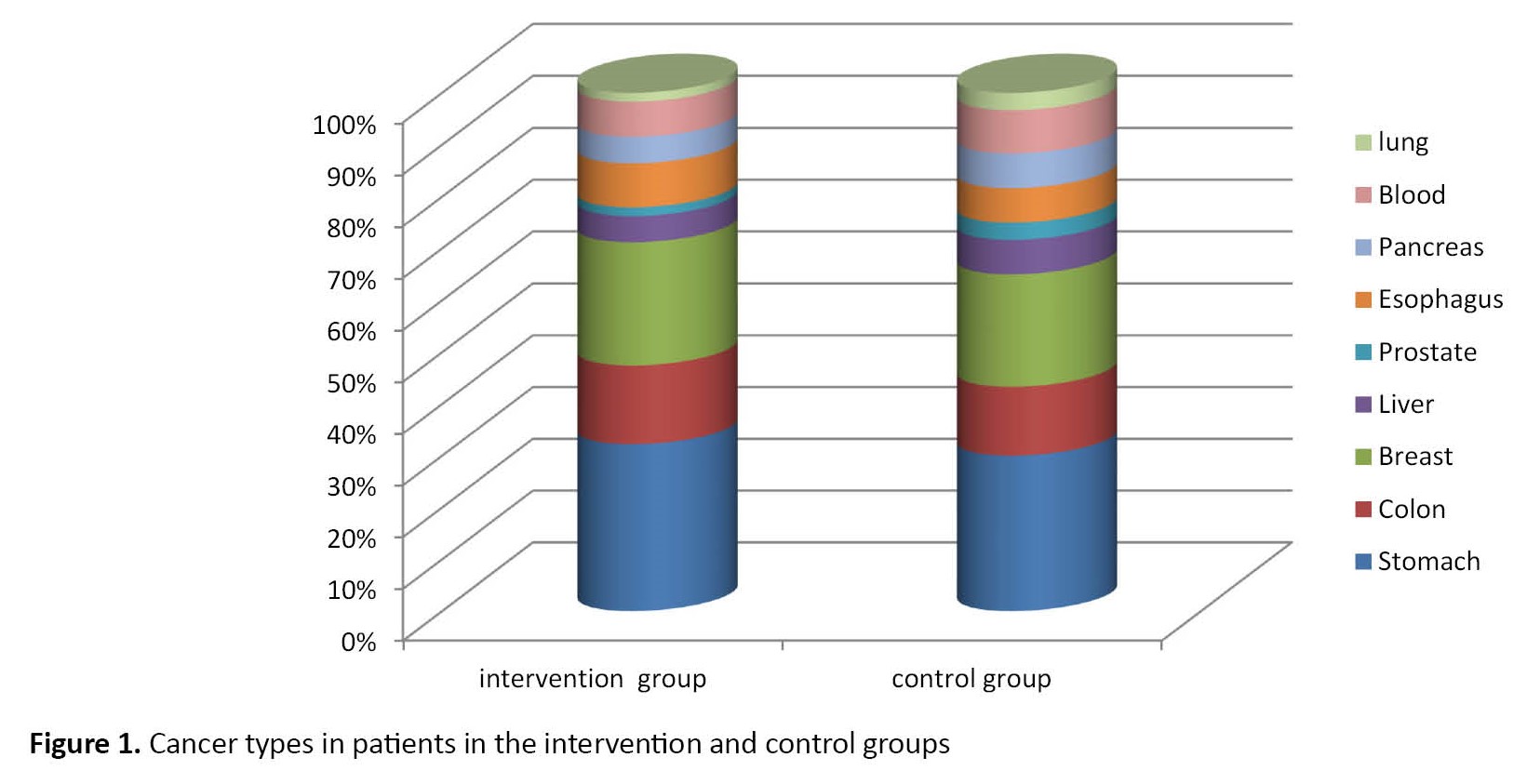
Of all patients participating in the intervention and control groups, the most common types of cancer were gastric (n=37), breast (n=27), and colon (n=17) (Figure 1). The mean life expectancy score of cancer patients in the experimental and control groups was not statistically significant (P<0.05) before the intervention. The covariance analysis results showed a significant difference between the intervention and control groups regarding quality of life (P<0.05). Also, an effect size of 0.832 was obtained, which shows that 83.2% of the variance of changes in life expectancy is predicted by religious intervention (Table 2).

Discussion
Based on the results of the present study, the difference in life expectancy scores after the intervention between the intervention and control groups was significant. The mechanism of this effect seems to be similar to the methods of attention and relaxation because the patient feels support from a superpower when praying, giving the living person a sense of confidence, security, and hope [26]. Therefore, in addition to medical treatments, the attitude of cancer patients towards the disease is improved by emphasizing the importance of religious interventions on how to deal with and adapt to the disease and the conditions that have arisen [27]. Zargani et al. also found that spiritual and religious interventions create a positive attitude toward patients, the environment, and the future. The patients do not consider themselves vulnerable and feel calm in an environment that strengthens coping with living conditions and promotes their mental health [28]. Karimi and Shariatnia also reported that spirituality and religious teachings, through finding the meaning of life, effectively adapt cancer patients to their current situation and affect prayer-based spiritual interventions such as cognitive assessments of the patient. Spiritual interventions create a positive attitude towards life and illness [29]. In the above explanation, it can be mentioned that the common problems in patients with incurable diseases, such as cancer, are denial and non-acceptance of the disease, in other words, negation and despairing beliefs about their disease and existence. Due to the threatening nature of cancer, the diagnosis of this disease may cause many religious crises in the individual [30]. Individuals and groups of researchers worldwide have achieved significant positive results about the impact of faith in God, religion and religious environments, and religious customs on the mental health of individuals, community mental health, and creating peace.
Almost all of these studies agree that the level of anxiety and especially the fear of death in religious settings is lower than in non-religious settings and communities because religious people see life as more meaningful and have no hope of living. They are more, so they experience less death anxiety. In general, spirituality reduces the fear of death, and thus, people with dubious religious views find death more frightening [31]. During chemotherapy, there is a lot of stress on patients, and their recovery process from it affects life expectancy [32].
In the present study, it was shown that religious interventions increase the life expectancy of cancer patients undergoing chemotherapy. Movahedi et al. found that hope can play an essential role in improving the general health of cancer patients and be effective in different stages of the disease [33]. In addition, Alagheband et al. concluded in their study that the higher the life expectancy, the better the response of these patients to the pressures and stresses caused by the treatment of the disease and the therapies offered. They accepted their diseases and acted on them better [34]. The results of Aghajani et al. showed that with increasing hope, the dimensions of physical symptoms, anxiety, social dysfunction, and the level of depression in patients decreased, which is also consistent with the results of the present study [35]. In another study, Aghajani et al. found the importance of paying attention to spiritual modulators, such as prayer behavior and personality traits, such as life expectancy, in shaping positive coping techniques [36].
Rahmanian et al. conducted a study to investigate the effect of group spiritual therapy on the life expectancy and lifestyle of patients with lung cancer [37]. Their study showed that the intervention emphasizing spirituality significantly increases life expectancy and strengthens cancer patients’ mental structure because spiritual issues have protective effects on these patients’ mental well-being, life satisfaction, cognitive changes, and physical health [38]. On the other hand, the results of the study by Luhmann et al. show that people with breast cancer have lower health stiffness scores and hope for recovery than chronic patients [39]. This finding is consistent with the results of the present study because, in both studies, the life expectancy of people with cancer was at a lower level than other people [39]. Vartolomei et al. also concluded that training to overcome helplessness increases life expectancy [40]. In this regard, Arkhodi et al. studied the role of life expectancy in religious beliefs and coronavirus anxiety. They showed that religious beliefs created hope, optimism, meaning, and life purpose. Human beings are mentally and physically effective, and religious people, due to their hope for life, have higher self-care behavior, are better adapted to their disease, and pass the treatment period faster. However, due to a lack of motivation and hope, unsatisfied people make less effort to adhere to their treatment plan and are less adaptable [41]. Spirituality can contribute to more adaptive behaviors in cancer patients, such as giving meaning to life and the present life experience [42]. The findings of the present study showed that the effect of religious teachings and concepts on attitudes toward disease is positive, consistent with the results of Marashi et al. Sajjadieh has developed a positive attitude towards disease in cancer patients [42]. In the explanation of the present findings, it can be said that cancer creates a lot of tension for these patients, and they have to spend long days in the hospital due to treatment, so interventions based on patients’ beliefs can help them a lot. Spatiality raises their hope and leads them to a higher life.
Conclusion
Religious intervention increases the life expectancy of cancer patients undergoing chemotherapy. Therapeutic staff, especially nurses, can, along with other routine care, guide patients undergoing chemotherapy to spirituality and help them to accept the disease and its complications better. It is recommended that training courses on how to care based on (religious) beliefs be held for nurses as in-service training so that nurses become familiar with the principles of caring based on religious intervention and use it in patients’ beds.
Study limitations
One of the limitations of the current study was the existence of religious beliefs in many Iranian men and women, which was beyond the control of the researchers. Another limitation of the present study was that the control group might have received religious or spiritual treatment outside the research environment. However, the patients of the control group were taught that during the study period, apart from medical treatment and routine nursing, they should not receive any psychological or religious counseling. They should inform the researcher if they participated in religious meetings and consultations, including the meetings organized by the research team. In that case, they would be excluded from the study.
Ethical Considerations
Compliance with ethical guidelines
This research was supported by Islamic Azad University, Khorramabad Branch (Code: IR.IAU.B.REC.1399.012) and registered in the Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20180714040458N1). Written informed consent was obtained from the patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and study design: Razia Mohseni; Analysis, data interpretation, writing the original draft: Mehran Naghibeiranvand; Rewriting and editing: Ghazal Shafieian; Final approval: Mehran Naghibeiranvand.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their gratitude to the patients who participated in this study and the staff of the Oncology Department of Shahid Rahimi Hospital in Khorramabad.
References
Cancer is one of the significant health problems and diseases in human societies [1]. Cancer is characterized by abnormal cells’ uninhibited and diffuse growth, leading to tumor formation [2]. The latest global statistics released by the World Health Organization (WHO) show that cancer is the second leading cause of death in the world and is responsible for 9.6 million annual deaths in 2018 [3]. The prevalence rates of cancer are 177 people per 10000 people and 140 women per 100000 people. The most prevalent cancers in Iran are breast (12.5%), gastric (10.6%), colon and rectal (9%), and lung (6.1%) [3]. Treatment of cancers includes chemotherapy, which is one of the most common methods of destroying cancer cells. Chemotherapy, along with its benefits, is often associated with toxicity and side effects that can affect the patient’s hope and quality of life [4]. Cancers and the challenges of preventing and treating them are the main issues in the health domain [5]. Medical models alone cannot be sufficient to care for these patients and increase the number of survivors [6]. Side effects of chemotherapy deprive a cancer patient of the ability to enjoy different aspects of life. In the meantime, hope enables people to see their situation and suffering more broadly [7]. Many experts believe that cancer is an incurable disease [8]. Therefore, cancer has adverse effects to different degrees in different aspects of the lives of cancer patients [9]. Although cancer affects mental health, the biggest issue for the patient at this time seems to be despair [10]. These patients often try to express their religious/spiritual needs [11]. Besides, attention to a spiritual/religious aspect of life is important [12].
On the other hand, inner strength, a crucial factor in improving life quality, well-being, and happiness, is associated with the primary sources of health [13]. Moreover, inner strength can facilitate adaptation to new situations, control depression symptoms, and increase disease management self-efficacy [14]. Hope as an inner force can enrich life and enable cancer patients to see beyond their current maladaptation and suffering [15]. Life expectancy is an essential criterion to see the impact of mortality and reflects disease status in a population [16]. Cancer has the most significant effect on life expectancy compared to other chronic diseases. Therefore, most research related to hope is also associated with cancer patients because this disease is a life-threatening factor. Consequently, cancer patients need to engage in a type of psychotherapy that focuses on hope [17].
Numerous studies have shown the positive effect of religion and spirituality on improving the mental health of individuals [18]. As a strong driver of motivation, religion has always played an essential role in human life. Religious interventions give life a purpose, save men from the sense of emptiness, and make them trust God as the best way to deal with stresses and diseases [19]. Other common problems in patients with incurable diseases such as cancer that are not diagnosed for a long time are denial, rejection of the disease, negativity, and despairing beliefs about the disease and life. In other words, cancer is associated with impaired attitudes [20]. According to the results of some studies, religion can be considered an important factor in modulating and reducing the psychological problems of cancer patients [21].
Jim et al. performed a meta-analysis on the effects of religion and physical and mental health on cancer patients. They concluded that religion affects physical and functional well-being and bodily symptoms in cancer patients. These findings demonstrate the importance of religion as part of a comprehensive cancer treatment and care program [22]. Zahra Estakhri et al. found a significant difference between religious beliefs, life expectancy, and quality of life of cancer and non-cancer patients (P<0.01) so that religious beliefs can strengthen the morale of cancer patients, increase their life expectancy and improve their quality of life [23].
Given the rising prevalence of cancer and the lack of research on this topic at the Shahid Rahimi Hospital Oncology Center in Khorramabad, which is a crucial hub for cancer chemotherapy in Lorestan Province, Iran, this study was conducted to determine the effect of religious interventions on life expectancy in patients undergoing chemotherapy.
Materials and Methods
Study participants
The present study was a clinical trial with intervention and control groups performed on 128 cancer patients (64 patients in each group) admitted to the oncology ward of Shahid Rahimi Hospital in Khorramabad during April and May 2017.
In April and May 2017, a clinical trial took place involving 128 cancer patients who were admitted to Shahid Rahimi Hospital’s Oncology Ward in Khorramabad. The study included an intervention group and a control group, each comprising 64 patients.
The researcher, the patients participating, and the data analyzer in the present study were kept blind. The research units were informed to participate in the study but were not informed whether they were in the intervention or control groups. Also, the researcher and the religious expert who held the religious intervention sessions did not know about the type of control or intervention groups of the patients. Finally, the person who analyzed the research data also did not know about the group of patients participating in the research, as coding, intervention, and control group data were provided to him.
Sample size calculation
The sample size was calculated based on the Equation 1:
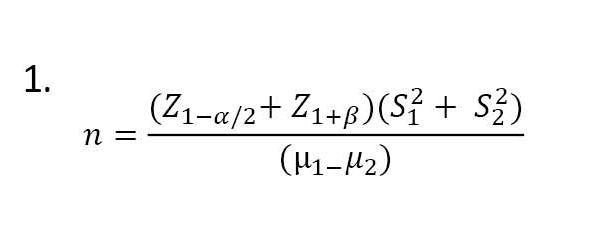
The confidence level was 95%, and the significance level was 0.05. The sampling method was simple random. Each patient who met the inclusion criteria was assigned a number, and the numbers were randomly selected (first, one person for the intervention group and then one person for the control group). The researchers started their research after obtaining permission from the Vice Chancellor for Research of the Islamic Azad University, Khorramabad Branch, receiving a code of ethics, and presenting a license to the relevant officials of Shahid Rahmi Hospital in Khorramabad.
Inclusion and exclusion criteria
The inclusion criteria included patients with cancer, knowledge of their disease, informed consent to participate in the study, performing at least one session of chemotherapy, being Shiite (the second-largest branch of Islam) and Iranian, having literacy and writing, and lacking mental illness and lack of blindness and hearing. The exclusion criteria included having a chronic physical illness other than cancer and a history of taking psychiatric and sedative drugs or other medications.
Data collection instruments
Data collection tools in this study were the demographic self-report questionnaire and Miller’s standard of living questionnaire [24]. The demographic questionnaire included 7 questions about age, sex, level of education, marital status, occupation, duration of illness, and number of chemotherapy sessions. Each person’s score will be between 48 and 240. Scores between 48 and 96 denote low individual hope; scores between 96 and 144 show a person’s average life expectancy, and scores above 144 show a person’s high life expectancy. This questionnaire does not have a cut-off score; the higher the person’s score, the more hope there is. In the study of Shirpoor and Ebrahimi Moghaddam, the total score of the questionnaire was correlated with the criterion score, and its validity coefficient was between 0.64 and 0.87 [25]. The present study used the Cronbach α method to determine the instrument’s reliability, which was 0.81.
Study intervention
Patients undergoing chemotherapy in the chemotherapy ward who met the inclusion criteria were selected and entered the study after providing the consent form. First, the necessary explanations about the purpose of the study, the method of the study, and the beneficial (possible) effects of religious programs on the patient’s motivation for the success of treatment were provided to patients according to information obtained from previous studies. After selecting the sample size, the patients were divided into intervention and control groups. The intervention group sessions were scheduled on Sundays each week (for 3 consecutive weeks) in two intervals (15.45 to 17 and 17 to 18.15). After determining the time of the sessions and conducting the pre-test with Miller’s life examination questionnaire for both intervention and control groups, religious sessions were held with the presence of a religious expert. For the intervention group, training sessions focused on trust in God, good morals, patience, gratitude, and remembrance of God. At the end of the meeting, a group discussion was held on the mentioned issues. After 3 weeks and 6 sessions (completing the intervention), the post-test was done. It should be noted that for the control group, the usual methods (routine medical and nursing care) and for the intervention group, in addition to the usual methods, the religious intervention method was used. To comply with ethical considerations, the prepared package was transferred to a CD and presented to the control group after the study.
Statistical analysis
The collected data were analyzed using SPSS software, version 23. The Kolmogorov-Smirnov test was employed for normal distribution of data. Descriptive and inferential statistical methods and covariance analysis were utilized in this research. Analysis of covariance was used to compare the life expectancy after the intervention in the experimental and control groups.
Results
The Mean±SD ages of the intervention and control groups were 43.46± 8.83 and 47.18±8.61 years, respectively. In both groups, 64 were males (50%) and 64 were females (50%). In the intervention group, 27 patients (42.2%) and in the control group, 24 (37.5%) had university education. In both groups, 111 patients (86.71%) were married. Also, 23 patients (35.9%) were in the intervention group. Economic status was good; in the control group, 25 patients (39.1%) had average economic status. A total of 60 patients (46.87%) had undergone 3-4 sessions of chemotherapy (Table 1).

Of all patients participating in the intervention and control groups, the most common types of cancer were gastric (n=37), breast (n=27), and colon (n=17) (Figure 1). The mean life expectancy score of cancer patients in the experimental and control groups was not statistically significant (P<0.05) before the intervention. The covariance analysis results showed a significant difference between the intervention and control groups regarding quality of life (P<0.05). Also, an effect size of 0.832 was obtained, which shows that 83.2% of the variance of changes in life expectancy is predicted by religious intervention (Table 2).

Discussion
Based on the results of the present study, the difference in life expectancy scores after the intervention between the intervention and control groups was significant. The mechanism of this effect seems to be similar to the methods of attention and relaxation because the patient feels support from a superpower when praying, giving the living person a sense of confidence, security, and hope [26]. Therefore, in addition to medical treatments, the attitude of cancer patients towards the disease is improved by emphasizing the importance of religious interventions on how to deal with and adapt to the disease and the conditions that have arisen [27]. Zargani et al. also found that spiritual and religious interventions create a positive attitude toward patients, the environment, and the future. The patients do not consider themselves vulnerable and feel calm in an environment that strengthens coping with living conditions and promotes their mental health [28]. Karimi and Shariatnia also reported that spirituality and religious teachings, through finding the meaning of life, effectively adapt cancer patients to their current situation and affect prayer-based spiritual interventions such as cognitive assessments of the patient. Spiritual interventions create a positive attitude towards life and illness [29]. In the above explanation, it can be mentioned that the common problems in patients with incurable diseases, such as cancer, are denial and non-acceptance of the disease, in other words, negation and despairing beliefs about their disease and existence. Due to the threatening nature of cancer, the diagnosis of this disease may cause many religious crises in the individual [30]. Individuals and groups of researchers worldwide have achieved significant positive results about the impact of faith in God, religion and religious environments, and religious customs on the mental health of individuals, community mental health, and creating peace.
Almost all of these studies agree that the level of anxiety and especially the fear of death in religious settings is lower than in non-religious settings and communities because religious people see life as more meaningful and have no hope of living. They are more, so they experience less death anxiety. In general, spirituality reduces the fear of death, and thus, people with dubious religious views find death more frightening [31]. During chemotherapy, there is a lot of stress on patients, and their recovery process from it affects life expectancy [32].
In the present study, it was shown that religious interventions increase the life expectancy of cancer patients undergoing chemotherapy. Movahedi et al. found that hope can play an essential role in improving the general health of cancer patients and be effective in different stages of the disease [33]. In addition, Alagheband et al. concluded in their study that the higher the life expectancy, the better the response of these patients to the pressures and stresses caused by the treatment of the disease and the therapies offered. They accepted their diseases and acted on them better [34]. The results of Aghajani et al. showed that with increasing hope, the dimensions of physical symptoms, anxiety, social dysfunction, and the level of depression in patients decreased, which is also consistent with the results of the present study [35]. In another study, Aghajani et al. found the importance of paying attention to spiritual modulators, such as prayer behavior and personality traits, such as life expectancy, in shaping positive coping techniques [36].
Rahmanian et al. conducted a study to investigate the effect of group spiritual therapy on the life expectancy and lifestyle of patients with lung cancer [37]. Their study showed that the intervention emphasizing spirituality significantly increases life expectancy and strengthens cancer patients’ mental structure because spiritual issues have protective effects on these patients’ mental well-being, life satisfaction, cognitive changes, and physical health [38]. On the other hand, the results of the study by Luhmann et al. show that people with breast cancer have lower health stiffness scores and hope for recovery than chronic patients [39]. This finding is consistent with the results of the present study because, in both studies, the life expectancy of people with cancer was at a lower level than other people [39]. Vartolomei et al. also concluded that training to overcome helplessness increases life expectancy [40]. In this regard, Arkhodi et al. studied the role of life expectancy in religious beliefs and coronavirus anxiety. They showed that religious beliefs created hope, optimism, meaning, and life purpose. Human beings are mentally and physically effective, and religious people, due to their hope for life, have higher self-care behavior, are better adapted to their disease, and pass the treatment period faster. However, due to a lack of motivation and hope, unsatisfied people make less effort to adhere to their treatment plan and are less adaptable [41]. Spirituality can contribute to more adaptive behaviors in cancer patients, such as giving meaning to life and the present life experience [42]. The findings of the present study showed that the effect of religious teachings and concepts on attitudes toward disease is positive, consistent with the results of Marashi et al. Sajjadieh has developed a positive attitude towards disease in cancer patients [42]. In the explanation of the present findings, it can be said that cancer creates a lot of tension for these patients, and they have to spend long days in the hospital due to treatment, so interventions based on patients’ beliefs can help them a lot. Spatiality raises their hope and leads them to a higher life.
Conclusion
Religious intervention increases the life expectancy of cancer patients undergoing chemotherapy. Therapeutic staff, especially nurses, can, along with other routine care, guide patients undergoing chemotherapy to spirituality and help them to accept the disease and its complications better. It is recommended that training courses on how to care based on (religious) beliefs be held for nurses as in-service training so that nurses become familiar with the principles of caring based on religious intervention and use it in patients’ beds.
Study limitations
One of the limitations of the current study was the existence of religious beliefs in many Iranian men and women, which was beyond the control of the researchers. Another limitation of the present study was that the control group might have received religious or spiritual treatment outside the research environment. However, the patients of the control group were taught that during the study period, apart from medical treatment and routine nursing, they should not receive any psychological or religious counseling. They should inform the researcher if they participated in religious meetings and consultations, including the meetings organized by the research team. In that case, they would be excluded from the study.
Ethical Considerations
Compliance with ethical guidelines
This research was supported by Islamic Azad University, Khorramabad Branch (Code: IR.IAU.B.REC.1399.012) and registered in the Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20180714040458N1). Written informed consent was obtained from the patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and study design: Razia Mohseni; Analysis, data interpretation, writing the original draft: Mehran Naghibeiranvand; Rewriting and editing: Ghazal Shafieian; Final approval: Mehran Naghibeiranvand.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their gratitude to the patients who participated in this study and the staff of the Oncology Department of Shahid Rahimi Hospital in Khorramabad.
References
- Pudkasam S, Tangalakis K, Chinlumprasert N, Apostolopoulos V, StojanovskaL. Breast cancer and exercise: The role of adiposity and immune markers. Maturitas. 2017; 105:16-22. [DOI:10.1016/j.maturitas.2017.04.022] [PMID]
- Merino Bonilla JA,TorresTabaneraM, Ros Mendoza LH. Breast cancer in the 21st century: From early detection to new therapies. Radiologia. 2017; 59(5):368-79. [DOI:10.1016/j.rx.2017.06.003] [PMID]
- Hasani J, Emamverdi F. [The effectiveness of mindfulness based group cognitive therapy on assertiveness of women with breast cancer (Persian)]. Ebnesina. 2017; 19(2):21-7. [Link]
- Moghimian M, Salmani F. [The study of correlation between spiritual well- being and hope in cancer patints referring to Seyyedo Shohada training -therapy center of Isfahan University of Medical Sciences, 2010 (Persian)]. Qom University of Medical Sciences Journal. 2012; 6(3):40-5. [Link]
- Bodai BI, Tuso P. Breast cancer survivorship: A comprehensive review of long-term medical issues and lifestyle recommendations. The Permanente Journal. 2015; 19(2):48-79. [DOI:10.7812/TPP/14-241] [PMID]
- Ebrahimipour H, Vejdani M, Taghipour A, Heidarabadi AB, Molavi Y. [Spiritual health in cancer patients at OMID hospital affiliated with Mashhad University of Medical Sciences-2012 (Persian)]. Journal of Reaserch on Religion & Health. 2015; 1(2):3-9. [Link]
- Bijari H, Ghanbari HashemAbadi BA, Aghamohammadian Sherbaf HR, Homayi Shandiz F. [Effects of hope- based group therapy on the promotion of hope in women with breast cancer (Persian)]. Foundations of Education. 2009; 10(1):172- 84. [DOI:10.22067/FE.V10I1.12781]
- Ranjbar F, Beirami A, Azizi SH, Zarei Sh, Mousavifard Z. [The effect of chemotherapy on the quality of life of cancer patients (Persian)].Paper presented at: Avan first annual student congress. 23 April 2020; Dezful, Iran. [Link]
- Khodaveirdyzadeh R, Rahimi R, Rahmani A, Ghahramanian A, Kodayari N, Eivazi J. Spiritual/religious coping strategies and their relationship with illness adjustment among Iranian breast cancer patients. Asian Pacific Journal of Cancer Prevention. 2016; 17(8):4095-9. [PMID]
- Drake K. Quality of life for cancer patients: From diagnosis to treatment and beyond. Nursing Management Journal. 2012; 43(2):20-5. [DOI:10.1097/01.NUMA.0000410865.48922.18] [PMID]
- Purnell JQ, Andersen BL, Wilmot JP. Religious practice and spirituality in the psychological adjustment of survivors of breast cancer. Counseling and Values. 2009; 53(3):165. [DOI:10.1002/j.2161-007X.2009.tb00123.x] [PMID]
- Lissoni P, Messina G, Parolini D, Balestra A, Brivio F, Fumagalli L, et al. A spiritual approach in the treatment of cancer: Relation between faith score and response to chemotherapy in advanced non-small cell lung cancer patients. In Vivo. 2008; 22(5):577-81. [PMID]
- Alpers LM, Helseth S, Bergbom I. Experiences of inner strength in critically ill patients-a hermeneutical approach. Intensive and Critical Care Nursing. 2012; 28(3):150-8. [DOI:10.1016/j.iccn.2011.10.004] [PMID]
- Nygren B, Norberg A, Lundman B. Inner strength as disclosed in narratives of the oldest old. Qualitative Health Research. 2007; 17(8):1060-73. [DOI:10.1177/1049732307306922] [PMID]
- Moghadamfar N, Amraei R, Asadi F, Amani O. [The efficacy of Acceptance and Commitment Therapy (ACT) on Hope and Psychological Well-being in Women with Breast Cancer under Chemotherapy (Persian)]. Iranian Journal of Psychiatric Nursing. 2018; 6(5):1-7. [Link]
- Mansano-Schlosser TC, Ceolim MF, Valerio TD. Poor sleep quality, depression and hope before breast cancer surgery. Applied Nursing Research.2017; 34:7-11. [DOI:10.1016/j.apnr.2016.11.010] [PMID]
- Pourfaraj M, Rezazadeh H. [Effectiveness of positive therapy on happiness and hope in cancer Patients (Persian)]. Counseling Culture and Psychotherapy. 2018; 9(33):119-36. [Link]
- Newton AT, McIntosh DN. Specific religious beliefs in a cognitive appraisal model of stress and coping. International Journal for the Psychology of Religion. 2010; 20(1):39-58. [DOI:10.1080/10508610903418129]
- Neissi AK, Karamalian H, Homaei R. [The effect of religious cognitive - behavioral group training on mental health of infertility couples in Esfahan (Persian)]. Family Counseling and Psychotherapy. 2012; 2(2):151-62. [Link]
- Sepahmansour M, Katebi M. [Comparison of health hardness and life expectancy in patients with diabetes and breast cancer (Persian)]. Health Psychology. 2019; 8(31):155-68. [Link]
- Valeberg BT, Grov EK. Symptoms in the cancer patient: Of importance for their caregivers’ quality of life and mental health? European Journal Oncology Nursing. 2013; 17(1):46-51. [DOI:10.1016/j.ejon.2012.01.009] [PMID]
- Jim HS, Pustejovsky JE, Park CL, Danhauer SC, Sherman AC, Fitchett G, et al. Religion, spirituality, and physical health in cancer patients: a meta-analysis. Cancer. 2015; 121(21):3760-8. [DOI:10.1002/cncr.29353] [PMID]
- Estakhri Z, Tajikzadeh F, Kazemi SA. [Comparison of the role of religious beliefs in hopefulness and quality of life among cancer and non-cancer patients in Shiraz, Iran (Persian)]. Religion and Health. 2016; 4(2):1-11. [Link]
- Miller JF, Powers MJ. Development of an instrument to measure hope. Nursing Research. 1988; 37(1):6-10. [DOI:10.1097/00006199-198801000-00002] [PMID]
- Shirpoor AH, EbrahimimoghadamH. [The effectiveness of life skills training on marital satisfaction and life expectancy of people with AIDS (Persian)]. Journal of Psychology New Ideas. 2017; 1(1):21-8. [Link]
- Kruizinga R, Hartog ID, Jacobs M, Daams JG, Scherer-Rath M, Schilderman JB, et al. The effect of spiritual interventions addressing existential themes using a narrative approach on quality of life of cancer patients: A systematic review and meta-analysis. Psychooncology. 2016; 25(3):253-65. [DOI:10.1002/pon.3910] [PMID]
- Yektayi M. [Pleasure of illness in the light of the wisdom of illness from the perspective of SahifehSajjadieh (Persian)]. Daneshvar Medicine. 2011; 18(92):35-42. [Link]
- Zargani A, Nasiri M, Hekmat K, Abbaspour Z, Vahabi S. A survey on the relationship between religiosity and quality of life in patients with breast cancer: A study in Iranian Muslims. Asia-Pacific Journal of Oncology Nursing. 2018; 5(2):217-22. [DOI:10.4103/apjon.apjon_65_17] [PMID]
- Karimi M, Shariatniya K. [The effectiveness of spirituality therapy on the quality of life of cancer women in Tehran (Persian)]. Nursing and Midwifery Journal. 2017; 15(2):106-18. [Link]
- Zakavi A, Marzband R. [Study of instructors’ spiritual factors in medical science education by emphasizing on revealed teachings (Persian)]. Journal of Religion and Health. 2014; 1(1):34-47. [Link]
- Pargament KI. Spiritually integrated psychotherapy: Understanding and addressing the sacred. New York: Guilford Press; 2011. [Link]
- Mogadam N, Amraae R, Asadi F, Amani O. [The efficacy of Acceptance and Commitment Therapy (ACT) on hope and psychological well-being in women with breast cancer under chemotherapy (Persian)]. Iranian Journal of Psychology Nursing. 2018; 6(5):1-8. [Link]
- Movahedi M, Movahedi Y, Farhadi A. [Effect of hope therapy training on life expectancy and general health in cancer patients (Persian)]. Journal of Holistic Nursing and Midwifery. 2015; 25(2):84-92. [Link]
- Alagheband M, Servat F, Zarepour F. [Investigation of the relationship between quality of life and life expectancy in patients with breast cancer (Persian)]. The Journal of Toloo-e-Behdasht. 2016; 15(2):175-85. [Link]
- Aghajani MJ, Akbari B. MirarzgarMS. [The relationship of praying and hardeniss with mental health (Persian)]. Paper presented at: 2th International Congress on Religious culture and Thought. 22 October 2015; Qom, Iran.
- Aghajani MJ, Akbari B. [Relationship of praying and life expectancy with general health of the women suffering from breast cancer (Persian)]. Religion and Health. 2017; 5(1):1-10. [Link]
- Rahmanian M, MoeinSamadani M, Oraki M. [Effect of spirituality group therapy on life expectancy and life style’s improvement of breath cancer patients (Persian)]. Biannual Journal of Applied Counseling. 2017; 7(1):101-14. [Link]
- Luhmann M, Necka EA, Schönbrodt FD, Hawkley LC. Is valuing happiness associated with lowerwell-being? A factor-level analysis using the Valuing Happiness Scale? Journal of Research in Personality. 2016; 60:46-50. [DOI:10.1016/j.jrp.2015.11.003] [PMID]
- Vartolomei L, Ferro M, Mirone V, Shariat SF, Vartolomei MD. Systematic review: Depression and anxiety prevalence in bladder cancer patients. Bladder Cancer. 2018; 4(3):319-26. [DOI:10.3233/BLC-180181] [PMID]
- Arkhodighalenoei M, Haghayeghi M, SaeidiRezvani T. [The mediating role of hope in the relationship between religious beliefs and corona virus disease anxiety (Persian)]. Counseling Culture & Psychotherapy. 2021; 12(47):307-28. [Link]
- Khodabakhshi-Koolaee A, Farhangi D. [Relationship of spiritual experiences and hope with living in present among men with cancer in Tehran (Persian)]. Journal of Pizhūhishdardīnvasalāmat. 2019; 5(2):75-88. [Link]
- Marashi S A, sharifi Rigi A, Hamid N. [The efficacy of spiritual/religious psychotherapy-emphasizing the importance of 15th and 23th Prayers of SahifehSajjadiyeh-on quality of life and attitude toward disease in cancer patients in Ahvaz City (Persian)]. Iranian Journal of Psychiatric Nursing. 2018; 6(5):34-41. [Link]
Type of Study: Original Article |
Subject:
Nursing
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |