Volume 12, Issue 1 (Winter 2024)
Iran J Health Sci 2024, 12(1): 17-26 |
Back to browse issues page
Ethics code: IR.KUMS.50002754
Clinical trials code: NA
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezaei S, Chehri A, Hosseini S S, Arefi M, Amiri H. Associations of Sleep Problems and Self-regulation With Interpersonal Aggression Among Healthcare Workers. Iran J Health Sci 2024; 12 (1) :17-26
URL: http://jhs.mazums.ac.ir/article-1-894-en.html
URL: http://jhs.mazums.ac.ir/article-1-894-en.html
Department of Psychology, Faculty of Literature and Humanities, Kermanshah Branch, Islamic Azad University, Kermanshah, Iran. , azitachehri@yahoo.com
Full-Text [PDF 847 kb]
(613 Downloads)
| Abstract (HTML) (1776 Views)
Full-Text: (528 Views)
Introduction
Healthcare workers, due to their continuing workplace challenges and job burnout (about 30% to 60% affected) [1], are a community vulnerable to mental health problems and maladaptive behaviors such as aggression [2]. Although the research body in the past mainly focused on workplace violence against health workers [3], aggression towards clients and patients is also common in one-third of healthcare workers [2]. Aggression is an instinctive behavior that can be disproportionate or proportionate, depending on the situation [4]. Proportionate aggression is an adaptive behavior subject to social values, whereas disproportionate or extreme aggression is maladaptive, occurring in the face of actual or perceived risk [4]. Disproportionate aggression includes four categories: Anger, hostility, verbal aggression, and physical aggression [5]. Lifetime aggression is also prevalent in up to 80% of adult populations across cultures [6, 7, 8] and about 68% in Iranian adults [9, 10, 11].
Aggressive behaviors bear many consequences, including emotional problems, physical injuries, academic or work inability, psychosomatic complaints, chronic physical disability, and mortality [12, 13]. Etiological studies are continuously trying to identify risk factors for aggression to facilitate the delivery of therapeutic interventions [14]. However, a better understanding and identification of the biopsychosocial factors associated with aggression can help formulate strategies and prevent it [15]. A fresh study classified risk factors for aggression into three general categories: Cortical thickness, personality pathology, and trauma exposure [14]. Nevertheless, aggression is a complex phenomenon affected by multiple risk factors, such as sociodemographic factors [10, 11, 15], physical illness and medication [10, 16], mental health conditions [15, 17], and sleep problems [18, 19, 20].
Sleep problems, which are included in the list of potential risk factors for the manifestation of aggressive behaviors [18, 19, 20], have a wide range of sleep disorders. However, the three categories of insomnia, sleep apnea, and poor sleep quality are among the most important sleep problems. Insomnia is characterized by persistent difficulty with sleep initiation, maintenance, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep [21]. Sleep apnea, also known as obstructive sleep apnea, is a sleep disorder in which periods of stopped breathing or shallow breathing occur more frequently during sleep. Each break lasts from a few seconds to a few minutes and occurs several times a night [22]. Poor sleep quality is a more general sleep disorder that includes several problematic components in subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping pills, and daytime dysfunction [23]. A meta-analytic review estimated the overall prevalence of sleep disorders to be 50% in Iran [24]. Sleep disorders are also common problems among healthcare workers, and their prevalence reaches about 80% [25].
Although cross-sectional and longitudinal associations between sleep problems and aggression are reported by some review studies [19, 20, 26, 27], other studies have attempted to identify protective factors for aggression, such as reading, regular physical exercise, sexual satisfaction, financial management, social network, intimate relationship, empathy, coping, self-control, emotion regulation, and self-regulation [10, 28-33]. Self-regulation is a multidimensional construct that includes cognitive, motivational-emotional, and physiological processes affecting the active control of goal-directed actions [34]. Self-regulation plays an active role in some systems, including active control, initiation, moderation, continuity, and coordination [34]. Many studies have reported higher levels of aggression in individuals with poor self-regulatory mechanisms [29, 31, 32]. The results of some studies, but not in Iran, support the role of self-regulation and some similar mechanisms in managing the aggressive behavior of health workers [2, 35, 36].
In addition to direct associations of sleep disorders and self-regulation with aggressive behaviors in health workers [2, 25, 35, 36, 37], the results of several studies specifically show that emotional self-regulation also mediates the effects of sleep problems on aggression [28, 29, 30]. However, previous studies on the protective role of self-regulation for aggression caused by sleep problems are limited in several aspects. First, these studies only reported the associations between sleep quality, deprivation, and aggression. Therefore, other sleep problems, such as sleep apnea and insomnia symptoms, have been neglected. Second, some studies did not include all aggression subscales, including anger, hostility, verbal aggression, and physical aggression. Third, different population groups (e.g. adolescents, adults, elderly, students, outpatients, and inpatients) were the target of previous studies [9, 10]. However, healthcare workers, who are a group at risk for sleep disorders (about 80%) and aggression (about 30%) [2, 25], have been largely ignored. Fourth, previous studies have mainly focused on violence against healthcare workers rather than the manifestations of aggression in them [11, 38].
However, the present study is novel and covers all four mentioned limitations. According to these considerations and limitations of the previous research, the present study aimed to explore the associations of both sleep problems (i.e. insomnia, sleep apnea, and poor sleep quality) and self-regulation with types of aggression (i.e. anger, hostility, verbal aggression, and physical aggression) among health workers. The study examined the association between sleep problems, self-regulation, and interpersonal aggression among health workers.
Materials and Methods
Study design and samples
The statistical population of the current cross-sectional study included all healthcare personnel working in four state-run hospitals in Kermanshah City, Iran, from March 2021 to March 2022. Using a multi-stage random sampling method, 450 healthcare staff were invited to participate in the study. The research team first randomly selected four government hospitals. Then, some departments of each hospital were randomly selected, and the staff list was provided. Finally, we randomly selected a few people from each department in proportion to the total number of people working there. The final sample consisted of physicians (n=62), nurses (n=233), guard staff (n=40), and service personnel (n=65). The sample size was calculated using two different methods. First, we calculated the power of the analyses and sufficiency of the sample for a small to medium anticipated effect size=0.20, power level=0.90, and α=0.05 for multiple regressions, including four predictor variables [39]. This analysis revealed a sample size of 82 for the present study. Second, we calculated the sample size for multiple regressions using a standard formula (N>50+8×number of predictor variables) [40, 41]. This analysis also revealed a sample size of 82 people for the present study. However, we used a sample size five times larger than the calculated amount to reduce all sampling errors, including α and β errors and the margin of error [41]. The sampling process was as follows. We invited 430 people to complete the questionnaires and 410 questionnaires were returned to the research team. The final sample consisted of 400 subjects after removing 10 subjects with large missing data. We included subjects fluent in Persian with an age range from 20 to 60 years, free from any pharmacotherapy or psychotherapy in the last 4 weeks, no substance abuse or drug addiction, and agreed to participate in the study. We also excluded physically disabled samples and subjects with many missing or invalid answers. The data collection process started after receiving the code of ethics from the Ethics Committee.
We first identified the samples and assured them about confidentiality. Then, the sample sociodemographic data, including gender and age groups, marital status, job condition, education level, and history of life-threatening illness, were collected using a self-report form. In the next step, 5 valid questionnaires to measure predictor and criterion variables were delivered to all participants by an experienced clinical psychologist. All questionnaires were distributed among the participants by a psychologist with a master’s degree (Shakiba Rezaei) trained by the supervisor (Azita Chehri). The predictor variables included poor sleep quality, sleep apnea, insomnia severity, and self-regulation, which were evaluated using the Pittsburgh sleep quality index (PSQI), the Berlin questionnaire (BQ), the insomnia severity index (ISI), and the self-regulation questionnaire (SRQ), respectively. The criterion variable was evaluated using the Buss-Perry aggression questionnaire (BPAQ).
Research tools
The Pittsburgh sleep quality index (PSQI) is a validated, self-report questionnaire comprising 18 items divided into 7 dimensions [23]: Subjective sleep quality (question 9), sleep latency (item 2 mean score and item 5a score), sleep duration (question 4), sleep efficiency (questions 1, 3, and 4), sleep disturbance (mean of items 5b and 5j), use of sleeping pills (question 6), and daytime dysfunction (mean of items 7 and 8). Each question has a score of 0-3, with a maximum score of 3 for each component. A set of these seven dimensions makes up the total score on the scale, which ranges from 0 to 21. The cutoff score for poor sleep quality is typically 5 or higher. Scores above this cutoff point indicate sleep disturbance in the individual. An initial validation study reported the scale’s Cronbach α equal to 0.83 and reported discriminant validity of the scale [23]. Also, the Persian version of PSQI is a good tool with acceptable discriminant validity and has a Cronbach α value of about 0.80 [42]. Another study reported the Cronbach α of the Persian version of PSQI equal to 0.94 [43].
The Berlin questionnaire (BQ) contains 10 questions in 3 categories to assess the risk for sleep apnea. Category I included 5 items related to snoring. Category II included 3 items related to daytime sleepiness, and category III included two items on the history of hypertension and or body mass index (BMI)>30 kg/m2. The differential validity of this questionnaire has been reported as acceptable [44]. The Persian version of BQ is a good screening tool with acceptable discriminant validity, and it had an agreement coefficient reliability above 0.80 [45].
The insomnia severity index (ISI) is a 7-item questionnaire used to measure the severity of insomnia. The index measures problems with sleep onset, sleep maintenance, early morning awakening, sleep dissatisfaction, sleep disturbances affecting daytime functioning, the impact of sleep disturbances on quality of life, and distress caused by sleep disturbances. Each item is given a score from 0 to 4 depending on its severity, and a total score is calculated by adding the scores of these 7 items [46]. A validation study confirmed both the reliability (α>0.80) and convergent validity of the Persian version of the scale with polysomnographic variables [47]. Another study in Iran [43] reported that the Cronbach α of the Persian version of ISI was acceptable (α=0.92).
The self-regulation questionnaire (SRQ) is a 31-item questionnaire that assesses the ability and severity of self-regulation. The questionnaire is rated on a Likert-type scale from 1 to 5 (strongly disagree or strongly agree). The person’s score ranges from 31 to 155, with higher scores indicating higher levels of self-regulation [48]. A previous study in Iran [34] reported that the reliability of this questionnaire is acceptable (α=0.93).
The Buss-Perry aggression questionnaire (BPAQ) is a 29-item scale used to measure aggression. The questions were scored on a 5-point rate, ranging from “extremely uncharacteristic of me” to “extremely characteristic of me”. The BPAQ contains four subscales: Anger, hostility, verbal aggression, and physical aggression. The scores are normalized on a scale of 0 to 1, with 1 being the highest level of aggression [5]. According to a previous report [49], the test-retest reliability of the Persian version of PSQI equals 0.78, and factor analysis methods confirmed the scale’s validity.
Data analysis
Data related to the continuous variables (age, aggression, poor sleep quality, sleep apnea, insomnia severity, and self-regulation) were reported as Mean±SD, and categorical data (gender groups, marital status, job condition, education level, history of life-threading illness) as frequency and percentage. We also compared the distribution of other variables, including marital status, education level, job condition, and life-threatening diseases.
Regarding the main objectives and analyses, we measured the relationship between predictors (poor sleep quality, sleep apnea, insomnia severity, and self-regulation) and criterion (all aggression subscales) variables using the Pearson correlation coefficients. In the next step, hierarchical linear regression analyses were used to identify the variables associated with aggression and its subscales. Before performing regression analyses, the non-violation of statistical assumptions (data normality, Durbin-Watson: Between 1.5 and 2.5, and the variance inflation factor: VIF <4) was checked and established [40, 41]. By entering all sleep problems in block 1 and self-regulation in block 2, we attempted to calculate both R2 and ΔR2. We compared ΔR2 to determine how much additional variance of self-regulation was predicted in the outcome (i.e. aggression subscales). The sleep problems and self-regulation in all models correlated to aggression subscales were identified using the ENTER method. We also reported β regression coefficients for all predictors in both blocks. Then, the differences in the β coefficients for sleep problems between blocks 1 and 2 (before and after entering the self-regulation variable) were reported using standardized z-scores. Because a larger sample size increases the power of statistical models and prevents biased results, we refrained from independently analyzing the subgroups (e.g. doctors or nurses) [40]. All statistical analyses were performed using SPSS software, version 25 (IBM Corp., Armonk, NY, USA) for two-tail tests and a P<0.05.
Results
Table 1 presents the sample’s distribution of demographic variables and disease history.
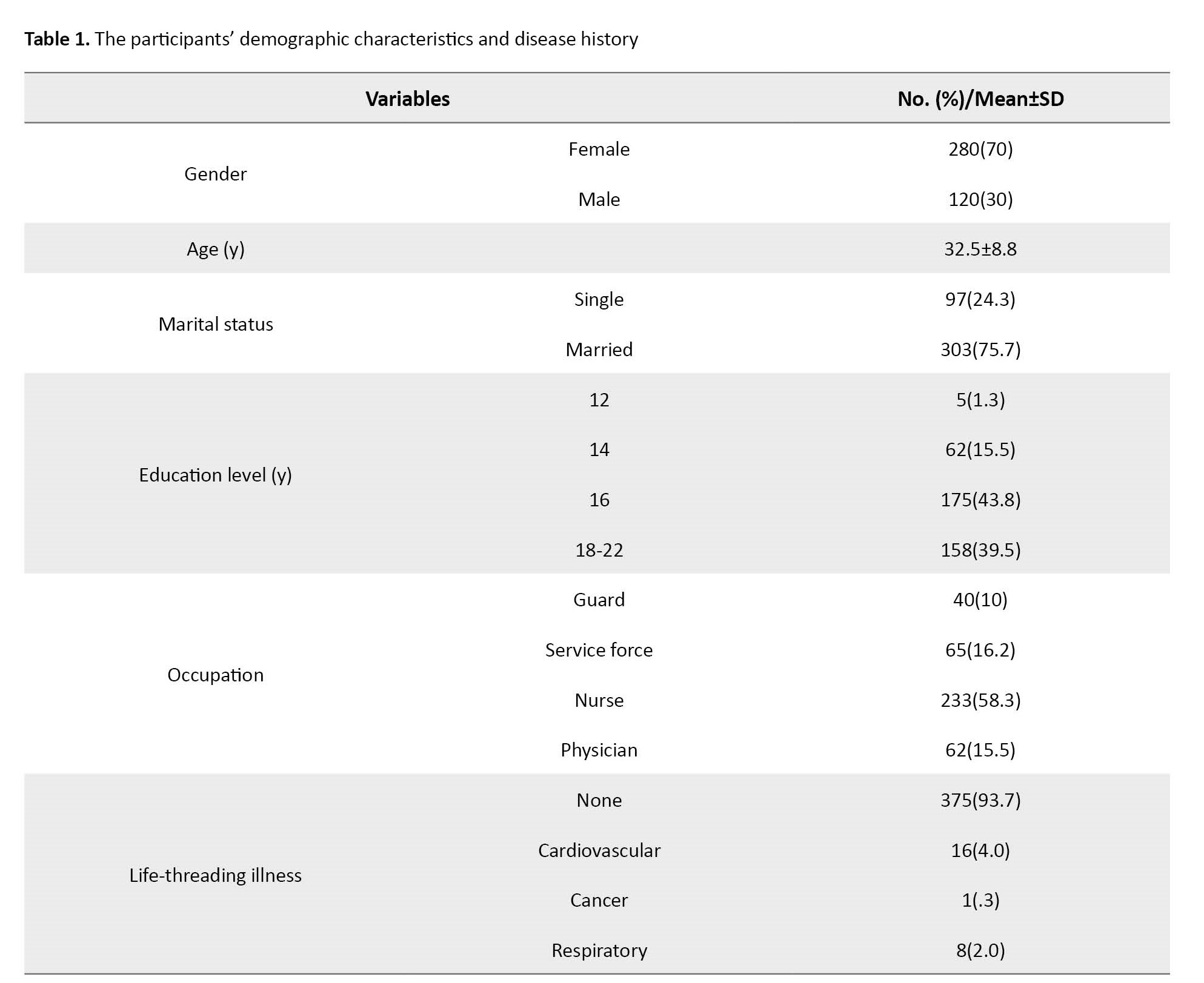
As seen, 70% of the samples were female, 76% were married, and 58% were nurses. The Mean±SD of age is 32.5±8.8 (between 20 and 55 years). This Table also shows that about 6% of the sample have a life-threading illness history.
Table 2 presents the descriptive data Mean±SD and Pearson correlations between the predictor (poor sleep quality, sleep apnea, insomnia severity, and self-regulation) and criterion (aggression) variables.
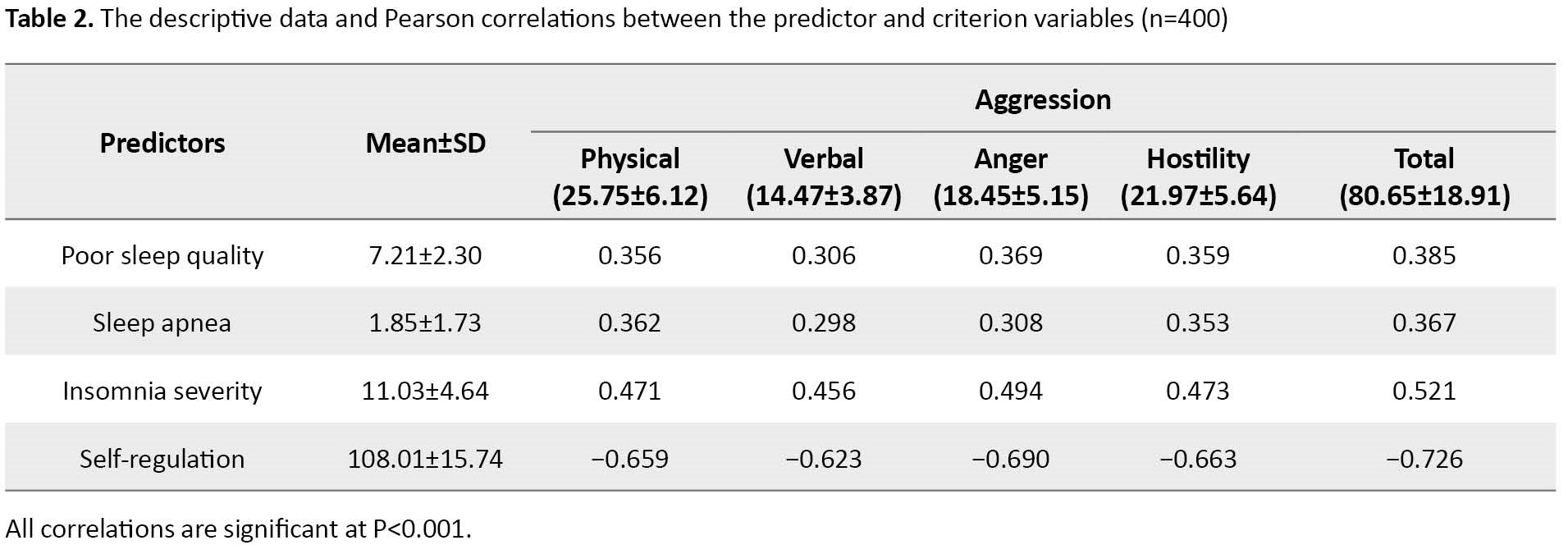
According to Table 2, the correlations between self-regulation and aggression variables are strongly significant (P<0.001). The negative correlations range from −0.623 (verbal aggression) to −0.726 (the total score of aggression). However, the correlations between all sleep and aggression variables are weakly to moderately significant (P<0.001). The correlations with the aggression subscales range from 0.306 to 0.385, 0.298 to 0.367, and 0.456 to 0.521 for poor sleep quality, sleep apnea, and insomnia severity, respectively.
Table 3 presents the hierarchical linear regressions predicting sleep problems and self-regulation as blocks to predict the aggression subscales and total score.
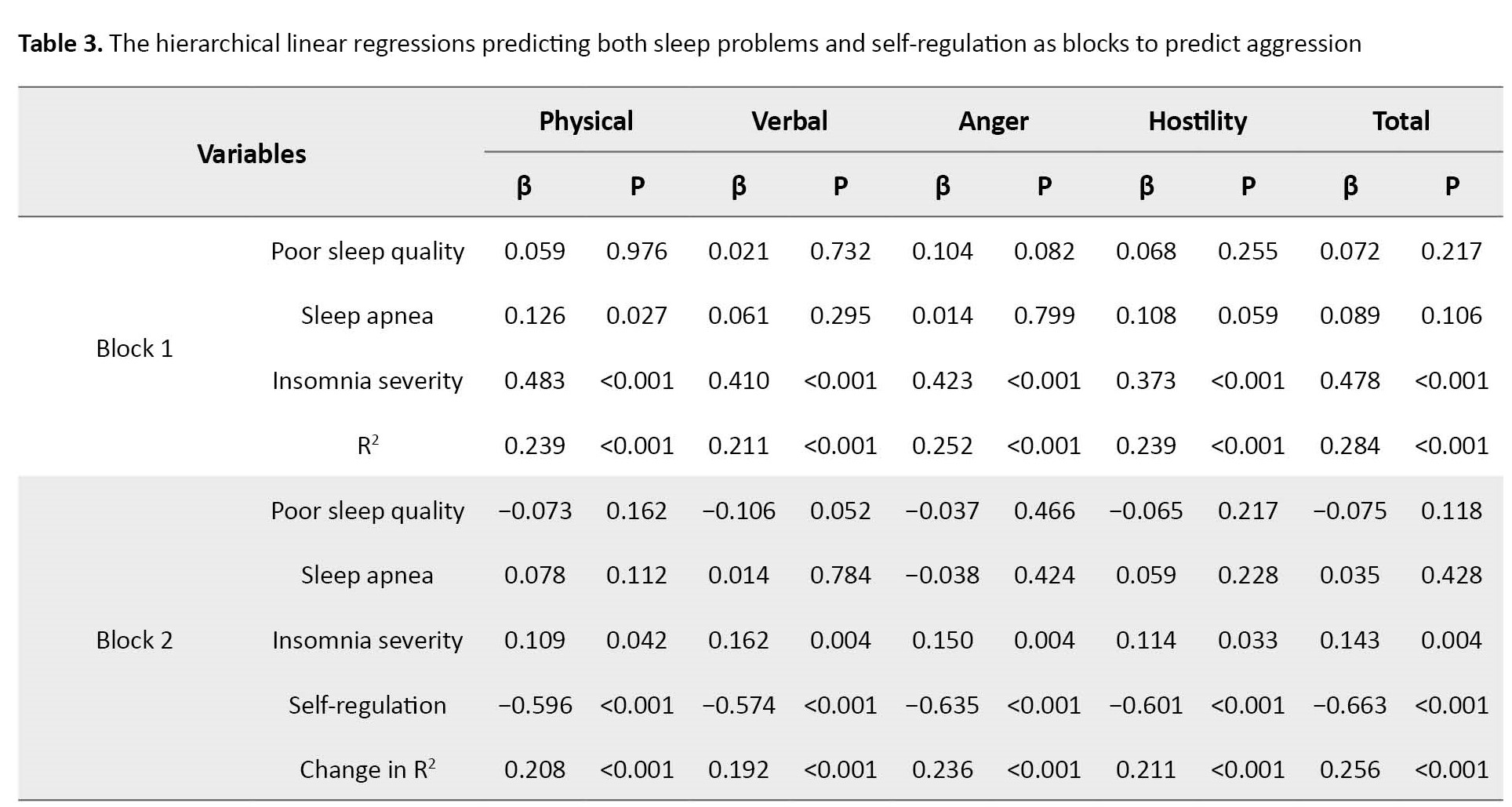
In block 1, three sleep problems, including poor sleep quality, sleep apnea, and insomnia severity, significantly predict all aggression subscales and total scores (all R2 ranging from 0.211 to 0.284, P<0.001). While poor sleep quality and sleep apnea are mostly mildly non-significantly related to aggression subscales, insomnia severity is strongly related to aggression and all subscales (β ranging from 0.373 to 0.483, P<0.001). In block 2, three sleep problems and self-regulation significantly predict all aggression subscales and total scores (ΔR2 ranging from 0.192 to 0.256, all P<0.001). In other words, self-regulation increases by 19.2% to 25.6%, the power of predicting aggression by sleep problems. Thus, self-regulation is strongly related to aggression, and all subscales (β ranging from −0.574 to −0.663, P<0.001).
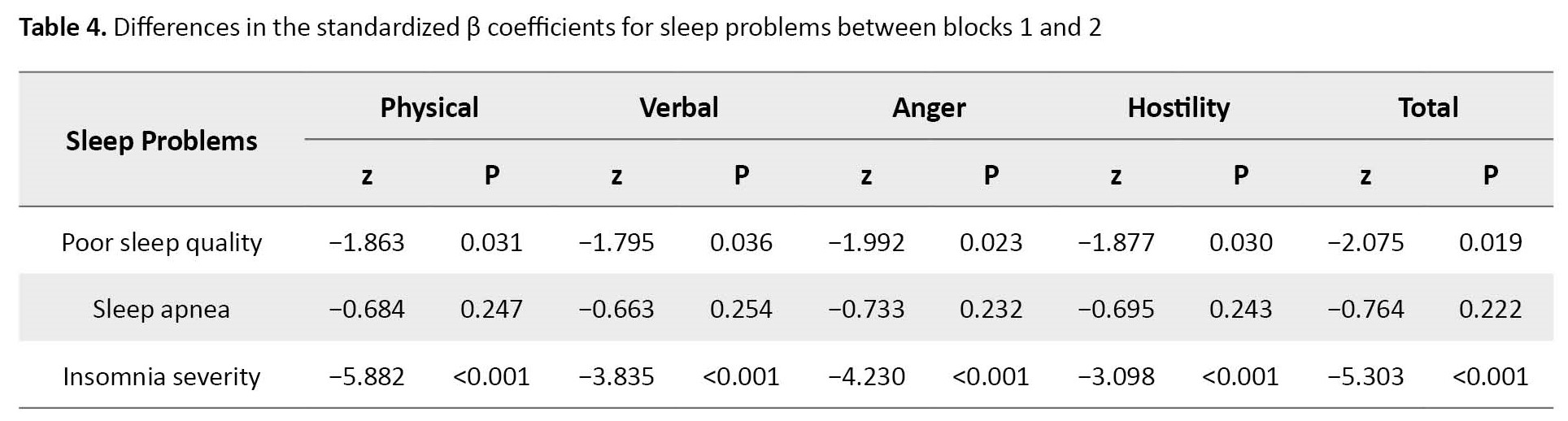
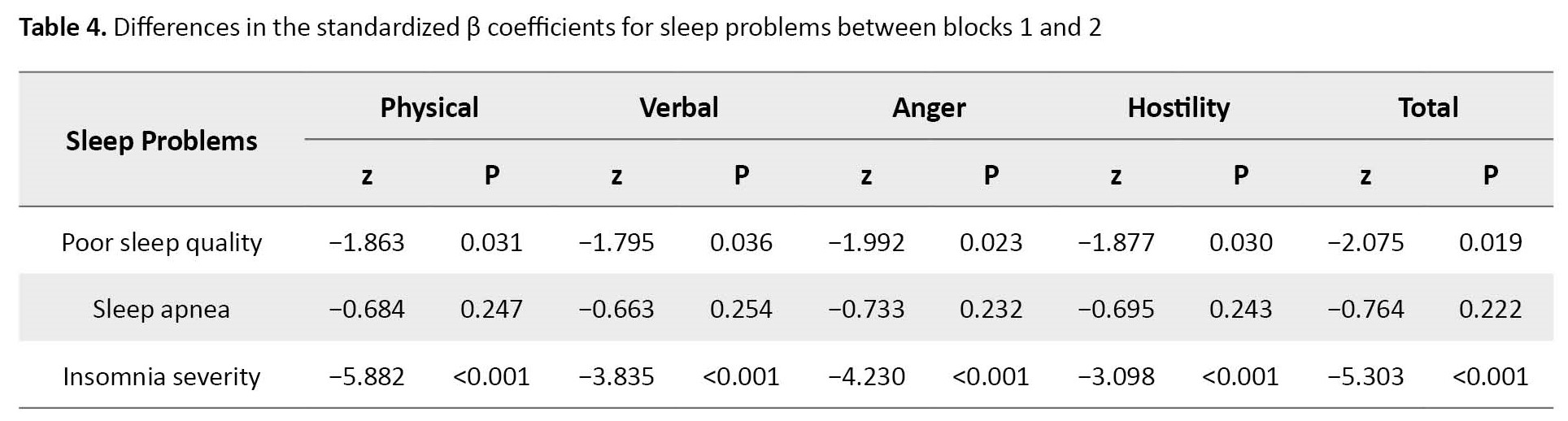
Table 3 for block 2 also shows that adding self-regulation to three sleep problems to predict aggression dramatically reduces the effect of sleep problems, especially the insomnia severity (from β=0.373 to 0.483 for all types of aggression to β=0.109 to 0.162). Table 4 presents that all standardized β coefficients for insomnia severity in blocks 1 and 2 are strongly different (z scores ranging from −3.098 to −5.882, P<0.001).
Discussion
The present study aimed to investigate the associations of sleep problems (poor sleep quality, sleep apnea, and insomnia) and self-regulation with aggression subscales, including anger, hostility, verbal aggression, and physical aggression among health workers. Previous studies show that aggressive behaviors and sleep disorders are common problems among health workers [2, 25]. Our results show that all sleep problems are significantly (but with weak to moderate effect sizes) related to the total score of aggression and all its subscales. Although one study did not find significant relationships between sleep problems and aggressive behaviors [50], several other studies reported the associations between some sleep problems (e.g. insomnia and sleep apnea) and aggression in both adult populations [18, 19, 20, 26] and other specific populations such as patients with epilepsy [27, 51]. Some studies also reported the relationship between sleep problems (e.g. insomnia and poor sleep quality) and aggressive behaviors among health workers [25, 37]. For example, one study found that poor sleep quality was significantly related to all aggression subscales [25]. However, studies among healthcare workers are few, and we found no contrary findings suggesting that sleep problems are not associated with aggression.
We found that insomnia severity, poor sleep quality, and sleep apnea are the most important sleep problems associated with all subfactors of aggression. This finding is consistent with previous studies investigating healthcare workers [25, 37]. Sleep problems can impair prefrontal cortex function, weakening top-down inhibition of aggressive behaviors [52]. The biological basis for the relationships between these phenomena is still unknown, and only speculative hypotheses have been put forward to explain them [27].
Our results also showed a significant negative relationship between self-regulation and all subscales of aggression. This finding is consistent with the results of previous studies among various population groups [28-30, 32, 33]. Conversely, one study did not report any significant relationship between some components of emotion regulation and aggression [53]. However, the results of some other studies supported the importance of self-regulation and similar mechanisms in health workers’ management of aggressive behavior [2, 35, 36, 54]. Self-regulation refers to internal and or transactional processes that enable individuals to direct their activities toward goals under changing circumstances over time [55]. People with high self-regulation continuously perform self-evaluation and self-monitoring, which can lead to self-organization and more adaptive behaviors. These are likely to be more self-efficacious and conscientious individuals who try to commit to a healthy lifestyle, including stress management, regular exercise, healthy eating, and regular sleep patterns. Therefore, poor self-regulation may be the direct and indirect facilitator of aggression.
Although aggression is a mental health problem with multifactorial risk factors (e.g. sociodemographic factors, physical illness and medication, and mental health conditions) that go beyond sleep problems and emotional dysregulation [10, 11, 15-17], we wanted to know what changes are made in the effect sizes of sleep problems when the self-regulation variable is added to the list of sleep variables in the regression models. Consistent with previous studies that showed the mediating role of emotional regulation in the relationship between sleep quality and aggression [29, 30], our results showed that adding self-regulation to the list of three sleep problems to predict aggression greatly reduces the effect size of both insomnia severity and in a milder way poor sleep quality. Although entering the variables with strong correlation into the regression model generally reduces the intensity of the associations of other predictor variables with the criterion variable [40], the finding means that the self-regulation (because of making very significant changes in the models) is directly a protective factor for aggression and indirectly reduces aggression by controlling the severity of insomnia. Although we could find no studies reporting a protective role of self-regulation on aggression by controlling sleep problems, a study by Demichelis et al. [29] showed that emotion regulation mediates the effects of sleep on aggression. However, self-regulation through promoting a healthy lifestyle [56] and increasing commitment to plans and goals dramatically reduces the risk of sleep problems and aggression.
We believe that the present study represents a pioneering work in reporting associations between three sleep problems and all subfactors of aggression. To our knowledge, previous studies do not report a protective role of self-regulation for aggression by controlling sleep apnea and insomnia severity [28-30]. However, the present research faces some limitations. First, using a cross-sectional design and self-report instruments prevents the reporting of causal relationships between the variables [57]. However, longitudinal evidence from future studies could provide valuable information for mental health researchers and clinicians. Second, some evidence supports the different symptoms and prevalence of aggression between men and women [58]. Although the comparison of gender groups was not the aim of the present study, future reports could use independent analyses for men and women. Third, most participants were between 20 and 40 years old, which can be a warning to generalize the findings to other age groups. Last, our sample was limited to health workers because they suffer more from sleep problems due to shift work. Thus, generalizing the present findings to other groups of society requires caution.
Conclusion
The present results showed that all sleep problems (positively) and self-regulation (negatively) are significantly related to the total score of aggression and all its subfactors, including anger, hostility, verbal aggression, and physical aggression. We found that the self-regulation variable is a protective factor for aggression and indirectly protects against aggression by controlling sleep problems, especially for insomnia severity. However, both sleep problems and self-dysregulation are modifiable risk factors for interpersonal aggression. Potentially, delivering interventions that promote self-regulation by controlling sleep problems may significantly prevent aggressive behaviors in adult health workers. However, the present study is limited to a cross-sectional design that includes only health workers and does not provide the results of gender and age subgroup analysis. Therefore, longitudinal evidence from future studies across the subgroups can give valuable information to mental health researchers, clinicians, and policymakers.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in the study involving human participants were conducted following the 1964 Helsinki Declaration. The study procedures were approved by the Ethics Committee of Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1402.130). Written informed consent was obtained from all individual participants included in the study.
Funding
This study was extracted from the PhD Dissertation of Shakiba Rezaei, approved by the Islamic Azad University, Kermanshah Barnch.
Authors contributions
Conceptualization: All authors; Methodology and analysis: Shakiba Rezaei and Hassan Amiri; Data collection: Shakiba Rezaei; Investigation: Saeede Sadat Hosseini and Mokhtar Arefi; Writing: All authors; Supervision: Azita Chehri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We thank the Islamic Azad University, Kermanshah Barnch and the Sleep Disorders Research Center of Kermanshah University of Medical Sciences for supporting this project.
References
Healthcare workers, due to their continuing workplace challenges and job burnout (about 30% to 60% affected) [1], are a community vulnerable to mental health problems and maladaptive behaviors such as aggression [2]. Although the research body in the past mainly focused on workplace violence against health workers [3], aggression towards clients and patients is also common in one-third of healthcare workers [2]. Aggression is an instinctive behavior that can be disproportionate or proportionate, depending on the situation [4]. Proportionate aggression is an adaptive behavior subject to social values, whereas disproportionate or extreme aggression is maladaptive, occurring in the face of actual or perceived risk [4]. Disproportionate aggression includes four categories: Anger, hostility, verbal aggression, and physical aggression [5]. Lifetime aggression is also prevalent in up to 80% of adult populations across cultures [6, 7, 8] and about 68% in Iranian adults [9, 10, 11].
Aggressive behaviors bear many consequences, including emotional problems, physical injuries, academic or work inability, psychosomatic complaints, chronic physical disability, and mortality [12, 13]. Etiological studies are continuously trying to identify risk factors for aggression to facilitate the delivery of therapeutic interventions [14]. However, a better understanding and identification of the biopsychosocial factors associated with aggression can help formulate strategies and prevent it [15]. A fresh study classified risk factors for aggression into three general categories: Cortical thickness, personality pathology, and trauma exposure [14]. Nevertheless, aggression is a complex phenomenon affected by multiple risk factors, such as sociodemographic factors [10, 11, 15], physical illness and medication [10, 16], mental health conditions [15, 17], and sleep problems [18, 19, 20].
Sleep problems, which are included in the list of potential risk factors for the manifestation of aggressive behaviors [18, 19, 20], have a wide range of sleep disorders. However, the three categories of insomnia, sleep apnea, and poor sleep quality are among the most important sleep problems. Insomnia is characterized by persistent difficulty with sleep initiation, maintenance, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep [21]. Sleep apnea, also known as obstructive sleep apnea, is a sleep disorder in which periods of stopped breathing or shallow breathing occur more frequently during sleep. Each break lasts from a few seconds to a few minutes and occurs several times a night [22]. Poor sleep quality is a more general sleep disorder that includes several problematic components in subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping pills, and daytime dysfunction [23]. A meta-analytic review estimated the overall prevalence of sleep disorders to be 50% in Iran [24]. Sleep disorders are also common problems among healthcare workers, and their prevalence reaches about 80% [25].
Although cross-sectional and longitudinal associations between sleep problems and aggression are reported by some review studies [19, 20, 26, 27], other studies have attempted to identify protective factors for aggression, such as reading, regular physical exercise, sexual satisfaction, financial management, social network, intimate relationship, empathy, coping, self-control, emotion regulation, and self-regulation [10, 28-33]. Self-regulation is a multidimensional construct that includes cognitive, motivational-emotional, and physiological processes affecting the active control of goal-directed actions [34]. Self-regulation plays an active role in some systems, including active control, initiation, moderation, continuity, and coordination [34]. Many studies have reported higher levels of aggression in individuals with poor self-regulatory mechanisms [29, 31, 32]. The results of some studies, but not in Iran, support the role of self-regulation and some similar mechanisms in managing the aggressive behavior of health workers [2, 35, 36].
In addition to direct associations of sleep disorders and self-regulation with aggressive behaviors in health workers [2, 25, 35, 36, 37], the results of several studies specifically show that emotional self-regulation also mediates the effects of sleep problems on aggression [28, 29, 30]. However, previous studies on the protective role of self-regulation for aggression caused by sleep problems are limited in several aspects. First, these studies only reported the associations between sleep quality, deprivation, and aggression. Therefore, other sleep problems, such as sleep apnea and insomnia symptoms, have been neglected. Second, some studies did not include all aggression subscales, including anger, hostility, verbal aggression, and physical aggression. Third, different population groups (e.g. adolescents, adults, elderly, students, outpatients, and inpatients) were the target of previous studies [9, 10]. However, healthcare workers, who are a group at risk for sleep disorders (about 80%) and aggression (about 30%) [2, 25], have been largely ignored. Fourth, previous studies have mainly focused on violence against healthcare workers rather than the manifestations of aggression in them [11, 38].
However, the present study is novel and covers all four mentioned limitations. According to these considerations and limitations of the previous research, the present study aimed to explore the associations of both sleep problems (i.e. insomnia, sleep apnea, and poor sleep quality) and self-regulation with types of aggression (i.e. anger, hostility, verbal aggression, and physical aggression) among health workers. The study examined the association between sleep problems, self-regulation, and interpersonal aggression among health workers.
Materials and Methods
Study design and samples
The statistical population of the current cross-sectional study included all healthcare personnel working in four state-run hospitals in Kermanshah City, Iran, from March 2021 to March 2022. Using a multi-stage random sampling method, 450 healthcare staff were invited to participate in the study. The research team first randomly selected four government hospitals. Then, some departments of each hospital were randomly selected, and the staff list was provided. Finally, we randomly selected a few people from each department in proportion to the total number of people working there. The final sample consisted of physicians (n=62), nurses (n=233), guard staff (n=40), and service personnel (n=65). The sample size was calculated using two different methods. First, we calculated the power of the analyses and sufficiency of the sample for a small to medium anticipated effect size=0.20, power level=0.90, and α=0.05 for multiple regressions, including four predictor variables [39]. This analysis revealed a sample size of 82 for the present study. Second, we calculated the sample size for multiple regressions using a standard formula (N>50+8×number of predictor variables) [40, 41]. This analysis also revealed a sample size of 82 people for the present study. However, we used a sample size five times larger than the calculated amount to reduce all sampling errors, including α and β errors and the margin of error [41]. The sampling process was as follows. We invited 430 people to complete the questionnaires and 410 questionnaires were returned to the research team. The final sample consisted of 400 subjects after removing 10 subjects with large missing data. We included subjects fluent in Persian with an age range from 20 to 60 years, free from any pharmacotherapy or psychotherapy in the last 4 weeks, no substance abuse or drug addiction, and agreed to participate in the study. We also excluded physically disabled samples and subjects with many missing or invalid answers. The data collection process started after receiving the code of ethics from the Ethics Committee.
We first identified the samples and assured them about confidentiality. Then, the sample sociodemographic data, including gender and age groups, marital status, job condition, education level, and history of life-threatening illness, were collected using a self-report form. In the next step, 5 valid questionnaires to measure predictor and criterion variables were delivered to all participants by an experienced clinical psychologist. All questionnaires were distributed among the participants by a psychologist with a master’s degree (Shakiba Rezaei) trained by the supervisor (Azita Chehri). The predictor variables included poor sleep quality, sleep apnea, insomnia severity, and self-regulation, which were evaluated using the Pittsburgh sleep quality index (PSQI), the Berlin questionnaire (BQ), the insomnia severity index (ISI), and the self-regulation questionnaire (SRQ), respectively. The criterion variable was evaluated using the Buss-Perry aggression questionnaire (BPAQ).
Research tools
The Pittsburgh sleep quality index (PSQI) is a validated, self-report questionnaire comprising 18 items divided into 7 dimensions [23]: Subjective sleep quality (question 9), sleep latency (item 2 mean score and item 5a score), sleep duration (question 4), sleep efficiency (questions 1, 3, and 4), sleep disturbance (mean of items 5b and 5j), use of sleeping pills (question 6), and daytime dysfunction (mean of items 7 and 8). Each question has a score of 0-3, with a maximum score of 3 for each component. A set of these seven dimensions makes up the total score on the scale, which ranges from 0 to 21. The cutoff score for poor sleep quality is typically 5 or higher. Scores above this cutoff point indicate sleep disturbance in the individual. An initial validation study reported the scale’s Cronbach α equal to 0.83 and reported discriminant validity of the scale [23]. Also, the Persian version of PSQI is a good tool with acceptable discriminant validity and has a Cronbach α value of about 0.80 [42]. Another study reported the Cronbach α of the Persian version of PSQI equal to 0.94 [43].
The Berlin questionnaire (BQ) contains 10 questions in 3 categories to assess the risk for sleep apnea. Category I included 5 items related to snoring. Category II included 3 items related to daytime sleepiness, and category III included two items on the history of hypertension and or body mass index (BMI)>30 kg/m2. The differential validity of this questionnaire has been reported as acceptable [44]. The Persian version of BQ is a good screening tool with acceptable discriminant validity, and it had an agreement coefficient reliability above 0.80 [45].
The insomnia severity index (ISI) is a 7-item questionnaire used to measure the severity of insomnia. The index measures problems with sleep onset, sleep maintenance, early morning awakening, sleep dissatisfaction, sleep disturbances affecting daytime functioning, the impact of sleep disturbances on quality of life, and distress caused by sleep disturbances. Each item is given a score from 0 to 4 depending on its severity, and a total score is calculated by adding the scores of these 7 items [46]. A validation study confirmed both the reliability (α>0.80) and convergent validity of the Persian version of the scale with polysomnographic variables [47]. Another study in Iran [43] reported that the Cronbach α of the Persian version of ISI was acceptable (α=0.92).
The self-regulation questionnaire (SRQ) is a 31-item questionnaire that assesses the ability and severity of self-regulation. The questionnaire is rated on a Likert-type scale from 1 to 5 (strongly disagree or strongly agree). The person’s score ranges from 31 to 155, with higher scores indicating higher levels of self-regulation [48]. A previous study in Iran [34] reported that the reliability of this questionnaire is acceptable (α=0.93).
The Buss-Perry aggression questionnaire (BPAQ) is a 29-item scale used to measure aggression. The questions were scored on a 5-point rate, ranging from “extremely uncharacteristic of me” to “extremely characteristic of me”. The BPAQ contains four subscales: Anger, hostility, verbal aggression, and physical aggression. The scores are normalized on a scale of 0 to 1, with 1 being the highest level of aggression [5]. According to a previous report [49], the test-retest reliability of the Persian version of PSQI equals 0.78, and factor analysis methods confirmed the scale’s validity.
Data analysis
Data related to the continuous variables (age, aggression, poor sleep quality, sleep apnea, insomnia severity, and self-regulation) were reported as Mean±SD, and categorical data (gender groups, marital status, job condition, education level, history of life-threading illness) as frequency and percentage. We also compared the distribution of other variables, including marital status, education level, job condition, and life-threatening diseases.
Regarding the main objectives and analyses, we measured the relationship between predictors (poor sleep quality, sleep apnea, insomnia severity, and self-regulation) and criterion (all aggression subscales) variables using the Pearson correlation coefficients. In the next step, hierarchical linear regression analyses were used to identify the variables associated with aggression and its subscales. Before performing regression analyses, the non-violation of statistical assumptions (data normality, Durbin-Watson: Between 1.5 and 2.5, and the variance inflation factor: VIF <4) was checked and established [40, 41]. By entering all sleep problems in block 1 and self-regulation in block 2, we attempted to calculate both R2 and ΔR2. We compared ΔR2 to determine how much additional variance of self-regulation was predicted in the outcome (i.e. aggression subscales). The sleep problems and self-regulation in all models correlated to aggression subscales were identified using the ENTER method. We also reported β regression coefficients for all predictors in both blocks. Then, the differences in the β coefficients for sleep problems between blocks 1 and 2 (before and after entering the self-regulation variable) were reported using standardized z-scores. Because a larger sample size increases the power of statistical models and prevents biased results, we refrained from independently analyzing the subgroups (e.g. doctors or nurses) [40]. All statistical analyses were performed using SPSS software, version 25 (IBM Corp., Armonk, NY, USA) for two-tail tests and a P<0.05.
Results
Table 1 presents the sample’s distribution of demographic variables and disease history.
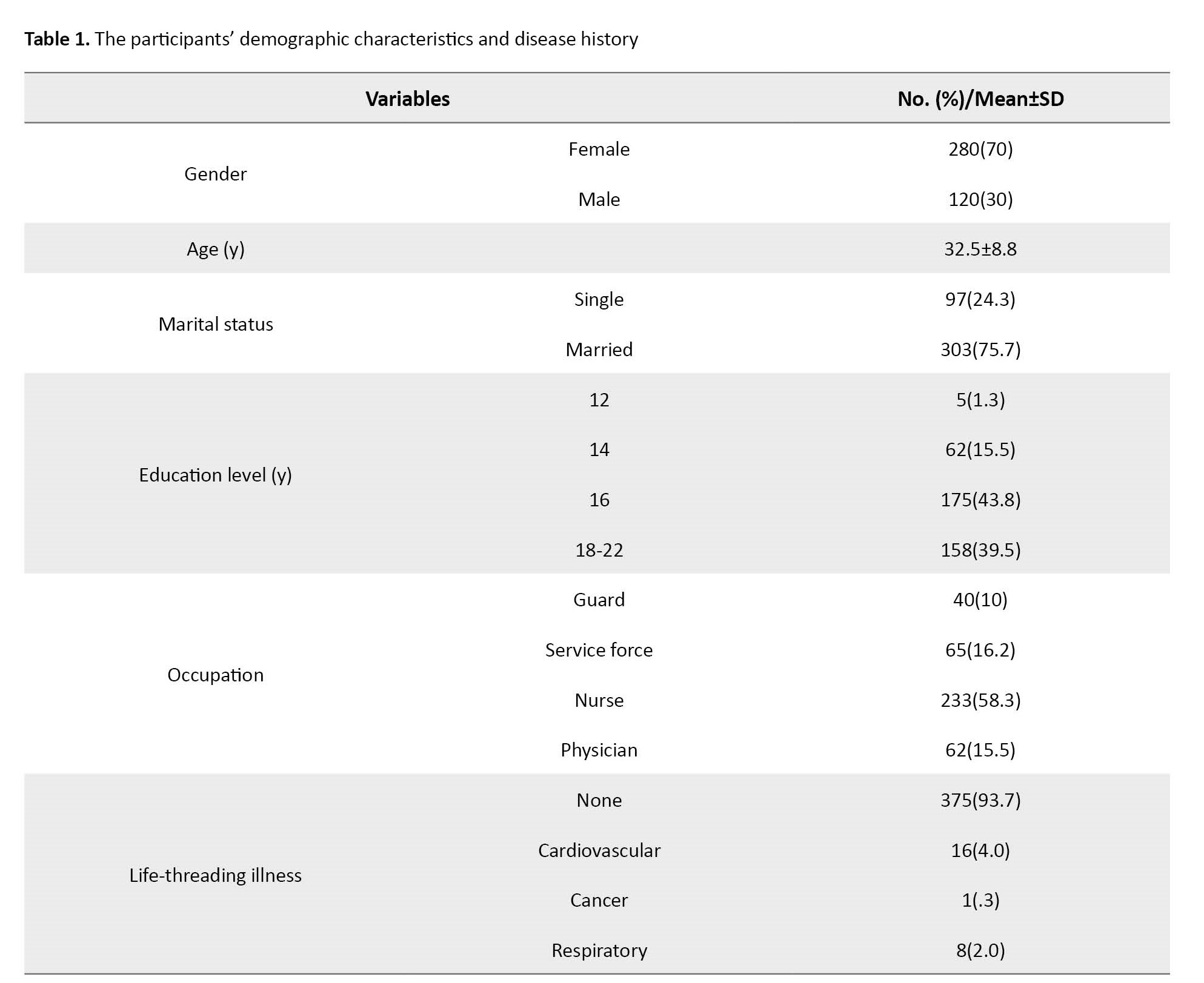
As seen, 70% of the samples were female, 76% were married, and 58% were nurses. The Mean±SD of age is 32.5±8.8 (between 20 and 55 years). This Table also shows that about 6% of the sample have a life-threading illness history.
Table 2 presents the descriptive data Mean±SD and Pearson correlations between the predictor (poor sleep quality, sleep apnea, insomnia severity, and self-regulation) and criterion (aggression) variables.
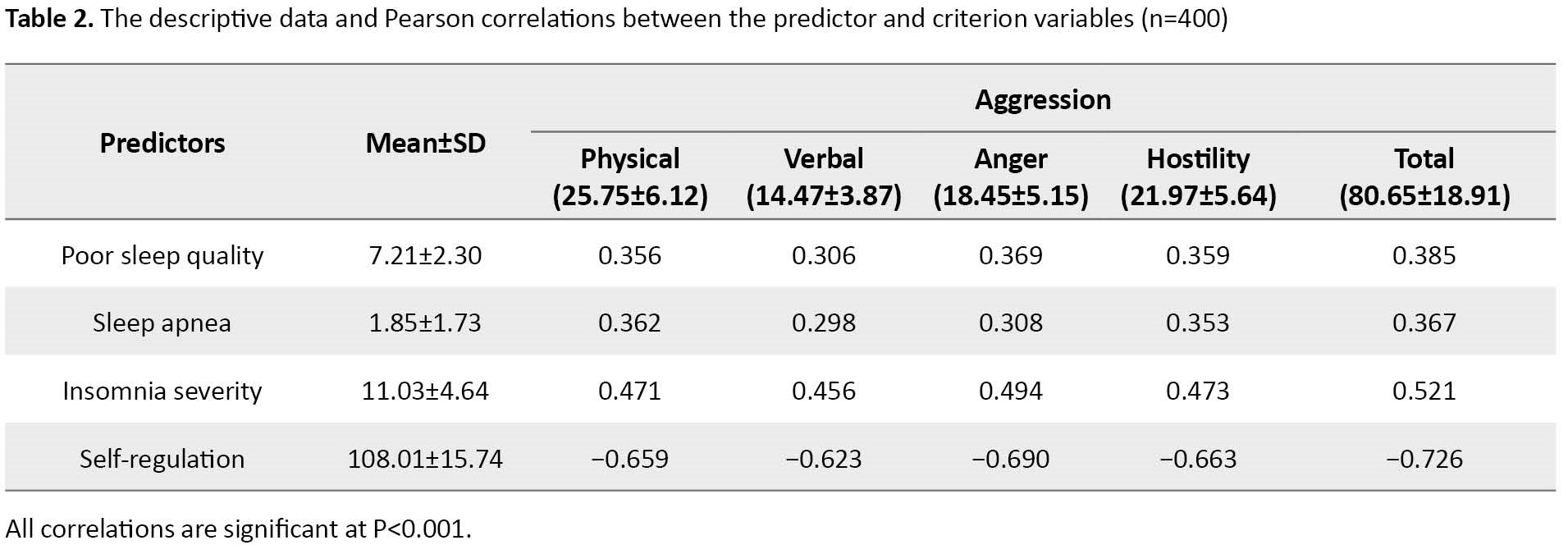
According to Table 2, the correlations between self-regulation and aggression variables are strongly significant (P<0.001). The negative correlations range from −0.623 (verbal aggression) to −0.726 (the total score of aggression). However, the correlations between all sleep and aggression variables are weakly to moderately significant (P<0.001). The correlations with the aggression subscales range from 0.306 to 0.385, 0.298 to 0.367, and 0.456 to 0.521 for poor sleep quality, sleep apnea, and insomnia severity, respectively.
Table 3 presents the hierarchical linear regressions predicting sleep problems and self-regulation as blocks to predict the aggression subscales and total score.
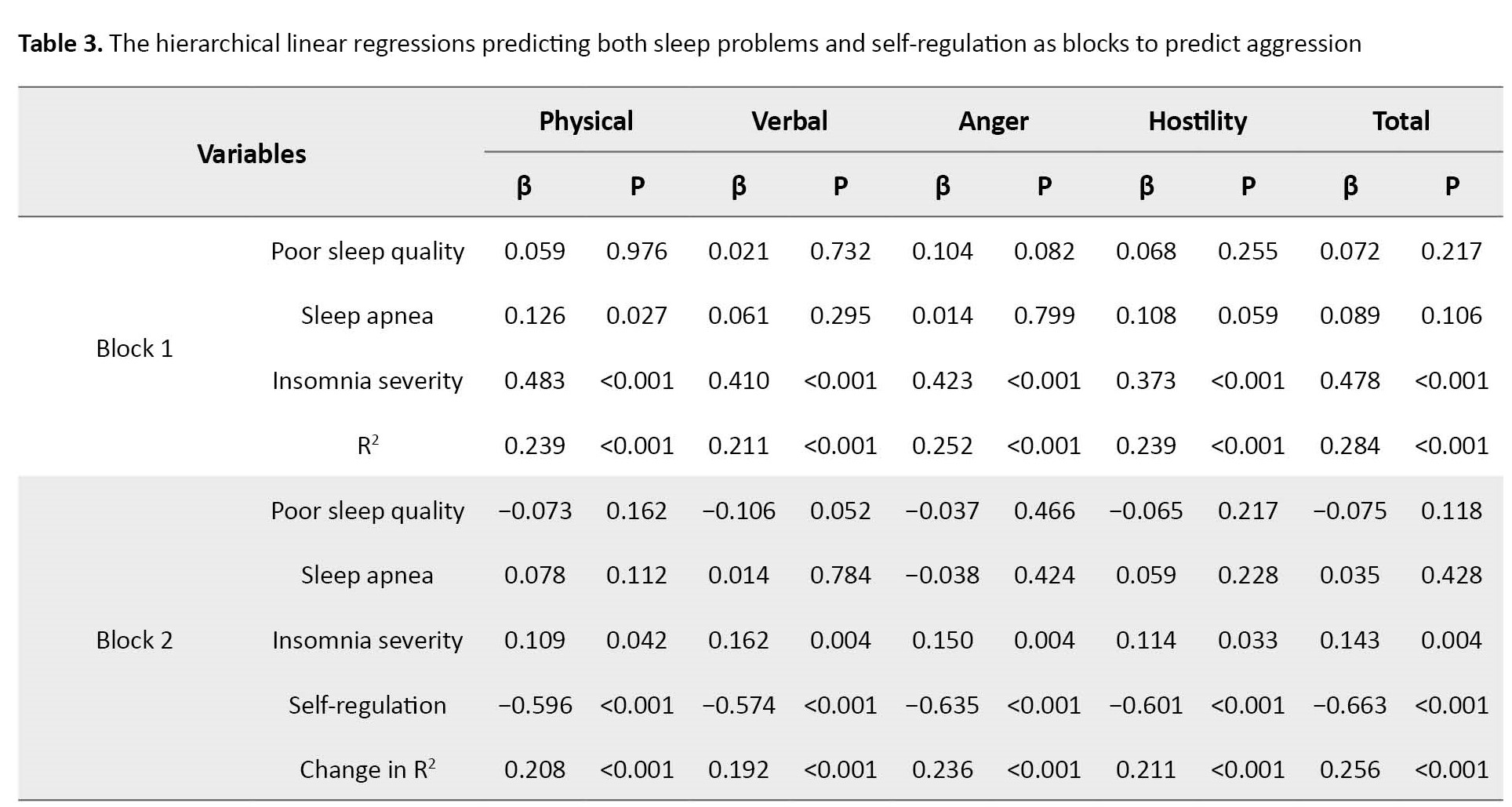
In block 1, three sleep problems, including poor sleep quality, sleep apnea, and insomnia severity, significantly predict all aggression subscales and total scores (all R2 ranging from 0.211 to 0.284, P<0.001). While poor sleep quality and sleep apnea are mostly mildly non-significantly related to aggression subscales, insomnia severity is strongly related to aggression and all subscales (β ranging from 0.373 to 0.483, P<0.001). In block 2, three sleep problems and self-regulation significantly predict all aggression subscales and total scores (ΔR2 ranging from 0.192 to 0.256, all P<0.001). In other words, self-regulation increases by 19.2% to 25.6%, the power of predicting aggression by sleep problems. Thus, self-regulation is strongly related to aggression, and all subscales (β ranging from −0.574 to −0.663, P<0.001).
Table 3 for block 2 also shows that adding self-regulation to three sleep problems to predict aggression dramatically reduces the effect of sleep problems, especially the insomnia severity (from β=0.373 to 0.483 for all types of aggression to β=0.109 to 0.162). Table 4 presents that all standardized β coefficients for insomnia severity in blocks 1 and 2 are strongly different (z scores ranging from −3.098 to −5.882, P<0.001).
Discussion
The present study aimed to investigate the associations of sleep problems (poor sleep quality, sleep apnea, and insomnia) and self-regulation with aggression subscales, including anger, hostility, verbal aggression, and physical aggression among health workers. Previous studies show that aggressive behaviors and sleep disorders are common problems among health workers [2, 25]. Our results show that all sleep problems are significantly (but with weak to moderate effect sizes) related to the total score of aggression and all its subscales. Although one study did not find significant relationships between sleep problems and aggressive behaviors [50], several other studies reported the associations between some sleep problems (e.g. insomnia and sleep apnea) and aggression in both adult populations [18, 19, 20, 26] and other specific populations such as patients with epilepsy [27, 51]. Some studies also reported the relationship between sleep problems (e.g. insomnia and poor sleep quality) and aggressive behaviors among health workers [25, 37]. For example, one study found that poor sleep quality was significantly related to all aggression subscales [25]. However, studies among healthcare workers are few, and we found no contrary findings suggesting that sleep problems are not associated with aggression.
We found that insomnia severity, poor sleep quality, and sleep apnea are the most important sleep problems associated with all subfactors of aggression. This finding is consistent with previous studies investigating healthcare workers [25, 37]. Sleep problems can impair prefrontal cortex function, weakening top-down inhibition of aggressive behaviors [52]. The biological basis for the relationships between these phenomena is still unknown, and only speculative hypotheses have been put forward to explain them [27].
Our results also showed a significant negative relationship between self-regulation and all subscales of aggression. This finding is consistent with the results of previous studies among various population groups [28-30, 32, 33]. Conversely, one study did not report any significant relationship between some components of emotion regulation and aggression [53]. However, the results of some other studies supported the importance of self-regulation and similar mechanisms in health workers’ management of aggressive behavior [2, 35, 36, 54]. Self-regulation refers to internal and or transactional processes that enable individuals to direct their activities toward goals under changing circumstances over time [55]. People with high self-regulation continuously perform self-evaluation and self-monitoring, which can lead to self-organization and more adaptive behaviors. These are likely to be more self-efficacious and conscientious individuals who try to commit to a healthy lifestyle, including stress management, regular exercise, healthy eating, and regular sleep patterns. Therefore, poor self-regulation may be the direct and indirect facilitator of aggression.
Although aggression is a mental health problem with multifactorial risk factors (e.g. sociodemographic factors, physical illness and medication, and mental health conditions) that go beyond sleep problems and emotional dysregulation [10, 11, 15-17], we wanted to know what changes are made in the effect sizes of sleep problems when the self-regulation variable is added to the list of sleep variables in the regression models. Consistent with previous studies that showed the mediating role of emotional regulation in the relationship between sleep quality and aggression [29, 30], our results showed that adding self-regulation to the list of three sleep problems to predict aggression greatly reduces the effect size of both insomnia severity and in a milder way poor sleep quality. Although entering the variables with strong correlation into the regression model generally reduces the intensity of the associations of other predictor variables with the criterion variable [40], the finding means that the self-regulation (because of making very significant changes in the models) is directly a protective factor for aggression and indirectly reduces aggression by controlling the severity of insomnia. Although we could find no studies reporting a protective role of self-regulation on aggression by controlling sleep problems, a study by Demichelis et al. [29] showed that emotion regulation mediates the effects of sleep on aggression. However, self-regulation through promoting a healthy lifestyle [56] and increasing commitment to plans and goals dramatically reduces the risk of sleep problems and aggression.
We believe that the present study represents a pioneering work in reporting associations between three sleep problems and all subfactors of aggression. To our knowledge, previous studies do not report a protective role of self-regulation for aggression by controlling sleep apnea and insomnia severity [28-30]. However, the present research faces some limitations. First, using a cross-sectional design and self-report instruments prevents the reporting of causal relationships between the variables [57]. However, longitudinal evidence from future studies could provide valuable information for mental health researchers and clinicians. Second, some evidence supports the different symptoms and prevalence of aggression between men and women [58]. Although the comparison of gender groups was not the aim of the present study, future reports could use independent analyses for men and women. Third, most participants were between 20 and 40 years old, which can be a warning to generalize the findings to other age groups. Last, our sample was limited to health workers because they suffer more from sleep problems due to shift work. Thus, generalizing the present findings to other groups of society requires caution.
Conclusion
The present results showed that all sleep problems (positively) and self-regulation (negatively) are significantly related to the total score of aggression and all its subfactors, including anger, hostility, verbal aggression, and physical aggression. We found that the self-regulation variable is a protective factor for aggression and indirectly protects against aggression by controlling sleep problems, especially for insomnia severity. However, both sleep problems and self-dysregulation are modifiable risk factors for interpersonal aggression. Potentially, delivering interventions that promote self-regulation by controlling sleep problems may significantly prevent aggressive behaviors in adult health workers. However, the present study is limited to a cross-sectional design that includes only health workers and does not provide the results of gender and age subgroup analysis. Therefore, longitudinal evidence from future studies across the subgroups can give valuable information to mental health researchers, clinicians, and policymakers.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in the study involving human participants were conducted following the 1964 Helsinki Declaration. The study procedures were approved by the Ethics Committee of Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1402.130). Written informed consent was obtained from all individual participants included in the study.
Funding
This study was extracted from the PhD Dissertation of Shakiba Rezaei, approved by the Islamic Azad University, Kermanshah Barnch.
Authors contributions
Conceptualization: All authors; Methodology and analysis: Shakiba Rezaei and Hassan Amiri; Data collection: Shakiba Rezaei; Investigation: Saeede Sadat Hosseini and Mokhtar Arefi; Writing: All authors; Supervision: Azita Chehri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We thank the Islamic Azad University, Kermanshah Barnch and the Sleep Disorders Research Center of Kermanshah University of Medical Sciences for supporting this project.
References
- De Hert S. Burnout in healthcare workers: Prevalence, impact and preventative strategies. Local and Regional Anesthesia. 2020; 13:171-83. [DOI:10.2147/LRA.S240564] [PMID]
- Pachi A, Kavourgia E, Bratis D, Fytsilis K, Papageorgiou SM, Lekka D, et al. Anger and aggression in relation to psychological resilience and alcohol abuse among health professionals during the first pandemic wave. Healthcare. 2023; 11(14):2031. [DOI:10.3390/healthcare11142031] [PMID]
- Mento C, Silvestri MC, Bruno A, Muscatello MR, Cedro C, Pandolfo G, et al. Workplace violence against healthcare professionals: A systematic review. Aggression and Violent Behavior. 2020; 51:101381. [DOI:10.1016/j.avb.2020.101381]
- Komasi S, Saeidi M, Soroush A, Zakiei A. The relationship between brain behavioral systems and the characteristics of the five factor model of personality with aggression among Iranian students. Journal of Injury and Violence Research. 2016; 8(2):67-74. [PMID]
- Buss AH, Perry M. The aggression questionnaire. Journal of Personality and Social Psychology. 1992; 63(3):452-9. [DOI:10.1037//0022-3514.63.3.452] [PMID]
- Krahé B, Tomaszewska P, Kuyper L, Vanwesenbeeck I. Prevalence of sexual aggression among young people in Europe: A review of the evidence from 27 EU countries. Aggression and Violent Behavior. 2014; 19(5):545-58. [DOI:10.1016/j.avb.2014.07.005]
- Liu J, Lewis G, Evans L. Understanding aggressive behaviour across the lifespan. Journal of Psychiatric Mental Health Nursing. 2013; 20(2):156-68. [DOI:10.1111/j.1365-2850.2012.01902.x] [PMID]
- Wang Y, Fu Y, Ghazi P, Gao Q, Tian T, Kong F, et al. Prevalence of intimate partner violence against infertile women in low-income and middle-income countries: A systematic review and meta-analysis. The Lancet. Global Health. 2022; 10(6):e820-30. [DOI:10.1016/S2214-109X(22)00098-5] [PMID]
- Kamali K, Maleki A, Yazdi SAB, Faghihzadeh E, Hoseinzade Z, Hajibabaei M, et al. The prevalence of violence and its association with mental health among the Iranian population in one year after the outbreak of COVID-19 disease. BMC Psychiatry. 2023; 23(1):33. [DOI:10.1186/s12888-022-04444-7] [PMID]
- Poorolajal J, Ebrahimi B, Rezapur-Shahkolai F, Doosti-Irani A, Alizadeh M, Ahmadpoor J, et al. The epidemiology of aggression and associated factors among Iranian adult population: A national survey. Journal of Research in Health Sciences. 2020; 20(4):e00499. [DOI:10.34172/jrhs.2020.34] [PMID]
- Sariaslani P, Soroush A, Faridmarandi B, Moarref M, Komasi S. Aggressive behavior and its triggers among hospitalized stroke patients’ entourages toward healthcare staff. Journal of Clinical Research in Paramedical Sciences. 2022; 11(2):e132226. [DOI:10.5812/jcrps-132226]
- Herrmann A, Seubert C, Glaser J. Consequences of exposure to violence, aggression, and sexual harassment in private security work: A mediation model. Journal of Interpersonal Violence. 2022; 37(11-12):NP9684-711. [DOI:10.1177/0886260520984432] [PMID]
- Sandoval GA, Marinho F, Delaney R, Pinto IV, Lima CMD, Costa RM, et al. Mortality risk among women exposed to violence in Brazil: a population-based exploratory analysis. Public Health. 2020; 179:45-50. [DOI:10.1016/j.puhe.2019.09.019] [PMID]
- Sheehan AE, Bounoua N, Miglin R, Spielberg JM, Sadeh N. A multilevel examination of lifetime aggression: integrating cortical thickness, personality pathology and trauma exposure. Social Cognitive and Affective Neuroscience. 2021; 16(7):716-25. [DOI:10.1093/scan/nsab042] [PMID]
- Saeidi M, Momeni K, Kakabraee K. Aggregation partitioning and study of demographic, medical, and psychological predictors related to derived clusters in cardiac rehabilitation patients: A cross-sectional study. Middle East Journal of Rehabilitation and Health Studies. 2019; 6(2):e86748. [DOI:10.5812/mejrh.86748]
- Wang Y, Li L, Cai J, Li H, Wang C. Incidental physical pain reduces brain activities associated with affective social feedback and increases aggression. Social Cognitive and Affective Neuroscience. 2023; 18(1):nsac048. [DOI:10.1093/scan/nsac048] [PMID]
- Whiting D, Gulati G, Geddes JR, Fazel S. Association of schizophrenia spectrum disorders and violence perpetration in adults and adolescents from 15 countries: A systematic review and meta-analysis. JAMA Psychiatry. 2022; 79(2):120-32. [DOI:10.1001/jamapsychiatry.2021.3721] [PMID]
- Carissimi A, Montanari CC, Kim LJ, Martins E, De Oliveira AA, Martinez D. Sleep apnea and aggressiveness. Sleep Medicine. 2013; 14(Supplement 1):e199. [DOI:10.1016/j.sleep.2013.11.473]
- Demichelis OP, Grainger SA, McKay KT, Bourdaniotis XE, Churchill EG, Henry JD. Sleep, stress and aggression: Meta-analyses investigating associations and causality. Neuroscience and Biobehavioral Reviews. 2022; 139:104732. [DOI:10.1016/j.neubiorev.2022.104732] [PMID]
- Van Veen MM, Lancel M, Beijer E, Remmelzwaal S, Rutters F. The association of sleep quality and aggression: A systematic review and meta-analysis of observational studies. Sleep Medicine Reviews. 2021; 59:101500. [DOI:10.1016/j.smrv.2021.101500] [PMID]
- Khazaie H, Komasi S, Mehra R, Khazaie S, Alipourian A, Nambi V, et al. Insomnia and incidence of heart failure in a sample of half a million people: A meta-analytic review and meta-regression of prospective studies. Current Sleep Medicine Reports. 2023; 9:281–95.[DOI:10.1007/s40675-023-00269-2]
- Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clinic Proceedings. 2011; 86(6):549-54; quiz 554-5. [DOI:10.4065/mcp.2010.0810] [PMID]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Jalali R, Mohammadi M, Vaisi-Raygani A, Salari N. The prevalence of sleep disorders among Iranian older adults: A systematic review and meta-analysis. Current Psychology. 2022; 41:8002–9.[DOI:10.1007/s12144-020-01252-8]
- Cybulska AM, Weymann A, Rachubińska K, Grochans S, Wójcik G, Grochans E. Factors associated with insomnia and aggression among healthcare workers during COVID-19 pandemic. International Journal of Environmental Research and Public Health. 2023; 20(2):1433. [DOI:10.3390/ijerph20021433] [PMID]
- Magnavita N, Di Stasio E, Capitanelli I, Lops EA, Chirico F, Garbarino S. Sleep problems and workplace violence: A systematic review and meta-analysis. Frontiers in Neuroscience. 2019; 13:997. [DOI:10.3389/fnins.2019.00997] [PMID]
- Sarzetto A, Bosia M, Pasqualoni E, Travaini G. Eyes wide open: A systematic review of the association between insomnia and aggression in forensic contexts. International Jornal of Law and Psychiatry. 2021; 78:101734. [DOI:10.1016/j.ijlp.2021.101734] [PMID]
- Christian MS, Ellis AP. Examining the effects of sleep deprivation on workplace deviance: A self-regulatory perspective. Academy of Management Journal. 2011; 54(5):913-34. [DOI:10.5465/amj.2010.0179]
- Demichelis OP, Grainger SA, Burr L, Henry JD. Emotion regulation mediates the effects of sleep on stress and aggression. Journal of Sleep Research. 2023; 32(3):e13787. [DOI:10.1111/jsr.13787] [PMID]
- Kirwan M, Svenson DW, Pickett SM, Parkhill MR. Emotion regulation as a mediator between sleep quality and interpersonal aggression. Personality and Individual Differences. 2019; 148:32-7. [DOI:10.1016/j.paid.2019.05.018]
- Klepfisz G, Daffern M, Day A. Understanding protective factors for violent reoffending in adults. Aggression and Violent Behavior. 2017; 32: 80-7. [DOI:10.1016/j.avb.2016.12.001]
- Plessen KJ, Constanty L, Ranjbar S, Turri F, Miano G, Lepage C, et al. The role of self-regulatory control processes in understanding aggressive ideations and behaviors: An experience sampling method study. Frontiers in Psychiatry. 2023; 13:1058814. [DOI:10.3389/fpsyt.2022.1058814] [PMID]
- Navas-Casado ML, García-Sancho E, Salguero JM. Associations between maladaptive and adaptive emotion regulation strategies and aggressive behavior: A systematic review. Aggression and Violent Behavior. 2023; 71:101845. [DOI:10.1016/j.avb.2023.101845]
- Zakiei A, Khazaie H, Alimoradi M, Kadivarian A, Rajabi-Gilan N, Komasi S. A causal model for the control of risk factors for cardiovascular diseases using a new temperamental personality theory in the general population of Western Iran: The mediating role of self-regulation. Journal of Practice of Cardiovascular Sciences. 2021; 7(3):190-7. [Link]
- Farahani M, Ebadie Zare S. Effectiveness of cognitive-behavioral anger management training on aggression and job satisfaction on nurses working in psychiatric hospital. Zahedan Journal of Research in Medical Sciences. 2018; 20(2):e55348. [DOI:10.5812/zjrms.55348]
- Goldblatt H, Freund A, Drach-Zahavy A, Enosh G, Peterfreund I, Edlis N. Providing health care in the shadow of violence: Does emotion regulation vary among hospital workers from different professions? Journal of Interpersonal Violence. 2020; 35(9-10):1908-33. [DOI:10.1177/0886260517700620] [PMID]
- Schneider-Matyka D, Cybulska AM, Rachubińska K, Grochans S, Weymann A. Factors associated with insomnia and aggression among healthcare workers during the COVID-19 pandemic. European Psychiatry. 2023; 66(S1):S211. [Link]
- Schablon A, Zeh A, Wendeler D, Peters C, Wohlert C, Harling M, et al. Frequency and consequences of violence and aggression towards employees in the German healthcare and welfare system: A cross-sectional study. BMJ Open. 2012; 2(5):e001420. [DOI:10.1136/bmjopen-2012-001420] [PMID]
- Free statistics calculators. A-priori sample size calculator for multiple regression [Internet]. 2023. [Updated 2024 February]. Available from: [Link]
- Pallant J.SPSS survival manual: A step by step guide to data analysis using IBM SPSS. New York: McGraw-Hill Education; 2020. [Link]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Boston: Pearson; 2013. [Link]
- Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep and Breathing. 2012; 16(1):79-82. [DOI:10.1007/s11325-010-0478-5] [PMID]
- Khazaie H, Najafi F, Zakiei A, Komasi S. Partitioning the sleep quality and insomnia severity among earthquake victims in the west of Iran: Cluster prediction based on personality and psychological factors. Journal of Research in Health Sciences. 2019; 19(4):e00458. [PMID]
- Tan A, Yin JD, Tan LW, van Dam RM, Cheung YY, Lee CH. Using the Berlin Questionnaire to predict obstructive sleep apnea in the general population. Journal of Clinical Sleep Medicine. 2017; 13(3):427-32. [DOI:10.5664/jcsm.6496] [PMID]
- Amra B, Nouranian E, Golshan M, Fietze I, Penzel T. Validation of the Persian version of Berlin Sleep Questionnaire for diagnosing obstructive sleep apnea. International Journal of Preventive Medicine. 2013; 4(3):334-9. [PMID]
- Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011; 34(5):601-8. [DOI:10.1093/sleep/34.5.601] [PMID]
- Yazdi Z, Sadeghniiat-Haghighi K, Zohal MA, Elmizadeh K. Validity and reliability of the Iranian version of the insomnia severity index. Malaysian Journal of Medical Sciences. 2012; 19(4):31-6. [PMID]
- Neal DJ, Carey KB. A follow-up psychometric analysis of the self-regulation questionnaire. Psychology of Addictive Behaviors. 2005; 19(4):414-22. [DOI:10.1037/0893-164X.19.4.414] [PMID]
- Amidi Mazaheri M, Karbasi M. General mental health and aggression in female prisoners in Isfahan. Health Education and Health Promotion. 2015; 3(4):15-26. [Link]
- Zschoche M, Schlarb AA. Is there an association between insomnia symptoms, aggressive behavior, and suicidality in adolescents? Adolescent Health, Medicine and Therapeutics. 2015; 6:29-36. [DOI:10.2147/AHMT.S76511] [PMID]
- Lee SA, Kim HJ, Kim HW, Koo YS. Insomnia symptoms and obesity are associated with aggression independent of depression in patients with epilepsy. Seizure. 2020; 74:65-70. [DOI:10.1016/j.seizure.2019.12.003] [PMID]
- Blair RJ. The neurobiology of impulsive aggression. Journal of Child and Adolescent Psychopharmacology. 2016; 26(1):4-9. [DOI:10.1089/cap.2015.0088] [PMID]
- Shadara Z, Dehghani M, Heidari M, Mahmoud Aliloo M. Distress tolerance, impulsivity, and aggression: The role of emotional dysregulation and reward sensitivity in individuals with borderline personality disorder features. Journal of Practice in Clinical Psychology. 2021; 9(1):37-50. [DOI:10.32598/jpcp.9.1.727.1]
- Tanabe Y, Asami T, Yoshimi A, Abe K, Saigusa Y, Hayakawa M, et al. Effectiveness of anger-focused emotional management training in reducing aggression among nurses. Nursing Open. 2023; 10(2):998-1006. [DOI:10.1002/nop2.1367] [PMID]
- Hennessy EA, Johnson BT, Acabchuk RL, McCloskey K, Stewart-James J. Self-regulation mechanisms in health behavior change: a systematic meta-review of meta-analyses, 2006-2017. Health Psychology Review. 2020; 14(1):6-42. [DOI:10.1080/17437199.2019.1679654] [PMID]
- Pfeffer I, Lach L, Sanchez X. Self-regulation and healthy lifestyles: Considering the future may increase current physical activity levels. Psychology, Health and Medicine. 2023; 28(10):2825-31. [DOI:10.1080/13548506.2022.2121973] [PMID]
- Wang X, Cheng Z. Cross-sectional studies: Strengths, weaknesses, and recommendations. Chest. 2020; 158(1):S65-71. [DOI:10.1016/j.chest.2020.03.012] [PMID]
- Björkqvist K. Gender differences in aggression. Current Opinion in Psychology. 2018; 19: 39-42. [DOI:10.1016/j.copsyc.2017.03.030] [PMID]
Type of Study: Original Article |
Subject:
Occupational Health
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









