Volume 12, Issue 2 (Spring 2024)
Iran J Health Sci 2024, 12(2): 141-148 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Safaie N, Moonesan M, Mirmohammadkhani M, Haidar E, Mansori K. Investigating the Epidemiology of Trauma in Children Under the Age of 15 Years in Semnan Province, Iran, From 2014 to 2018. Iran J Health Sci 2024; 12 (2) :141-148
URL: http://jhs.mazums.ac.ir/article-1-905-en.html
URL: http://jhs.mazums.ac.ir/article-1-905-en.html
Department of Emergency Medicine, School of Medicine, Semnan University of Medical Sciences, Semnan, Iran. , moonesan2023@gmail.com
Full-Text [PDF 668 kb]
(900 Downloads)
| Abstract (HTML) (2666 Views)
Full-Text: (804 Views)
Introduction
According to the definition of the World Health Organization (WHO), injury, and trauma are the acute contact of the body with mechanical energy, heat, electricity, chemical substances, and radioactive radiation more than the body can tolerate [1]. Trauma is one of the major health problems associated with death and a wide range of disabilities. All countries with different economic levels are dealing with this problem [2]. According to the report by the WHO, trauma is one of the common causes of death and disability in all age groups under 60 years. Also, this organization has predicted that injuries caused by accidents will be the second cause of years of life lost [3, 4].
Children are more exposed to trauma due to their physiological conditions and growth process, and the trauma inflicted on them can have deep and long-term effects [5]. In addition to the physical dimensions of psychological injuries, trauma in children will have deep and long-term effects on the performance of this group of patients [6, 7]. According to studies, the prevalence of childhood trauma in Western countries can vary from 15% to 25% [8]; however, more than 90% of all injury-related deaths still occur in children in low-income developing countries [9]. Trauma is the cause of more than 45% of deaths in children aged 1-14 years. Non-penetrating abdominal trauma is the third most common cause of death due to trauma in children, and at the same time, it is the most common undiagnosed fatal injury in this group [10, 11]. In Iran, the death rate due to trauma is estimated at 58 per 100 000 people. Trauma is the second cause of death in children under the age of 5 years in Iran. Studies have shown that falls, accidents, and violence are the main causes of trauma in children [12, 13].
The most important risk factors related to trauma in children include natural disasters, car accidents, physical, sexual, and emotional abuse, emotional and physical neglect, living with a family member with mental health or substance use disorders, witnessing domestic violence, sudden separation from a loved one, poverty, racism and discrimination, and violence in the community [14].
Trauma affects all races and cultures and all economic and social levels are exposed to its damage; however, there are noticeable differences in terms of prevalence and incidence, mechanism of creation, care methods, and outcomes among societies [15]. In the few studies that have been conducted in the field of the epidemiology of children’s trauma, even in similar populations, different results have been reported. For example, in the study done by Karbakhsh et al. in Tehran City, Iran, the most common causes of children’s trauma were falls (50.6%) and traffic accidents (40.6%) [16]. In Odetola’s study, domestic accidents (52%), falls (33%), and traffic accidents (12%) were determined as common causes of trauma among children in the United States [17].
However, traumatic injuries in children are a major and preventable cause of death and disability. The costs of preventing traumatic events are much lower than the costs of treatment, which are spent by families and the health system [18, 19]. In any country, estimating the rates of incidence, prevalence, and mortality of intentional and unintentional injuries in children and the correct evaluation of these injuries can help health policymakers design effective programs to control and prevent such incidents [20]. In Iran, given the increasing number of traffic accidents and the high rate of traffic accidents compared to many countries in the world, investigating the epidemiology and mechanism of trauma is essential, especially for children [21]. Accordingly, because of the importance of childhood and the necessity of considering the health of these groups as future makers of the country, the present study determines the pattern, causes, and consequences of trauma leading to hospitalization in children under the age of 15 years who were referred to the Emergency Department of Kowsar Hospital in Semnan, from 2014 to 2018.
Materials and Methods
Study design and subjects
This cross-sectional study was conducted to investigate the epidemiology of trauma in children under the age of 15 years who were referred to the emergency department of Kowsar Hospital, Semnan from 2014 to 2018. All children under 15 years of age who were referred to this hospital for trauma were studied. Firstly, only cases who were referred to the hospital were examined, and the information of other patients who died at the scene of the accident or were treated at home or in outpatient centers was not available. Secondly, due to the lack of accurate registration of international classification of disease codes, it was impossible to determine the exact type of injury in some patients. Thirdly, the study did not include any interventions or preventive strategies, limiting the results’ applicability. Meanwhile, the sample size was relatively small, which may have affected the accuracy of the results.
Study procedure
In this study, the data included age, gender, anatomical location of trauma, cause of trauma, the place of the occurrence of trauma, the type of intervention after trauma in the hospital, referral procedure to the hospital, and consequence and time of trauma which was extracted from the electronic records of patients in Kowsar Hospital of Semnan from 2014 to 2018. The inclusion criteria were having under 15 years of age and referral to the hospital due to trauma. Meanwhile, the exclusion criterion was incomplete data.
Statistical analysis
In the descriptive data analysis, Mean±SD frequency and percentage were used for quantitative variables. In addition, the chi-square test was used to investigate the association between gender and age with the cause of trauma and its outcome in children. The data were analyzed using the SPSS software, version 26. Meanwhile, the P<0.05 was considered a statistically significant level.
Results
A total of 2218 children were referred to the emergency department of Kowsar Semnan Hospital because of trauma from 2014 to 2018. Table 1 shows the demographic and clinical characteristics of traumatized children.
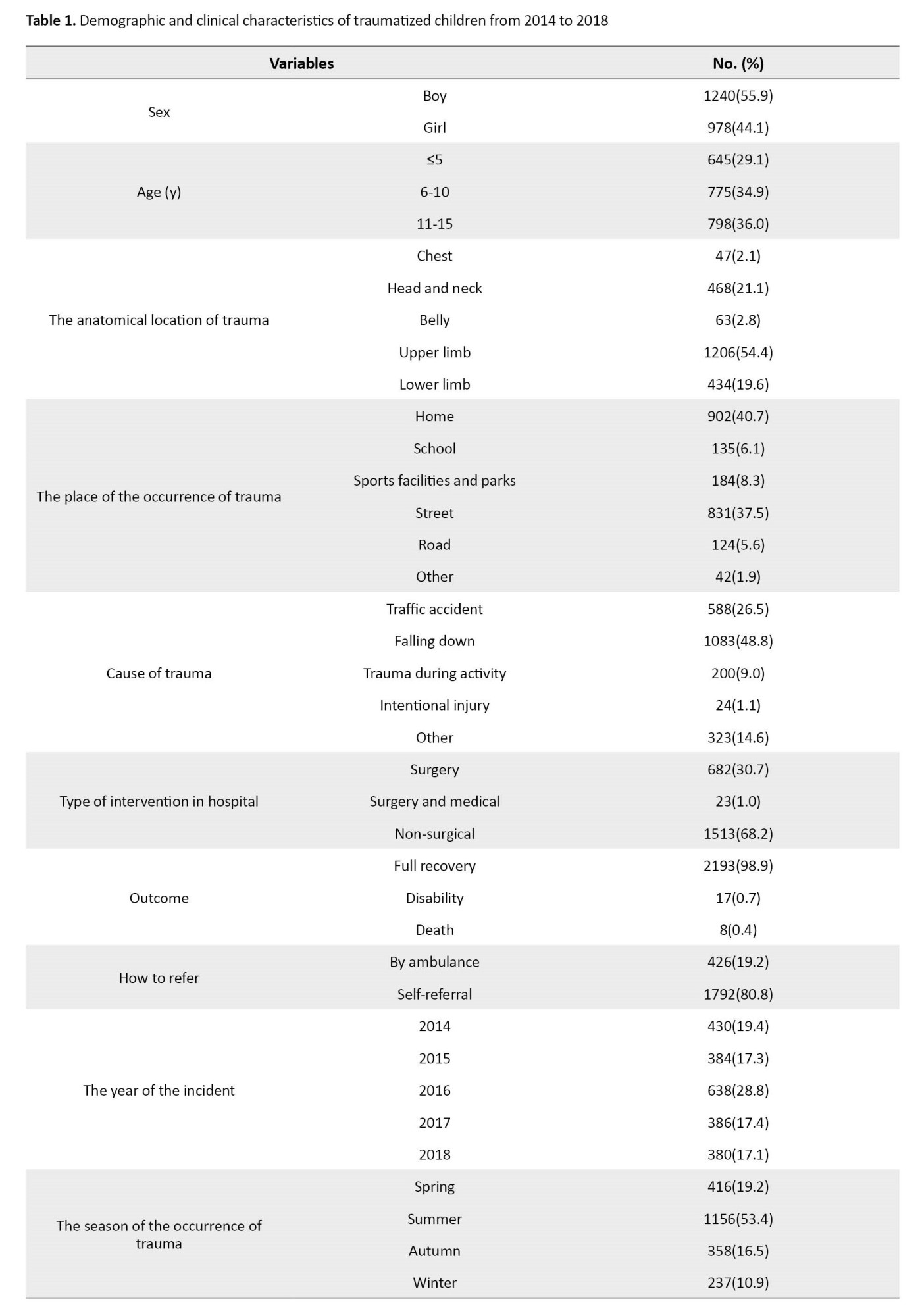
Accordingly, 1240 (55.9%) of the children were boys. Most of the traumatized children were in the age group of 10-15 years. The Mean±SD of the number of hospitalization days in the general ward and intensive care unit was 33.1±13.2 and 11.2±0.39 days, respectively. The most common site of injury was the upper limbs (n=1206 [54.4%]). The home was the most frequent place of occurrence of accidents leading to trauma (n=902 [40.7%]). Falling was the most common event leading to trauma (n=1083 [48.8%]). Also, 98.9% (n=2193) of the children were discharged from the emergency room with full recovery and about 0.4% (n=8) died. The highest number of trauma cases in these 5 years was in 2016 with 28.8% (n=638) and in terms of season, the most common time of trauma was related to summer with 53.4%. Other details can be seen in Table 1.
Table 2 shows the relationship between gender and age with the cause of trauma and its outcome in children under study.
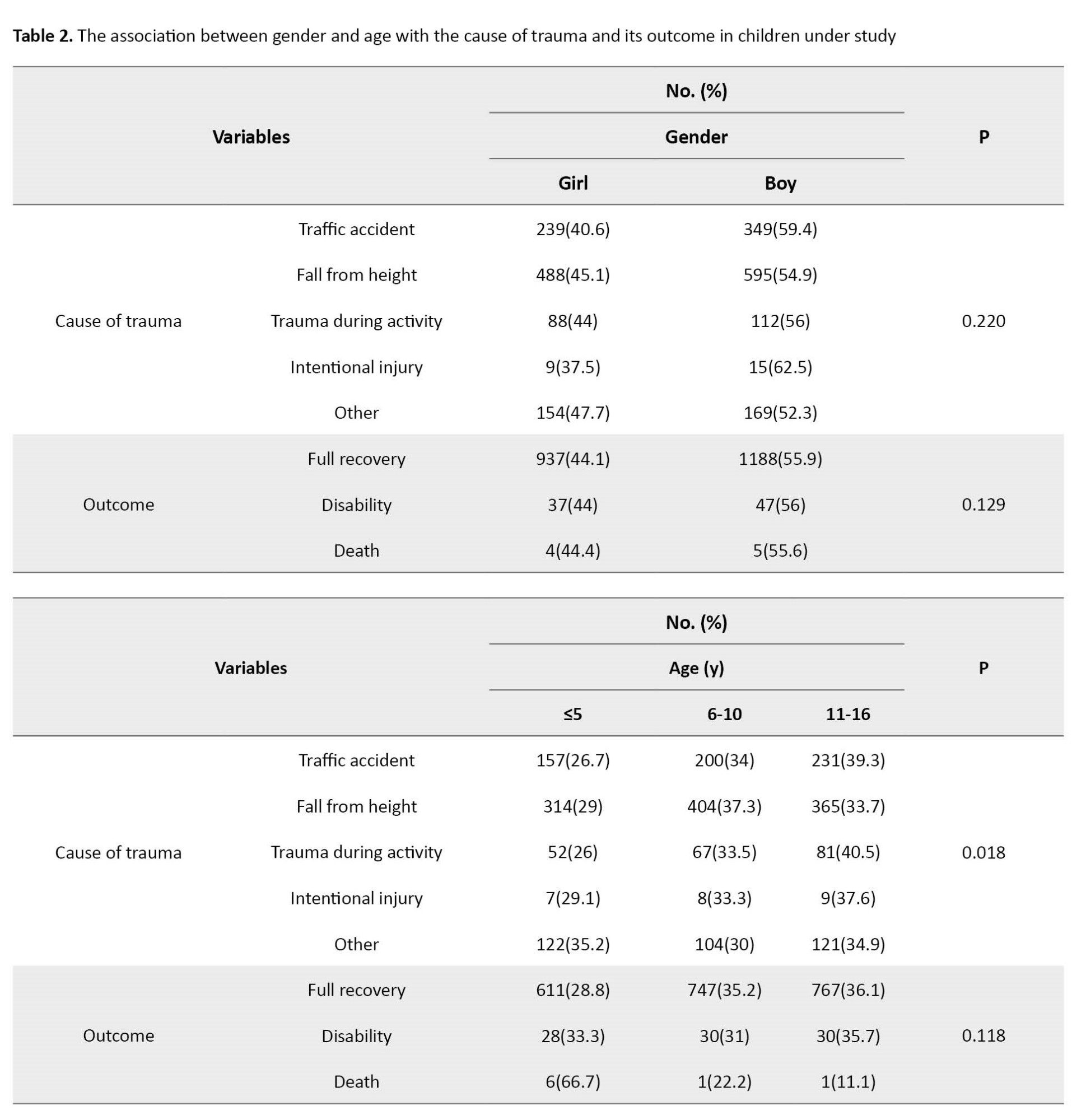
Accordingly, the chi-square test results showed no statistically significant relationship between gender with the cause of trauma and its outcome in traumatized children (P>0.05). Also, there was no statistically significant relationship between age with outcome in traumatized children (P>0.05). However, a statistically significant relationship was observed between the cause of trauma and age so the frequency of all traumatic events in children ≤5 was less than in other age groups (P<0.05).
Discussion
A total of 2218 injured children were examined, of which 55.9% were boys. More than a third of them were in the age group of 10-15 years (36%). The Mean±SD number of hospitalization days in the general ward and intensive care unit were 33.1±13.2 and 11.2±0.39 days, respectively. The most common site of injury was the upper limbs (54.4%). In addition, the home was the most frequent place of occurrence of accidents leading to trauma (40.7%). Most of the children’s traumas occurred in the summer season (53.4%). The most common event leading to trauma was falling (48.8%) and 0.4% died. Also, a statistically significant relationship was observed between the cause of trauma and age (P<0.05).
According to the results of this study, boys were traumatized more than girls. This is in line with studies conducted in different regions. For example, in a study conducted in the United States on more than 1.2 million children referred to the emergency department, 62% of traumatized children were boys [17]. The results of Karbakhsh et al.’s study in Tehran City, Iran, showed that 69.1% of traumatized children were boys [16]. In the study of Mirzaie et al. in Zahedan City, Iran, the incidence rate of hand trauma among boys was reported at 68% [22]. In Saaiq’s study on the cases of burns caused by electrocution of children in Pakistan, the highest frequency (89.41%) was related to boys [23]. Similar values in other studies conducted on this issue emphasize that different forms of trauma are more common in boys than girls [24, 25]. The occurrence of more trauma among boys can be attributed to two factors. On the one hand, boys are more likely to be allowed to be in high-risk situations; additionally, the frequency of high-risk behaviors is higher in boys. For example, the incidence rate of attention deficit hyperactive disorder in boys is about 2 times that of girls, which can lead to an increase in risky behaviors [26].
In the present study, the most common causes of trauma were falling (48.8%) and accidents, respectively. In line with the results of our study, in a study conducted in Tehran City, Iran, the most common cause of trauma in children was falls (50.6%) [16]. In another study conducted by Khorshidi in Hamedan City, Iran, falling was the most common cause of trauma (53%) [27]. In another study in the United Arab Emirates, the main mechanism of injuries leading to hospitalization of children falling was determined [22]. In Odetola’s study in America, domestic accidents, such as falls are the most common cause of children’s trauma, but traffic accidents were reported as the most important cause of trauma that led to children’s hospitalization [17]. Although there are differences in the introduction of the most common cause of trauma in children in different studies; however, in most of the studies, similar to the present study, traffic accidents and falls from heights were responsible for more than 70% of children’s trauma.
In the present study, the upper limbs were determined as the most common anatomical sites of trauma, which is consistent with the studies conducted in this field [17, 27]. However, in some other studies, the most common affected areas in children were head and neck [26, 28]. The reason for this inconsistency is unclear. Because due to the larger head-body ratio in children and the greater resistance of the bone structures of the organs, the probability of head and neck injury is higher [29]. In addition, some of this contradiction may be related to the non-referral of patients with mild trauma to the hospital or the outpatient treatment of these patients outside the hospital [27].
In the present study, most of the children’s trauma cases were related to the summer season (53.4%), which was consistent with similar studies in this field. Asadi et al.’s study in Gilan Province, Iran, as well as Arhami Dolatabadi et al.’s study in Tehran City, Iran, showed that most of the children’s traumas occurred in the summer season [20, 30]. Considering the closure of schools in the summer and the presence of more children at home as well as more trips in this season, the higher amount of trauma is not off the subject.
In the present study, the most common place of trauma was determined as home (44%) followed by the street (35%), which was in line with the results of similar studies [27, 31]. This finding is credible considering the presence of more children in the home compared to other places. In our study, the frequency of all traumatic events in children under 5 years was lower than in other children which was consistent with the results of other studies in this field [20, 27]. The reason for the lower number of traumatic events at this age may be due to the higher level of care received from parents compared to other age groups.
The mortality rate due to trauma among the children in our study was estimated at 0.4%, which was lower compared to other studies conducted in Iran (2.26%) and the United States (1.6%) [16, 32]. The mortality rate of children following trauma is higher than the amount observed in the present study. It is possible that the high intensity of most of the events (especially traffic accidents) as well as the high vulnerability of children led to death in the early moments of the accident before being referred to the hospital. For example, the results of a study indicated that 5.1% of the children who had an accident had died before the rescue forces arrived [22].
Conclusion
According to the results, the most common places of trauma were related to the house and the street due to falls and accidents. Therefore, in addition to informing families of the danger lurking in children, securing homes, and teaching children traffic rules and regulations should be given serious attention.
Study limitations and recommendations
This study faced the following limitations. Firstly, only the cases who were referred to the hospital have been examined, and the information of other patients who died at the scene of the accident or were treated at home or in outpatient centers was not available. Secondly, due to the lack of accurate registration of international classification of disease codes, it was impossible to determine the exact type of injury in some patients the design of the trauma registration system will help to conduct more accurate studies in the future and will increase the effectiveness of preventive strategies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Deputy of the Research and Ethics Committee of Semnan University of Medical Sciences (Code: IR.SEMUMS.REC.1396.213).
Funding
The present article was extracted from the general physician thesis of Elnaz Haidar, approved by School of Medicine, Semnan University of Medical Sciences.
Authors contributions
Conceptualization, supervision, funding acquisition and resources: Mohammadreza Moonesan and Nilufar Safaie; Methodology: Majid Mirmohammadkhani; Data collection: Elnaz Haidar; Data analysis: Kamyar Mansori Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their sincere gratitude to the staff of Kowsar Hospital for their cooperation during the carry-out of this research.
According to the definition of the World Health Organization (WHO), injury, and trauma are the acute contact of the body with mechanical energy, heat, electricity, chemical substances, and radioactive radiation more than the body can tolerate [1]. Trauma is one of the major health problems associated with death and a wide range of disabilities. All countries with different economic levels are dealing with this problem [2]. According to the report by the WHO, trauma is one of the common causes of death and disability in all age groups under 60 years. Also, this organization has predicted that injuries caused by accidents will be the second cause of years of life lost [3, 4].
Children are more exposed to trauma due to their physiological conditions and growth process, and the trauma inflicted on them can have deep and long-term effects [5]. In addition to the physical dimensions of psychological injuries, trauma in children will have deep and long-term effects on the performance of this group of patients [6, 7]. According to studies, the prevalence of childhood trauma in Western countries can vary from 15% to 25% [8]; however, more than 90% of all injury-related deaths still occur in children in low-income developing countries [9]. Trauma is the cause of more than 45% of deaths in children aged 1-14 years. Non-penetrating abdominal trauma is the third most common cause of death due to trauma in children, and at the same time, it is the most common undiagnosed fatal injury in this group [10, 11]. In Iran, the death rate due to trauma is estimated at 58 per 100 000 people. Trauma is the second cause of death in children under the age of 5 years in Iran. Studies have shown that falls, accidents, and violence are the main causes of trauma in children [12, 13].
The most important risk factors related to trauma in children include natural disasters, car accidents, physical, sexual, and emotional abuse, emotional and physical neglect, living with a family member with mental health or substance use disorders, witnessing domestic violence, sudden separation from a loved one, poverty, racism and discrimination, and violence in the community [14].
Trauma affects all races and cultures and all economic and social levels are exposed to its damage; however, there are noticeable differences in terms of prevalence and incidence, mechanism of creation, care methods, and outcomes among societies [15]. In the few studies that have been conducted in the field of the epidemiology of children’s trauma, even in similar populations, different results have been reported. For example, in the study done by Karbakhsh et al. in Tehran City, Iran, the most common causes of children’s trauma were falls (50.6%) and traffic accidents (40.6%) [16]. In Odetola’s study, domestic accidents (52%), falls (33%), and traffic accidents (12%) were determined as common causes of trauma among children in the United States [17].
However, traumatic injuries in children are a major and preventable cause of death and disability. The costs of preventing traumatic events are much lower than the costs of treatment, which are spent by families and the health system [18, 19]. In any country, estimating the rates of incidence, prevalence, and mortality of intentional and unintentional injuries in children and the correct evaluation of these injuries can help health policymakers design effective programs to control and prevent such incidents [20]. In Iran, given the increasing number of traffic accidents and the high rate of traffic accidents compared to many countries in the world, investigating the epidemiology and mechanism of trauma is essential, especially for children [21]. Accordingly, because of the importance of childhood and the necessity of considering the health of these groups as future makers of the country, the present study determines the pattern, causes, and consequences of trauma leading to hospitalization in children under the age of 15 years who were referred to the Emergency Department of Kowsar Hospital in Semnan, from 2014 to 2018.
Materials and Methods
Study design and subjects
This cross-sectional study was conducted to investigate the epidemiology of trauma in children under the age of 15 years who were referred to the emergency department of Kowsar Hospital, Semnan from 2014 to 2018. All children under 15 years of age who were referred to this hospital for trauma were studied. Firstly, only cases who were referred to the hospital were examined, and the information of other patients who died at the scene of the accident or were treated at home or in outpatient centers was not available. Secondly, due to the lack of accurate registration of international classification of disease codes, it was impossible to determine the exact type of injury in some patients. Thirdly, the study did not include any interventions or preventive strategies, limiting the results’ applicability. Meanwhile, the sample size was relatively small, which may have affected the accuracy of the results.
Study procedure
In this study, the data included age, gender, anatomical location of trauma, cause of trauma, the place of the occurrence of trauma, the type of intervention after trauma in the hospital, referral procedure to the hospital, and consequence and time of trauma which was extracted from the electronic records of patients in Kowsar Hospital of Semnan from 2014 to 2018. The inclusion criteria were having under 15 years of age and referral to the hospital due to trauma. Meanwhile, the exclusion criterion was incomplete data.
Statistical analysis
In the descriptive data analysis, Mean±SD frequency and percentage were used for quantitative variables. In addition, the chi-square test was used to investigate the association between gender and age with the cause of trauma and its outcome in children. The data were analyzed using the SPSS software, version 26. Meanwhile, the P<0.05 was considered a statistically significant level.
Results
A total of 2218 children were referred to the emergency department of Kowsar Semnan Hospital because of trauma from 2014 to 2018. Table 1 shows the demographic and clinical characteristics of traumatized children.
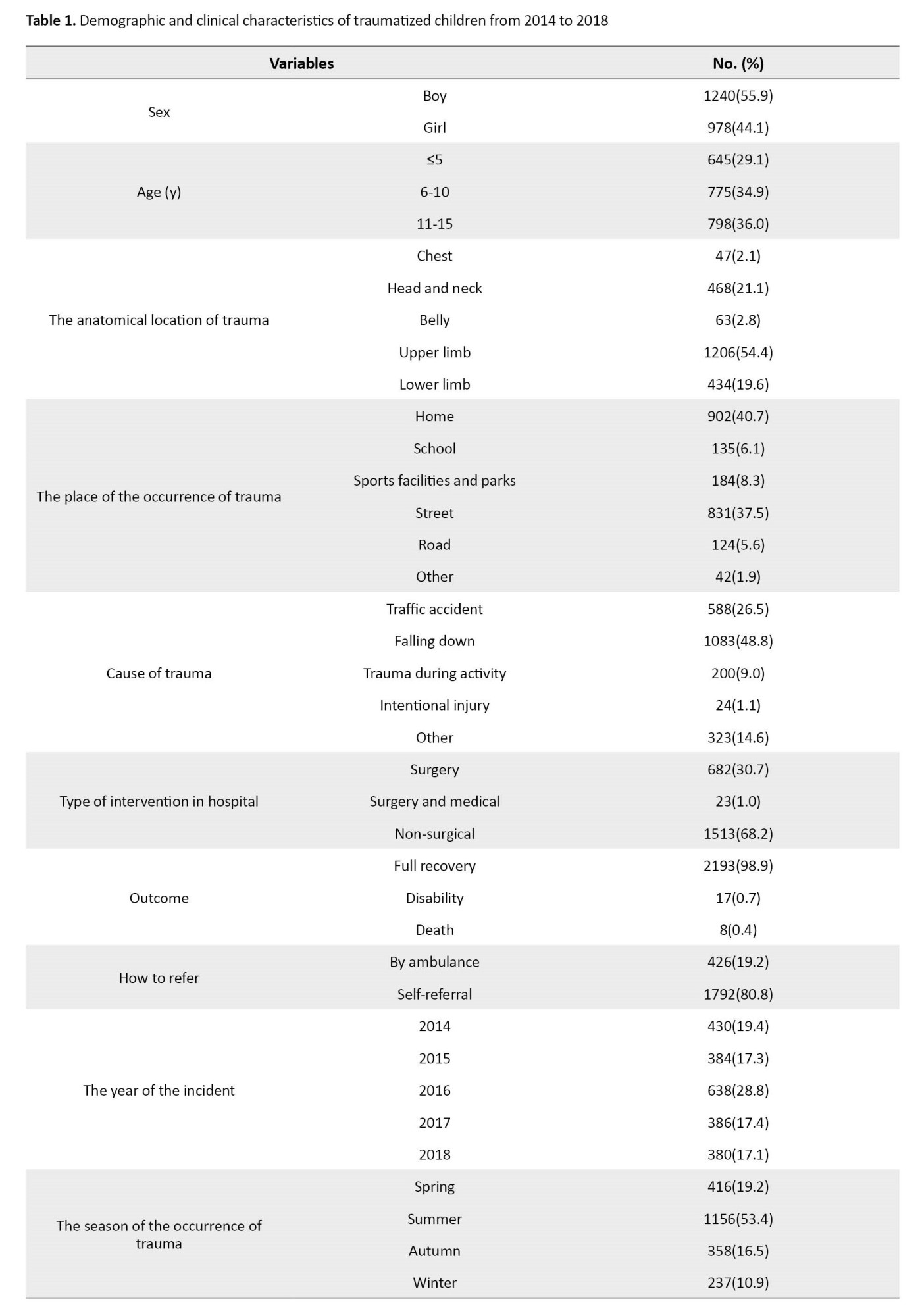
Accordingly, 1240 (55.9%) of the children were boys. Most of the traumatized children were in the age group of 10-15 years. The Mean±SD of the number of hospitalization days in the general ward and intensive care unit was 33.1±13.2 and 11.2±0.39 days, respectively. The most common site of injury was the upper limbs (n=1206 [54.4%]). The home was the most frequent place of occurrence of accidents leading to trauma (n=902 [40.7%]). Falling was the most common event leading to trauma (n=1083 [48.8%]). Also, 98.9% (n=2193) of the children were discharged from the emergency room with full recovery and about 0.4% (n=8) died. The highest number of trauma cases in these 5 years was in 2016 with 28.8% (n=638) and in terms of season, the most common time of trauma was related to summer with 53.4%. Other details can be seen in Table 1.
Table 2 shows the relationship between gender and age with the cause of trauma and its outcome in children under study.
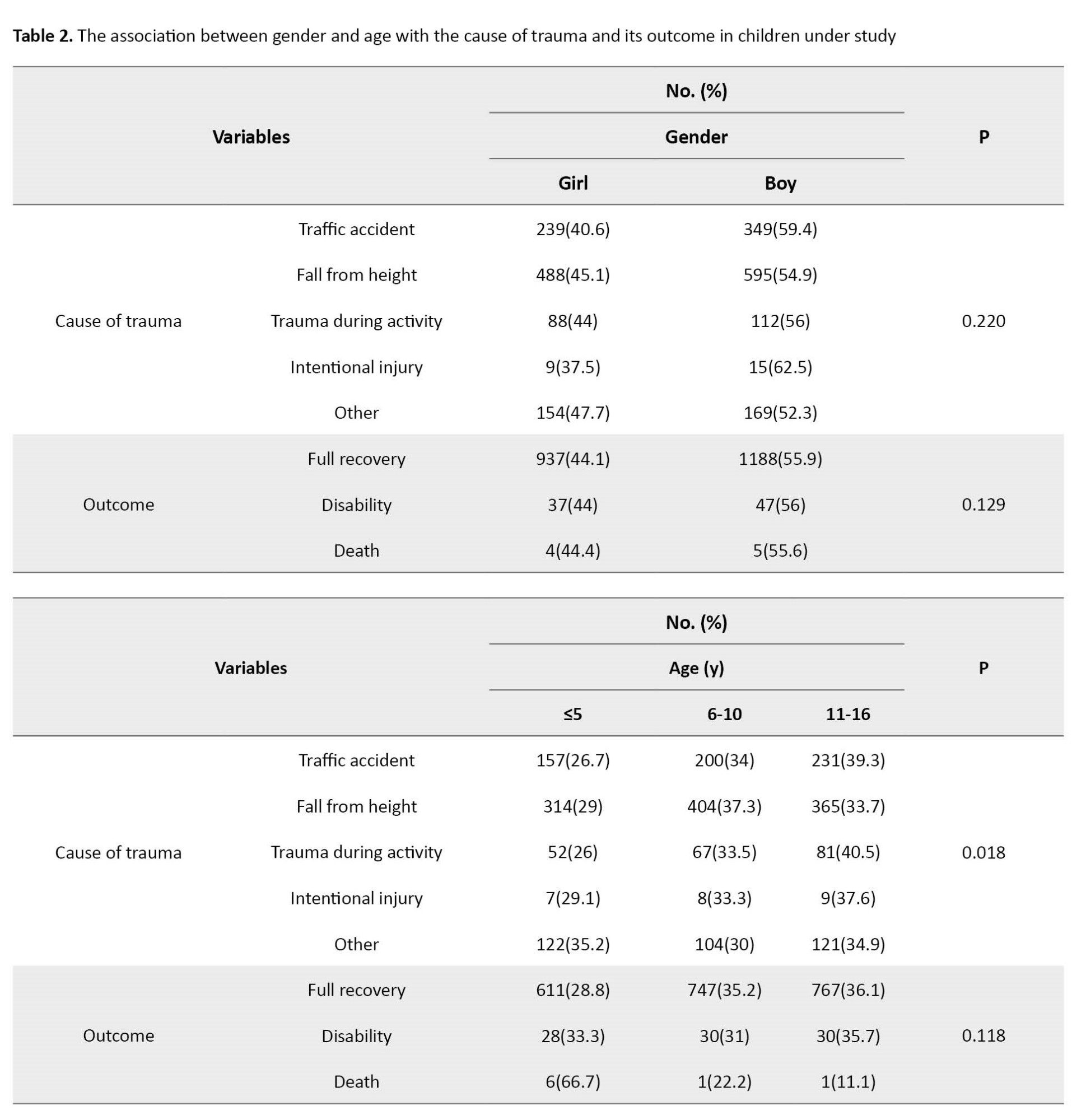
Accordingly, the chi-square test results showed no statistically significant relationship between gender with the cause of trauma and its outcome in traumatized children (P>0.05). Also, there was no statistically significant relationship between age with outcome in traumatized children (P>0.05). However, a statistically significant relationship was observed between the cause of trauma and age so the frequency of all traumatic events in children ≤5 was less than in other age groups (P<0.05).
Discussion
A total of 2218 injured children were examined, of which 55.9% were boys. More than a third of them were in the age group of 10-15 years (36%). The Mean±SD number of hospitalization days in the general ward and intensive care unit were 33.1±13.2 and 11.2±0.39 days, respectively. The most common site of injury was the upper limbs (54.4%). In addition, the home was the most frequent place of occurrence of accidents leading to trauma (40.7%). Most of the children’s traumas occurred in the summer season (53.4%). The most common event leading to trauma was falling (48.8%) and 0.4% died. Also, a statistically significant relationship was observed between the cause of trauma and age (P<0.05).
According to the results of this study, boys were traumatized more than girls. This is in line with studies conducted in different regions. For example, in a study conducted in the United States on more than 1.2 million children referred to the emergency department, 62% of traumatized children were boys [17]. The results of Karbakhsh et al.’s study in Tehran City, Iran, showed that 69.1% of traumatized children were boys [16]. In the study of Mirzaie et al. in Zahedan City, Iran, the incidence rate of hand trauma among boys was reported at 68% [22]. In Saaiq’s study on the cases of burns caused by electrocution of children in Pakistan, the highest frequency (89.41%) was related to boys [23]. Similar values in other studies conducted on this issue emphasize that different forms of trauma are more common in boys than girls [24, 25]. The occurrence of more trauma among boys can be attributed to two factors. On the one hand, boys are more likely to be allowed to be in high-risk situations; additionally, the frequency of high-risk behaviors is higher in boys. For example, the incidence rate of attention deficit hyperactive disorder in boys is about 2 times that of girls, which can lead to an increase in risky behaviors [26].
In the present study, the most common causes of trauma were falling (48.8%) and accidents, respectively. In line with the results of our study, in a study conducted in Tehran City, Iran, the most common cause of trauma in children was falls (50.6%) [16]. In another study conducted by Khorshidi in Hamedan City, Iran, falling was the most common cause of trauma (53%) [27]. In another study in the United Arab Emirates, the main mechanism of injuries leading to hospitalization of children falling was determined [22]. In Odetola’s study in America, domestic accidents, such as falls are the most common cause of children’s trauma, but traffic accidents were reported as the most important cause of trauma that led to children’s hospitalization [17]. Although there are differences in the introduction of the most common cause of trauma in children in different studies; however, in most of the studies, similar to the present study, traffic accidents and falls from heights were responsible for more than 70% of children’s trauma.
In the present study, the upper limbs were determined as the most common anatomical sites of trauma, which is consistent with the studies conducted in this field [17, 27]. However, in some other studies, the most common affected areas in children were head and neck [26, 28]. The reason for this inconsistency is unclear. Because due to the larger head-body ratio in children and the greater resistance of the bone structures of the organs, the probability of head and neck injury is higher [29]. In addition, some of this contradiction may be related to the non-referral of patients with mild trauma to the hospital or the outpatient treatment of these patients outside the hospital [27].
In the present study, most of the children’s trauma cases were related to the summer season (53.4%), which was consistent with similar studies in this field. Asadi et al.’s study in Gilan Province, Iran, as well as Arhami Dolatabadi et al.’s study in Tehran City, Iran, showed that most of the children’s traumas occurred in the summer season [20, 30]. Considering the closure of schools in the summer and the presence of more children at home as well as more trips in this season, the higher amount of trauma is not off the subject.
In the present study, the most common place of trauma was determined as home (44%) followed by the street (35%), which was in line with the results of similar studies [27, 31]. This finding is credible considering the presence of more children in the home compared to other places. In our study, the frequency of all traumatic events in children under 5 years was lower than in other children which was consistent with the results of other studies in this field [20, 27]. The reason for the lower number of traumatic events at this age may be due to the higher level of care received from parents compared to other age groups.
The mortality rate due to trauma among the children in our study was estimated at 0.4%, which was lower compared to other studies conducted in Iran (2.26%) and the United States (1.6%) [16, 32]. The mortality rate of children following trauma is higher than the amount observed in the present study. It is possible that the high intensity of most of the events (especially traffic accidents) as well as the high vulnerability of children led to death in the early moments of the accident before being referred to the hospital. For example, the results of a study indicated that 5.1% of the children who had an accident had died before the rescue forces arrived [22].
Conclusion
According to the results, the most common places of trauma were related to the house and the street due to falls and accidents. Therefore, in addition to informing families of the danger lurking in children, securing homes, and teaching children traffic rules and regulations should be given serious attention.
Study limitations and recommendations
This study faced the following limitations. Firstly, only the cases who were referred to the hospital have been examined, and the information of other patients who died at the scene of the accident or were treated at home or in outpatient centers was not available. Secondly, due to the lack of accurate registration of international classification of disease codes, it was impossible to determine the exact type of injury in some patients the design of the trauma registration system will help to conduct more accurate studies in the future and will increase the effectiveness of preventive strategies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Deputy of the Research and Ethics Committee of Semnan University of Medical Sciences (Code: IR.SEMUMS.REC.1396.213).
Funding
The present article was extracted from the general physician thesis of Elnaz Haidar, approved by School of Medicine, Semnan University of Medical Sciences.
Authors contributions
Conceptualization, supervision, funding acquisition and resources: Mohammadreza Moonesan and Nilufar Safaie; Methodology: Majid Mirmohammadkhani; Data collection: Elnaz Haidar; Data analysis: Kamyar Mansori Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their sincere gratitude to the staff of Kowsar Hospital for their cooperation during the carry-out of this research.
References
- Gerhart JI, Canetti D, Hobfoll SE. Traumatic stress in overview: Definition, context, scope, and long-term outcomes. In: Cherry KE, editor. Traumatic Stress and Long-Term Recovery. Cham: Springer; 2015. [DOI:10.1007/978-3-319-18866-9_1]
- Magruder KM, McLaughlin KA, Elmore Borbon DL. Trauma is a public health issue. European Journal of Psychotraumatology. 2017; 8(1):1375338. [DOI:10.1080/20008198.2017.1375338] [PMID]
- Akbarpour S, Jafari N, Mobasheri F, Pezeshkan P. [Years of life lost due to intentional and unintentional injuries in Mazandaran province in 1387 (Persian)]. Iranian Journal of Epidemiology. 2012; 7(4):29-34. [Link]
- Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Injury Prevention: Journal of the International Society for Child and Adolescent Injury Prevention. 2015; 21(6):434-40. [DOI:10.1136/ip.2005.010983rep] [PMID]
- Goddard A. Adverse childhood experiences and trauma-informed care. Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners. 2021; 35(2):145-55. [DOI:10.1016/j.pedhc.2020.09.001] [PMID]
- Kassam-Adams N, Marsac ML, Hildenbrand A, Winston F. Posttraumatic stress following pediatric injury: Update on diagnosis, risk factors, and intervention. JAMA Pediatrics. 2013; 167(12):1158-65. [DOI:10.1001/jamapediatrics.2013.2741] [PMID]
- Azami-Aghdash S, Ebadifard Azar F, Pournaghi Azar F, Rezapour A, Moradi-Joo M, Moosavi A, et al. Prevalence, etiology, and types of dental trauma in children and adolescents: Systematic review and meta-analysis. Medical Journal of the Islamic Republic of Iran. 2015; 29:234. [PMID]
- Shamohammadi M, Salmanian M, Mohammadi MR, Sadeghi Bahmani D, Holsboer-Trachsler E, Brand S. Prevalence of self-reported trauma in a sample of Iranian children is low and unrelated to parents' education or current employment status. Brazilian Journal of Psychiatry. 2019; 41(3):208-12. [DOI:10.1590/1516-4446-2018-0146] [PMID]
- Mehmood A, Agrawal P, Allen KA, Al-Kashmiri A, Al-Busaidi A, Hyder AA. Childhood injuries in Oman: Retrospective review of a multicentre trauma registry data. BMJ Paediatrics Open. 2018; 2(1):e000310. [DOI:10.1136/bmjpo-2018-000310] [PMID]
- Miele V, Di Giampietro I, Ianniello S, Pinto F, Trinci M. Diagnostic imaging in pediatric polytrauma management. La Radiologia medica. 2015; 120(1):33-49. [DOI:10.1007/s11547-014-0469-x] [PMID]
- Schacherer N, Miller J, Petronis K. Pediatric blunt abdominal trauma in the emergency department: Evidence-based management techniques. Pediatric Emergency Medicine Practice. 2014; 11(10):1-23; quiz 23. [PMID]
- Forouzanfar MH, Sepanlou SG, Shahraz S, Dicker D, Naghavi P, Pourmalek F, et al. Evaluating causes of death and morbidity in Iran, global burden of diseases, injuries, and risk factors study 2010. Archives of Iranian Medicine. 2014; 17(5):304–20. [PMID]
- Khazaei Z, Khazaei S, Valizadeh R, Mazharmanesh S, Mamdohi S, Rahimi Pordanjani S, et al. The epidemiology of injuries and accidents in children under one year of age, during (2009-2016) in Hamadan Province, Iran. International Journal of Pediatrics. 2016; 4(7):2213-20. [DOI:10.22038/ijp.2016.7014]
- Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012; 32(2):122-38. [DOI:10.1016/j.cpr.2011.12.001] [PMID]
- Pino PS, San Juan Hurtado L, Monasterio Ocares MC. Pediatric trauma and its relation to social health determinants. Infermeria Global. 2013; 328-35. [Link]
- Karbakhsh M, Zargar M, Zarei MR, Khaji A. Childhood injuries in Tehran: A review of 1281 cases. The Turkish Journal of Pediatrics. 2008; 50(4):317. [PMID]
- Odetola FO, Gebremariam A. Paediatric trauma in the USA: Patterns of emergency department visits and associated hospital resource use. International Journal of Injury Control and Safety Promotion. 2015; 22(3):260-6. [DOI:10.1080/17457300.2014.925937] [PMID]
- Naidoo N, Muckart DJ. The wrong and wounding road: Paediatric polytrauma admitted to a level 1 trauma intensive care unit over a 5-year period. South African Medical Journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2015; 105(10):823-6. [DOI:10.7196/SAMJnew.8090] [PMID]
- Yadollahi M, Mohammadinia L, Norouzi M. Epidemiology of trauma in children and adolescents based on emergency medical services (EMS 115) in Shiraz, 2017. Journal of Health Sciences & Surveillance System. 2022; 10(4):488-94. [DOI:10.30476/jhsss.2021.92240.1329]
- Dolatabadi AA, Mohseninia N, Amiri M, Motamed H, Asl AH. Pediatric trauma patients in Imam Hossein emergency department; an epidemiologic study. Iranian Journal of Emergency Medicine. 2016; 3:4-8. [DOI: 10.22037/ijem.v3i1.10971]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990- 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020; 396(10258):1204-22. [DOI:10.1016/S0140-6736(20)30925-9] [PMID]
- Mirzaie M, Parsa A, Salehi M, Dahmardehei M, Moghadam MH, Mirzaie N. Epidemiology of hand injuries in children presenting to an orthopedic trauma center in southeast of Iran. The Archives of Bone and joint Surgery. 2014; 2(3):225-31. [PMID]
- Saaiq M. Epidemiology and outcome of childhood electrical burn injuries at Pakistan Institute of Medical Sciences Islamabad, Pakistan. Journal of Burn Care & Research: Official Publication of the American Burn Association. 2016; 37:e174-80. [DOI:10.1097/BCR.0000000000000202] [PMID]
- Othman N, Kendrick D, Al-Windi A. Childhood burns in Sulaimaniyah province, Iraqi Kurdistan: A prospective study of admissions and outpatients. Burns: Journal of the International Society for Burn Injuries. 2015; 41(2):394-400. [DOI:10.1016/j.burns.2014.07.008] [PMID]
- Ma SH, Ang MD, Chang YT, Dai YX. Association between vitiligo and hearing loss. Journal of the American Academy of Dermatology. 2021; 85(6):1465-72. [DOI:10.1016/j.jaad.2020.12.029] [PMID]
- Mohamed ES, Said EA, Sayed DS, Awad SM, Ahmed MH. Auditory system dysfunction in patients with vitiligo: Is it a part of a systemic autoimmune process? The Egyptian Journal of Otolaryngology 2017; 33:594-602. [DOI:10.4103/ejo.ejo_6_17]
- Khorshidi H, Daneshyar S, Eslami ZS, Moradi A. [Epidemiolog of pediatric trauma in Hamedan, Iran (2016-2017) (Persian)]. Journal of Gorgan University of Medical Sciences. 2019; 21(2):99-105. [Link]
- Kawakami T, Hashimoto T. Disease severity indexes and treatment evaluation criteria in vitiligo. Dermatology Research and Practice. 2011; 2011:750342. [DOI:10.1155/2011/750342] [PMID]
- Abantanga FA, Mock CN. Childhood injuries in an urban area of Ghana a hospital-based study of 677 cases. Pediatric Surgery International. 1998; 13:515-8. [DOI:10.1007/s003830050387] [PMID]
- Asadi P, Asadi K, Rimaz S, Monsef-Kasmaie V, Zohrevandi B, Mohtasham-Amiri Z. Epidemiology of trauma in children admitted to Poursina Teaching Hospital. Journal of Guilan University of Medical Sciences. 2015; 23(S1):9-15. [Link]
- Oboirien M. Pattern of paediatric trauma in Sokoto, North West Nigeria. African Journal of Paediatric Surgery: AJPS. 2013; 10(2):172-5. [DOI:10.4103/0189-6725.115047] [PMID]
- Brown RL. Epidemiology of injury and the impact of health disparities. Current Opinion in Pediatrics. 2010; 22(3):321-5. [DOI:10.1097/MOP.0b013e3283395f13] [PMID]
Type of Study: Original Article |
Subject:
Emergency Medicine
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









