Volume 12, Issue 2 (Spring 2024)
Iran J Health Sci 2024, 12(2): 131-140 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Veiskarami P, Roozbahani M, Mortazavi I. Development of Language and Social Skills in Hearing-impaired Children With and Without Rehabilitation. Iran J Health Sci 2024; 12 (2) :131-140
URL: http://jhs.mazums.ac.ir/article-1-920-en.html
URL: http://jhs.mazums.ac.ir/article-1-920-en.html
Department of Motor Behavior, Faculty of Humanites, Borujerd Branch, Islamic Azad University, Borujerd, Iran. , Mehdi.roozbahani@iau.ac.ir
Full-Text [PDF 877 kb]
(1355 Downloads)
| Abstract (HTML) (2810 Views)
Full-Text: (1218 Views)
Introduction
In recent years, early diagnosis and timely intervention in developmental disorders have received much attention, and more emphasis is placed on diagnosing disabilities at a younger age, especially in infancy and childhood, i.e. from birth to two years old [1, 2]. The World Health Organization (WHO) noted in a 1966 report that screening children was necessary to identify developmental disorders [3]. Development has various aspects, including physical, emotional, motor, language, personal-social, and cognitive, that interact with each other [4]. For example, a physically-impaired child can also be affected by emotional, motor, and cognitive aspects [5].
Language development is one of the components of development that is particularly important. Language learning is a natural, unique human developmental process by which a child learns his mother tongue as the first language. Moreover, language is not only a means of communicating ideas and thoughts but also creates cultural ties, friendships, and economic relations [6].
Another essential development component is personal and social skills. Social skills are acquired through social behaviors; they help people interact with others to stimulate positive reactions and hinder negative ones [7]. Psychologists believe that the first years of a person’s life are the foundation of his future life because, at this stage, the children realize themselves from others [8]. Like other components, social development is closely related to other aspects of development. The child’s language, communication, and social functions development, which are related to each other, play a crucial role in the child’s development [7]. Therefore, the future of human society depends on children’s physical and psychological development [9]. However, 18% to 16% of children in different societies suffer from speech and language disabilities, learning disabilities, and emotional or behavioral disorders. In comparison, only 20% to 30% of children with all developmental-behavioral disorders are diagnosed before school age. About 70% to 80% of these children are not referred for early intervention services due to the lack of timely diagnosis of these problems during primary health care [10].
One of the most important physical aspects is the sense of hearing, which may affect other development components. Achieving speech, cognition, behavior, and social development in the early stages of life requires auditory input and communication [11]. Hearing loss is common in childhood and may significantly affect speech, social, and physical development [12]. Children with hearing loss exhibit more behavior problems than normal children. Once the language abilities of children with hearing loss are considered, the adverse effects of hearing loss on behavior disappear. Behavioral problems are found more commonly in children with hearing loss, and behavioral problems are highest amongst those with hearing loss with the least developed language capabilities [13].
A person is identified as having hearing loss when he or she cannot hear a pure tone with an intensity of 25 dB in at least one ear. Hearing tests are recommended to diagnose hearing loss in all infants. Hearing problems fall into three categories: Conductive, sensory-neural, and central hearing loss [14]. The prevalence of bilateral, moderate to severe, and persistent sensory neural deafness in infants ranges from 0.5 to 1 per 1000 live births. Hearing loss can occur at any age due to various factors, so the prevalence in children under 6 is between 1.5 and 2 per 1000 [15].
Fortunately, timely identification and support for newborns with hearing difficulties are now possible by the worldwide adoption of the neonatal hearing screening scheme. After the diagnosis of hearing loss, the next step is to start the intervention and rehabilitation process. First, an auditory function is optimized through the suitable selection of hearing aids, and then, the rehabilitation phase begins. Different hearing rehabilitation programs try to restore capabilities, preserve the deaf individual’s dignity, and establish their legal and social standing [16]. Rehabilitation also attends to other needs and abilities beyond the physical or mental conditions that hinder a disabled person’s functioning. Recently, in addition to the disabled person, much attention has been paid to the social environment in which the person lives because it is the social environment that largely determines the consequences of the disability [17].
Many studies have been done on children’s language and social skills development, but most of these studies have been in the children’s age group over three years. Therefore, we decided to study the development of language and personal-social skills in children with normal hearing (NHC), rehabilitated hearing-impaired children (RHIC), and non-rehabilitated hearing-impaired children (NRHIC) aged 6 to 18 months according to the Denver 2 scale [18].
Materials and Methods
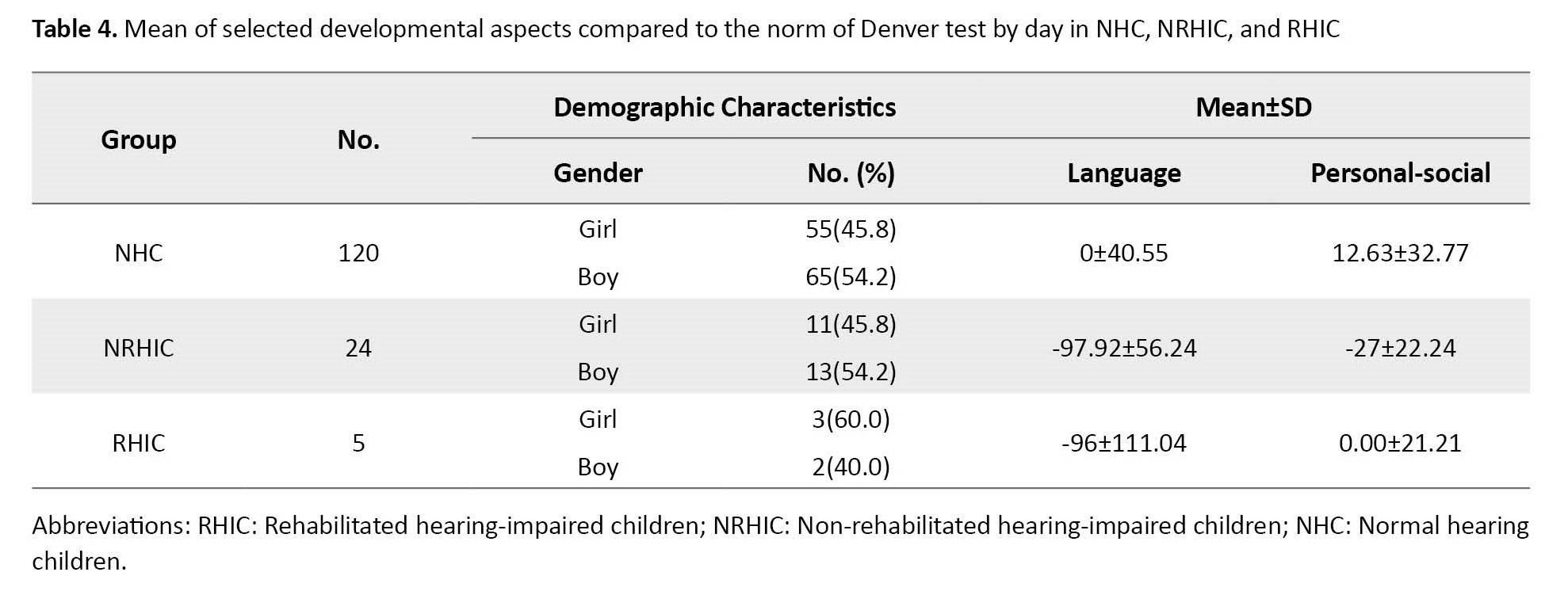
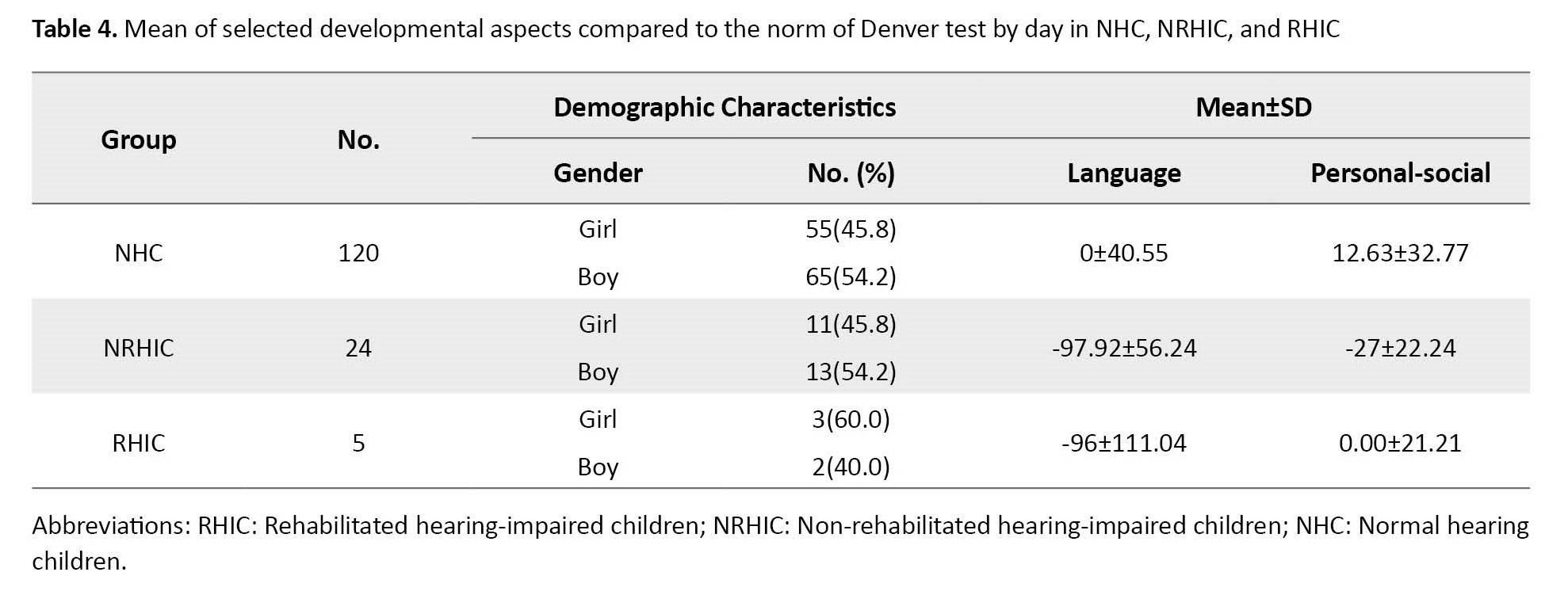
This cross-sectional study was conducted from 2020 to 2021 in Khorramabad City, Lorestan Province, Iran. We used convenience sampling to choose 120 NHC children with healthy physical conditions, comprising 55 girls (45.8%) and 65 boys (54.2%). Also, we included 24 NRHIC, consisting of 11 girls (45.8%) and 13 boys (54.2%). Finally, we recruited 5 RHIC, with 3 girls (60%) and two boys (40%). The hearing threshold of hearing-impaired children participating in this project was 90 to 120 dB, and they lacked any accompanying disorders. Non-rehabilitated hearing-impaired children were identified as hearing-impaired in the hearing screening program but did not enter the appropriate rehabilitation intervention phase during the project follow-up. In this study, the rehabilitated hearing-impaired group consisted of children who received rehabilitation services from special centers for the hearing-impaired after being diagnosed with deafness. The services offered include hearing aids, lip reading, speech reading, and other relevant skills that can be used for at least three months. The study population comprised all children aged 6 to 18 months identified through newborn hearing screening test sites in Khorramabad City, Iran. The reported issues varied from mild hearing loss in one ear to severe bilateral hearing loss. The inclusion criteria for the NHC group included overall good health, normal hearing, age 6-18 months, and parental consent. For the NRHIC group, the inclusion criteria comprised severe to profound hearing loss and the child’s general health. For the RHIC group. The inclusion criteria comprised severe to profound hearing loss, receiving appropriate hearing rehabilitation services for at least 3 months. Children with accompanying disabilities (other than hearing loss, for example, autism or blindness, attention-deficit/hyperactivity disorder, etc.) or their parents refused to do the tests and also, children with mild to moderate or unilateral hearing loss were excluded from the plan. Also, children with mild to moderate or unilateral hearing loss were excluded from the plan.
Therefore, according to this project’s inclusion and exclusion criteria, the study only recruited a small number of samples of both rehabilitated and non-rehabilitated hearing-impaired children.
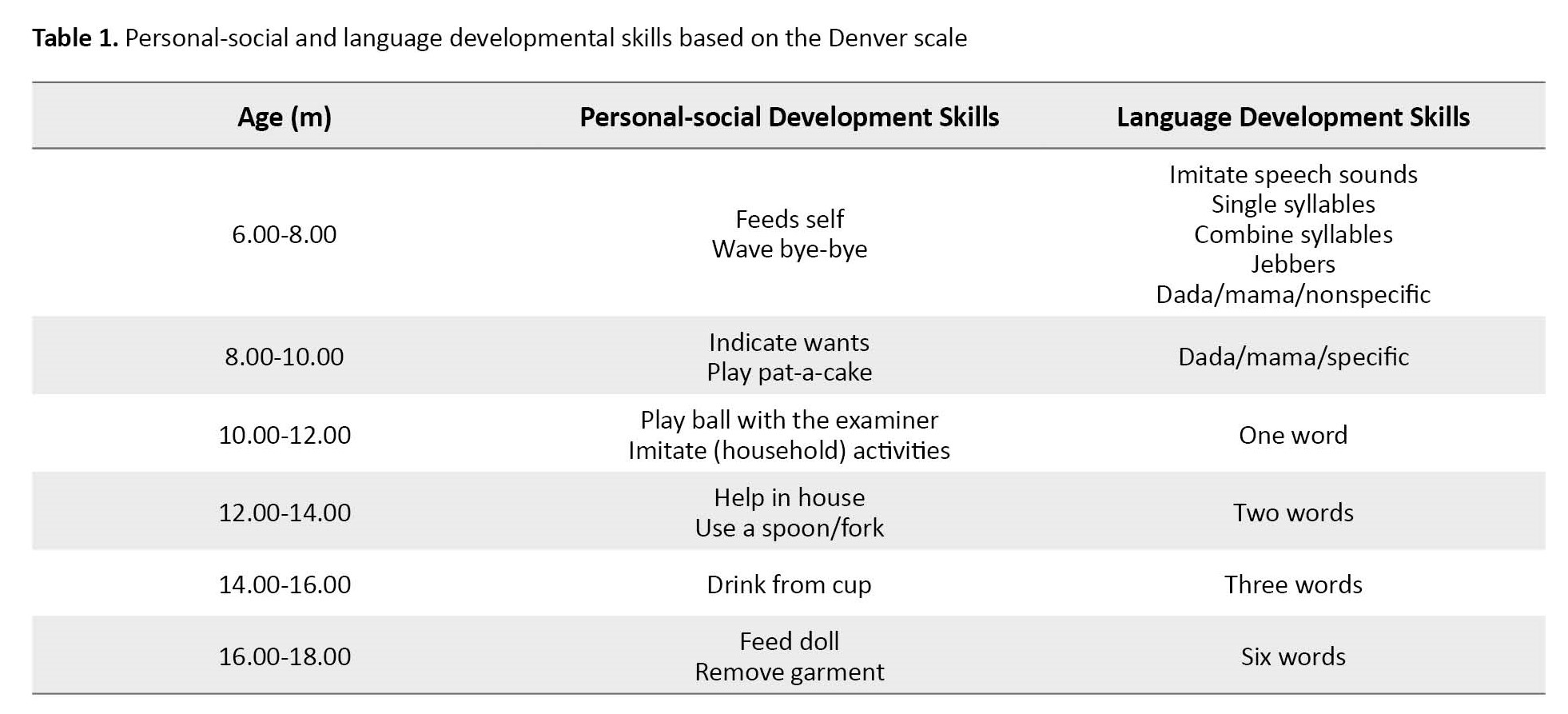
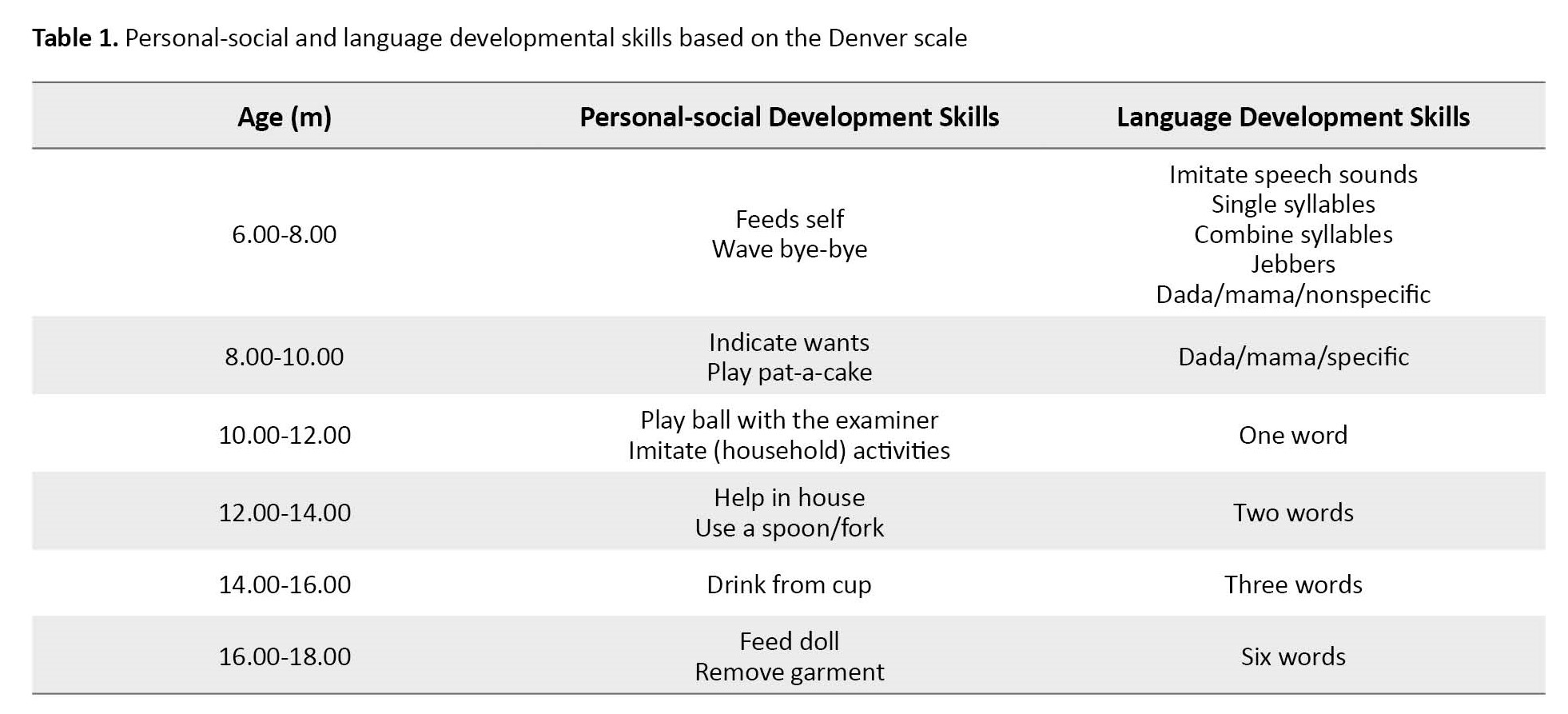
The Denver development screening test 2 (DDST-II) was employed to measure development assignments in this project. In 1967, Frankenberg et al. designed the Denver test, which underwent revision and standardization in 1990. The test consists of 125 items and is designed to assess children from birth to 6 years of age across 4 aspects: Personal-social development, fine motor development, language development, and gross motor development. The test assesses developmental tasks and skills based on the natural order in which they typically appear in children [18]. The chart provides information on the ages at which 25% to 50%, 50% to 75%, and 75% to 90% of Denver children have completed each task. This study considers the age range in which 50% to 75% of children could perform the task as the norm. The validity and reliability of the DDST-II have been confirmed in Iran [19]. According to the Denver test, children aged 6 to 18 months are assessed for 9 language development skills, while personal-social and language development are evaluated through 11 skills [20]. This project carried out developmental tasks for each child’s age (Table 1).
Demographic data were initially collected for all children at the Central Audiology Clinic of Khorramabad, following all COVID-19 protocols. Then, eligible participants underwent diagnostic hearing assessments, including otoacoustic emissions (OAE), auditory brainstem response (ABR), auditory steady-state response (ASSR), and behavioral audiometry when necessary. The child’s personal-social and developmental language skills were then evaluated using the DDST-II appropriate for their age. OAE was employed as one of the tests in this study. A passing result on this test indicated normal hearing sensitivity, while a failing result prompted referral for further diagnostic hearing evaluations. ABR was the next test. The presence of wave V at an intensity of 25-30 dB confirms normal hearing in the child, whereas the absence of ABR waves at higher intensities results in additional diagnostic tests. Lastly, ASSR was conducted on children referred for ABR testing to confirm the final diagnosis of hearing loss. Behavioral audiometry involves observing the child’s responses to sounds produced by sound makers (a drum for low-frequency sounds and a bell for high-frequency sounds).
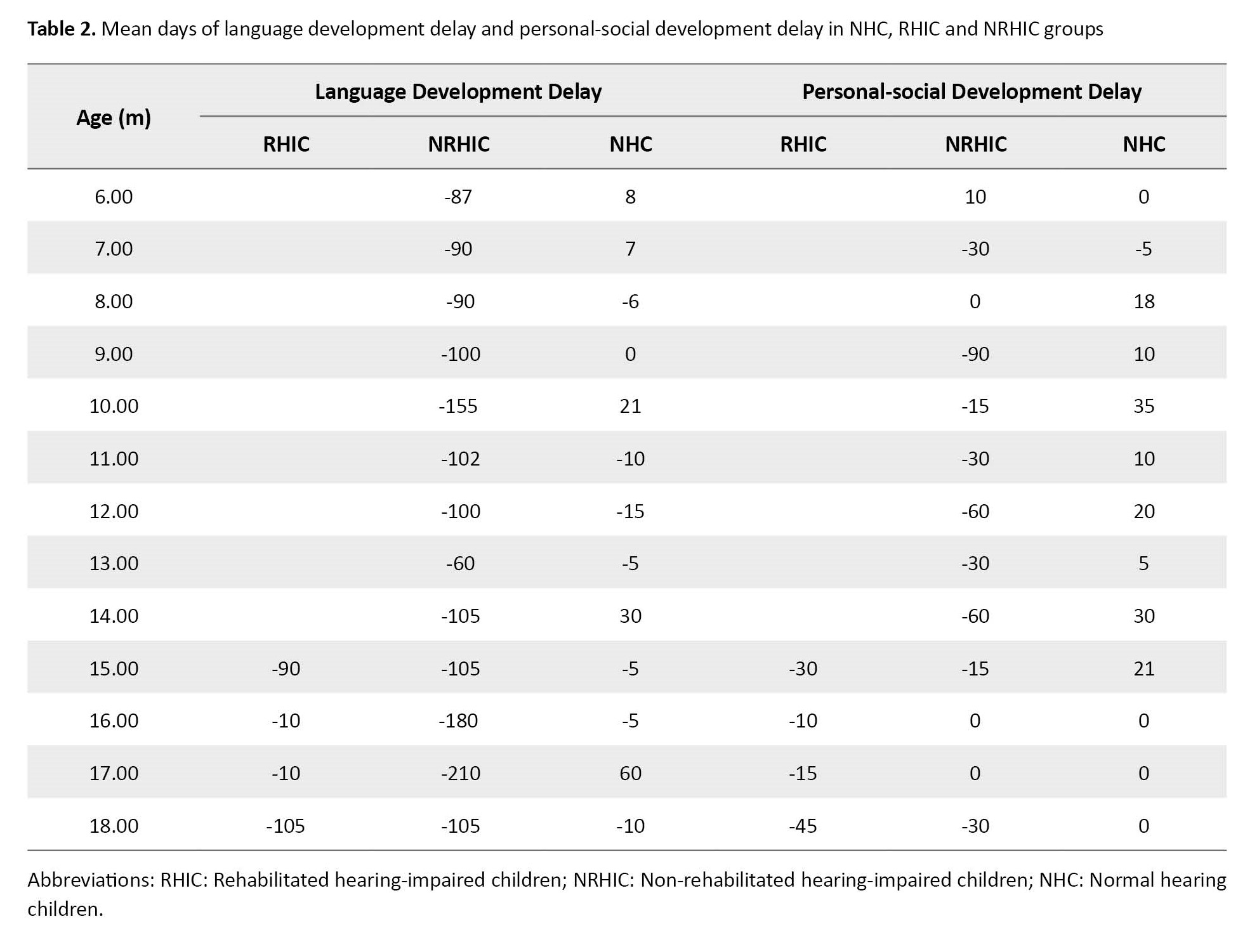
A vertical line was drawn on the Denver chart sheet according to the child’s calendar age. The test date was recorded to evaluate language and personal-social development with the DDST-II. Then, all the items in each section (personal-social and developmental language skills), the age line passes through them performed. A “P” would be recorded in the column if the child completed the task, and an “F” if the child did not. Following the examiner’s instructions, the child performed the skill and scored 1 for passing or 0 for failing. In this research, if 50% to 75% of Denver’s typical children could accomplish the task, it was considered the standard for a child’s expected ability (all three groups involved in the study). Data from the Denver assessment were analyzed based on latency, absence of delay, or children’s developmental progress per day (Table 2).
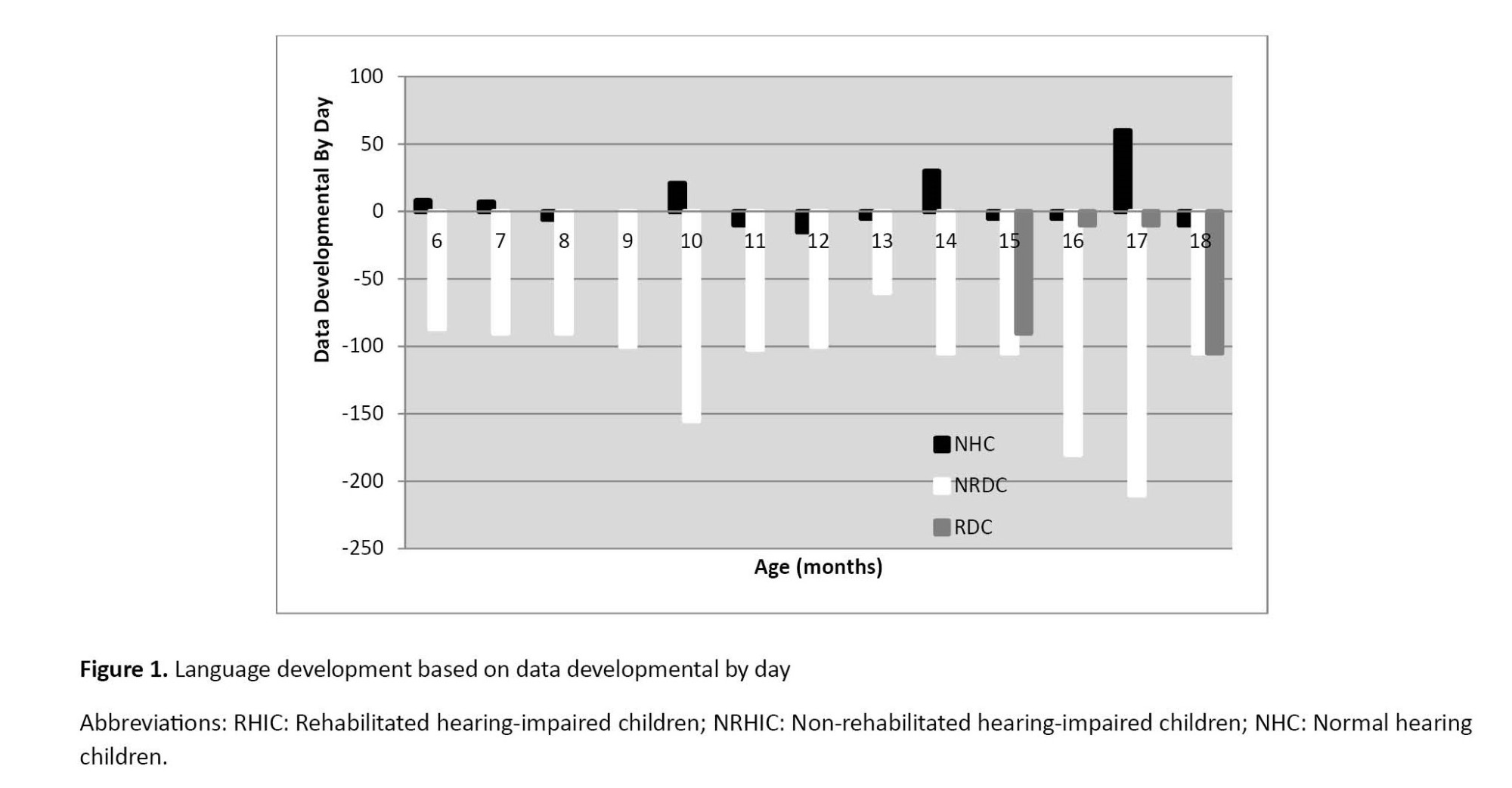
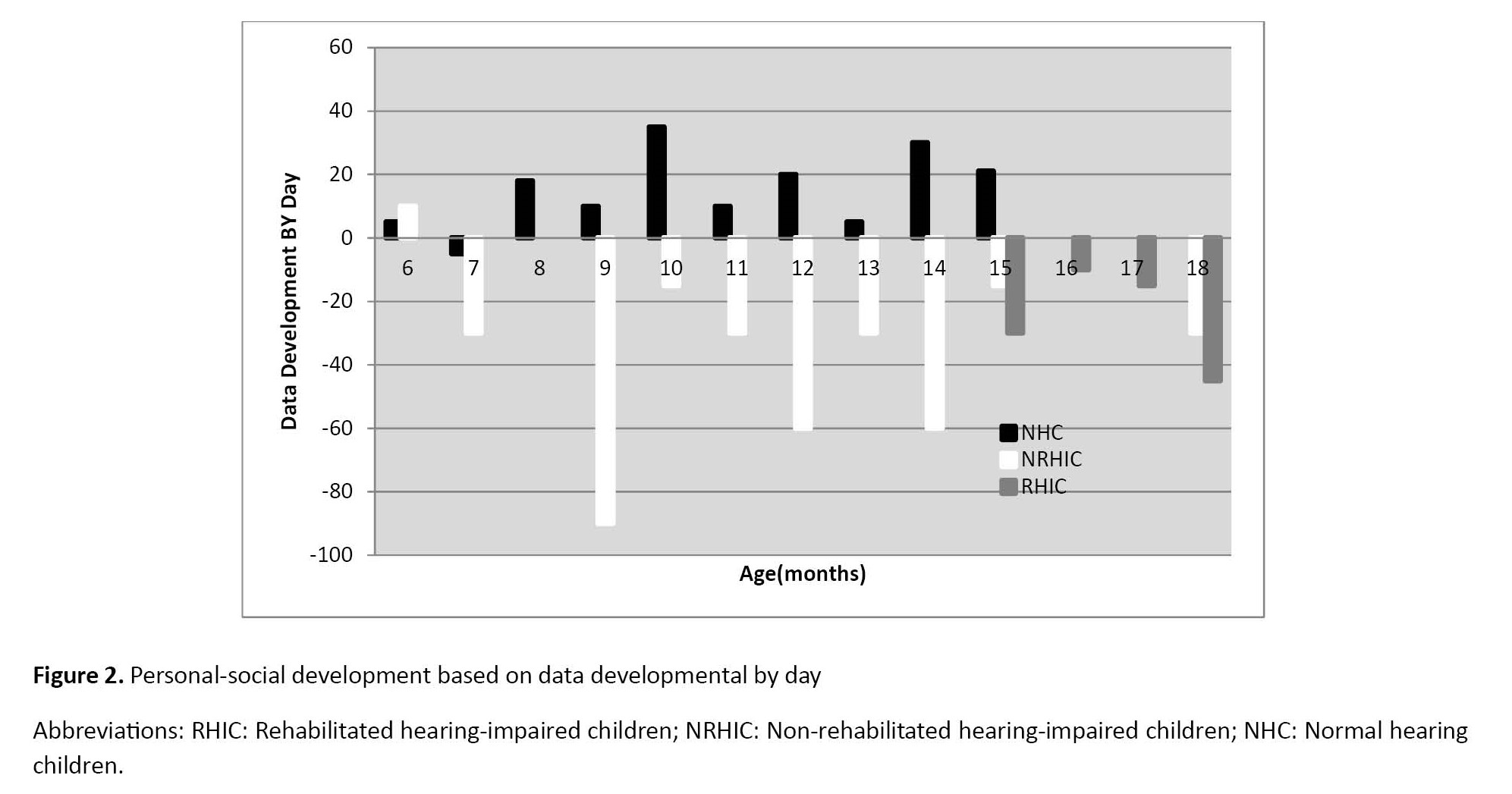
A positive symbol next to the number of days indicates improvement in the chosen developmental aspect compared to the Denver sample. Conversely, a negative symbol suggests a delay in the developmental aspect selected compared to the Denver sample (Figures 1 and 2).
A zero marks that the participant’s development is on par with the Denver sample.
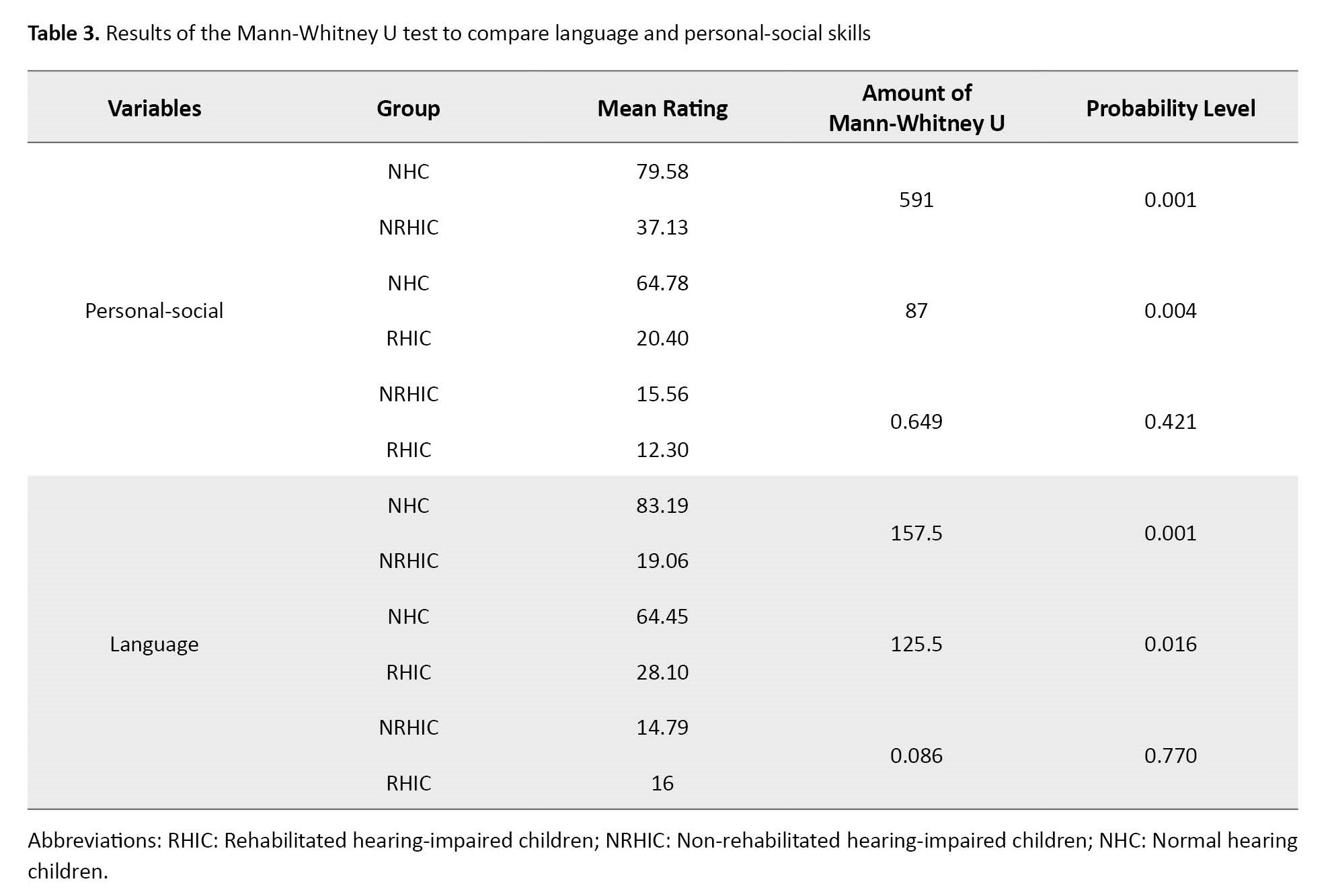
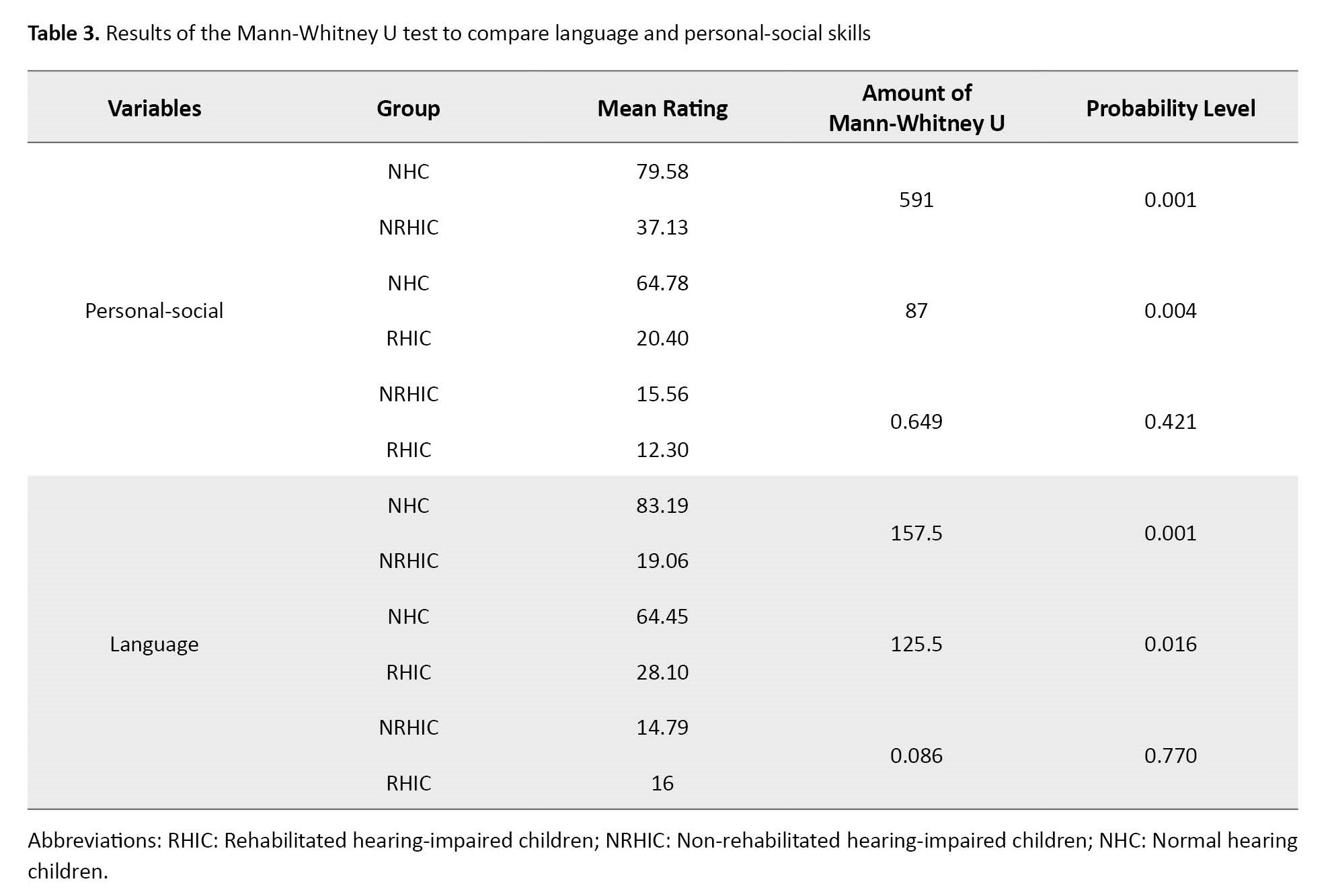
Data analysis was performed based on the number of days of delay or progress of children’s personal-social and language skills development compared to the Denver scale (Table 2). The Kruskal-Wallis and Mann-Whitney non-parametric tests were used to analyze daily developmental data (Table 3).
Results
The results showed a statistically significant difference between language development in the NHC group and hearing-impaired children groups: NRIHC (P=0.001) and RIHC (P=0.016). The development of personal-social skills between the NHC group and RHIC (P=0.004) and NRHIC (P=0.001) was statistically significant. However, the difference in these two developmental aspects, language (P=0.770) and personal social (P=0.0421), between the two hearing-impaired groups was not significant (P≤0.05) (Tables 2 and 4).
Figures 1 and 2 show the participants’ delay, non-delay, or advanced development based on the day’s developmental data. NHC children are above the midline with a positive score, while some have a negative score below the midline. The statistical analysis reveals no significant difference between the language and personal-social development in NHC and Denver samples. Additionally, Figure 1 shows that the language development scores in NRHIC and RHIC groups are constantly below the midline with a negative score. Similarly, in Figure 2, the personal-social development scores in the NRHIC and RHIC groups are below the midline with a negative score.
Discussion
Based on the results of this study, the presence of hearing impairment in early childhood, in other words, in the pre-language stage, delays the development of language and social skills. Therefore, to compensate for this delay, solving the hearing problem and rehabilitating the affected children is necessary. The child should also be treated from the very beginning of childhood and immediately after the diagnosis of hearing loss. The global emphasis on timely hearing problem diagnosis and rehabilitation will be discussed in the following. Then, the causes of delay in rehabilitating the children participating in this study will be examined.
According to the American Hearing and Speech Association (ASHA), hearing-impaired children should undergo hearing rehabilitation following the diagnosis of hearing loss. Language and speech development are affected regardless of the cause of the hearing loss (whether acquired or congenital) [21]. It is recommended that hearing rehabilitation be begun within 6 months, as delayed participation may impact the results [16]. The age of children receiving hearing rehabilitation plays a significant role in the outcomes, affecting emotional, social, linguistic, and speech development [22].
Before implanting or using a hearing aid, children with pre-lingual deafness experience a period of auditory deprivation, limiting their speech access (vocabulary). It is often hypothesized that prolonged periods of auditory deprivation will result in significant delays in vocabulary size [23]. This hypothesis is supported by studies demonstrating a negative relationship between age at implantation and vocabulary size [24-26].
The length of auditory deprivation also appears to affect developmental rates in vocabulary. Studies by Shakrawal et al. (2022) showed that great communication benefits were achieved by early implantation without hearing aid use; the results exemplify the importance of enhanced social environments provided by everyday life experience for human brain development and reassure parents considering cochlear implants where hearing aid and speech training is unavailable [27].
The consensus among cochlear implant (CI) researchers is that receiving a CI after age two is late, whereas receiving a CI before one year is early [28]. There is a strong connection between language and motor systems, so young children can discover new objects and practice language through acquiring motor skills [29].
On the other hand, deaf children have delayed fine and gross motor development [30]. Thus, delays in language development can be related to delays in motor development.
In Khoramabad (project area), despite increasing knowledge about the importance of early intervention and rehabilitation in hearing care, many children have arrived too late to receive a hearing aid and begin a hearing rehabilitation program. We found that out of the 29 deaf children, 19 were diagnosed with hearing problems before 3 months, 8 between 3 and 6 months, and only one after 6 months. This finding highlights the effectiveness of the global hearing screening program. Timely and accurate assessment after diagnosis can prevent hearing loss from becoming a disability in the future for hearing-impaired children. However, only 5 children had access to rehabilitation services. Delays and deficiencies in hearing rehabilitation services impair the success of neonatal hearing screening programs. Among the 29 deaf children, 8 had a family member who was deaf (first or second degree), and 21 came from families without prior experience with hearing impairment, often leading to resistance in accepting their child’s hearing loss. This resistance can result in missed opportunities for timely treatment and rehabilitation for the child.
Finally, it is essential to underline that auditory training falls under hearing rehabilitation. However, the excessive focus of the rehabilitation team on this aspect has resulted in the neglect of other crucial components of auditory rehabilitation, such as motor development and personal-social skills.
Numerous studies have addressed the deficiencies in social skills among individuals with hearing impairments. These studies have highlighted the significance of education, acquisition, and application of social skills and their promotion [31]. Regrettably, the level of education among parents in all three participant groups was moderate, with a few having postgraduate education. Furthermore, concerning employment, the majority had unstable jobs, such as manual labor, gardening, painting, and seasonal work. These findings reflect the unfavorable economic conditions of households in the city under investigation. The rising costs of hearing aids, treatment, and rehabilitation classes may contribute to the limited number of children undergoing rehabilitation. Economic sanctions in Iran have increased expenses for hearing aids and cochlear implants. The COVID-19 pandemic has further exacerbated the situation by reducing resources available for children, as hearing training centers have closed, leaving only online education. The global neonatal hearing screening program advocates for prompt evaluation and intervention within the first few months after birth following a diagnosis of hearing loss for effective hearing rehabilitation.
Conclusion
Delays in language and social skills development are evident in hearing-impaired children at an early age, so rehabilitation should start early in childhood. Health is a complex and comprehensive system that requires an interdisciplinary approach to address its multiple determinants. In rehabilitating deaf children, attention should be paid to all aspects of development, which requires the cooperation of specialists in different treatment fields. Also, the Denver-II screening test is recommended to assess language and skills development in health centers and centers specialized for hearing-impaired children aged 6 to 18 months.
Study limitations
Due to the spread of COVID-19, families were unwilling to go to the center for hearing and developmental assessment tests, especially the parents of deaf children. On the other hand, children who were identified as having severe to profound hearing loss used online services due to the COVID-19 pandemic and the suspension of hearing training centers. However, the online programs were not as effective as face-to-face meetings. Therefore, very few children benefited from appropriate hearing training and the conditions for participating in the study.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Islamic Azad Unversity, Boroujerd Branch (Code: IR.IAU.B.REC.1400.007).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and supervision: Parvin Veisarami and Mehdi Roozbahai; Methodology: Parvin Veiskarami and Ideh Mortazavi; Funding acquisition and resources: Parvin Veiskarami, Mehdi Roozbahai and Ideh Mortazavi; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank the neonatal hearing screening program officials in the Welfare Organization of Lorestan Province for their cooperation in achieving the desired statistical population despite the limitations caused by the COVID-19 epidemic.
References
In recent years, early diagnosis and timely intervention in developmental disorders have received much attention, and more emphasis is placed on diagnosing disabilities at a younger age, especially in infancy and childhood, i.e. from birth to two years old [1, 2]. The World Health Organization (WHO) noted in a 1966 report that screening children was necessary to identify developmental disorders [3]. Development has various aspects, including physical, emotional, motor, language, personal-social, and cognitive, that interact with each other [4]. For example, a physically-impaired child can also be affected by emotional, motor, and cognitive aspects [5].
Language development is one of the components of development that is particularly important. Language learning is a natural, unique human developmental process by which a child learns his mother tongue as the first language. Moreover, language is not only a means of communicating ideas and thoughts but also creates cultural ties, friendships, and economic relations [6].
Another essential development component is personal and social skills. Social skills are acquired through social behaviors; they help people interact with others to stimulate positive reactions and hinder negative ones [7]. Psychologists believe that the first years of a person’s life are the foundation of his future life because, at this stage, the children realize themselves from others [8]. Like other components, social development is closely related to other aspects of development. The child’s language, communication, and social functions development, which are related to each other, play a crucial role in the child’s development [7]. Therefore, the future of human society depends on children’s physical and psychological development [9]. However, 18% to 16% of children in different societies suffer from speech and language disabilities, learning disabilities, and emotional or behavioral disorders. In comparison, only 20% to 30% of children with all developmental-behavioral disorders are diagnosed before school age. About 70% to 80% of these children are not referred for early intervention services due to the lack of timely diagnosis of these problems during primary health care [10].
One of the most important physical aspects is the sense of hearing, which may affect other development components. Achieving speech, cognition, behavior, and social development in the early stages of life requires auditory input and communication [11]. Hearing loss is common in childhood and may significantly affect speech, social, and physical development [12]. Children with hearing loss exhibit more behavior problems than normal children. Once the language abilities of children with hearing loss are considered, the adverse effects of hearing loss on behavior disappear. Behavioral problems are found more commonly in children with hearing loss, and behavioral problems are highest amongst those with hearing loss with the least developed language capabilities [13].
A person is identified as having hearing loss when he or she cannot hear a pure tone with an intensity of 25 dB in at least one ear. Hearing tests are recommended to diagnose hearing loss in all infants. Hearing problems fall into three categories: Conductive, sensory-neural, and central hearing loss [14]. The prevalence of bilateral, moderate to severe, and persistent sensory neural deafness in infants ranges from 0.5 to 1 per 1000 live births. Hearing loss can occur at any age due to various factors, so the prevalence in children under 6 is between 1.5 and 2 per 1000 [15].
Fortunately, timely identification and support for newborns with hearing difficulties are now possible by the worldwide adoption of the neonatal hearing screening scheme. After the diagnosis of hearing loss, the next step is to start the intervention and rehabilitation process. First, an auditory function is optimized through the suitable selection of hearing aids, and then, the rehabilitation phase begins. Different hearing rehabilitation programs try to restore capabilities, preserve the deaf individual’s dignity, and establish their legal and social standing [16]. Rehabilitation also attends to other needs and abilities beyond the physical or mental conditions that hinder a disabled person’s functioning. Recently, in addition to the disabled person, much attention has been paid to the social environment in which the person lives because it is the social environment that largely determines the consequences of the disability [17].
Many studies have been done on children’s language and social skills development, but most of these studies have been in the children’s age group over three years. Therefore, we decided to study the development of language and personal-social skills in children with normal hearing (NHC), rehabilitated hearing-impaired children (RHIC), and non-rehabilitated hearing-impaired children (NRHIC) aged 6 to 18 months according to the Denver 2 scale [18].
Materials and Methods
This cross-sectional study was conducted from 2020 to 2021 in Khorramabad City, Lorestan Province, Iran. We used convenience sampling to choose 120 NHC children with healthy physical conditions, comprising 55 girls (45.8%) and 65 boys (54.2%). Also, we included 24 NRHIC, consisting of 11 girls (45.8%) and 13 boys (54.2%). Finally, we recruited 5 RHIC, with 3 girls (60%) and two boys (40%). The hearing threshold of hearing-impaired children participating in this project was 90 to 120 dB, and they lacked any accompanying disorders. Non-rehabilitated hearing-impaired children were identified as hearing-impaired in the hearing screening program but did not enter the appropriate rehabilitation intervention phase during the project follow-up. In this study, the rehabilitated hearing-impaired group consisted of children who received rehabilitation services from special centers for the hearing-impaired after being diagnosed with deafness. The services offered include hearing aids, lip reading, speech reading, and other relevant skills that can be used for at least three months. The study population comprised all children aged 6 to 18 months identified through newborn hearing screening test sites in Khorramabad City, Iran. The reported issues varied from mild hearing loss in one ear to severe bilateral hearing loss. The inclusion criteria for the NHC group included overall good health, normal hearing, age 6-18 months, and parental consent. For the NRHIC group, the inclusion criteria comprised severe to profound hearing loss and the child’s general health. For the RHIC group. The inclusion criteria comprised severe to profound hearing loss, receiving appropriate hearing rehabilitation services for at least 3 months. Children with accompanying disabilities (other than hearing loss, for example, autism or blindness, attention-deficit/hyperactivity disorder, etc.) or their parents refused to do the tests and also, children with mild to moderate or unilateral hearing loss were excluded from the plan. Also, children with mild to moderate or unilateral hearing loss were excluded from the plan.
Therefore, according to this project’s inclusion and exclusion criteria, the study only recruited a small number of samples of both rehabilitated and non-rehabilitated hearing-impaired children.
The Denver development screening test 2 (DDST-II) was employed to measure development assignments in this project. In 1967, Frankenberg et al. designed the Denver test, which underwent revision and standardization in 1990. The test consists of 125 items and is designed to assess children from birth to 6 years of age across 4 aspects: Personal-social development, fine motor development, language development, and gross motor development. The test assesses developmental tasks and skills based on the natural order in which they typically appear in children [18]. The chart provides information on the ages at which 25% to 50%, 50% to 75%, and 75% to 90% of Denver children have completed each task. This study considers the age range in which 50% to 75% of children could perform the task as the norm. The validity and reliability of the DDST-II have been confirmed in Iran [19]. According to the Denver test, children aged 6 to 18 months are assessed for 9 language development skills, while personal-social and language development are evaluated through 11 skills [20]. This project carried out developmental tasks for each child’s age (Table 1).
Demographic data were initially collected for all children at the Central Audiology Clinic of Khorramabad, following all COVID-19 protocols. Then, eligible participants underwent diagnostic hearing assessments, including otoacoustic emissions (OAE), auditory brainstem response (ABR), auditory steady-state response (ASSR), and behavioral audiometry when necessary. The child’s personal-social and developmental language skills were then evaluated using the DDST-II appropriate for their age. OAE was employed as one of the tests in this study. A passing result on this test indicated normal hearing sensitivity, while a failing result prompted referral for further diagnostic hearing evaluations. ABR was the next test. The presence of wave V at an intensity of 25-30 dB confirms normal hearing in the child, whereas the absence of ABR waves at higher intensities results in additional diagnostic tests. Lastly, ASSR was conducted on children referred for ABR testing to confirm the final diagnosis of hearing loss. Behavioral audiometry involves observing the child’s responses to sounds produced by sound makers (a drum for low-frequency sounds and a bell for high-frequency sounds).
A vertical line was drawn on the Denver chart sheet according to the child’s calendar age. The test date was recorded to evaluate language and personal-social development with the DDST-II. Then, all the items in each section (personal-social and developmental language skills), the age line passes through them performed. A “P” would be recorded in the column if the child completed the task, and an “F” if the child did not. Following the examiner’s instructions, the child performed the skill and scored 1 for passing or 0 for failing. In this research, if 50% to 75% of Denver’s typical children could accomplish the task, it was considered the standard for a child’s expected ability (all three groups involved in the study). Data from the Denver assessment were analyzed based on latency, absence of delay, or children’s developmental progress per day (Table 2).
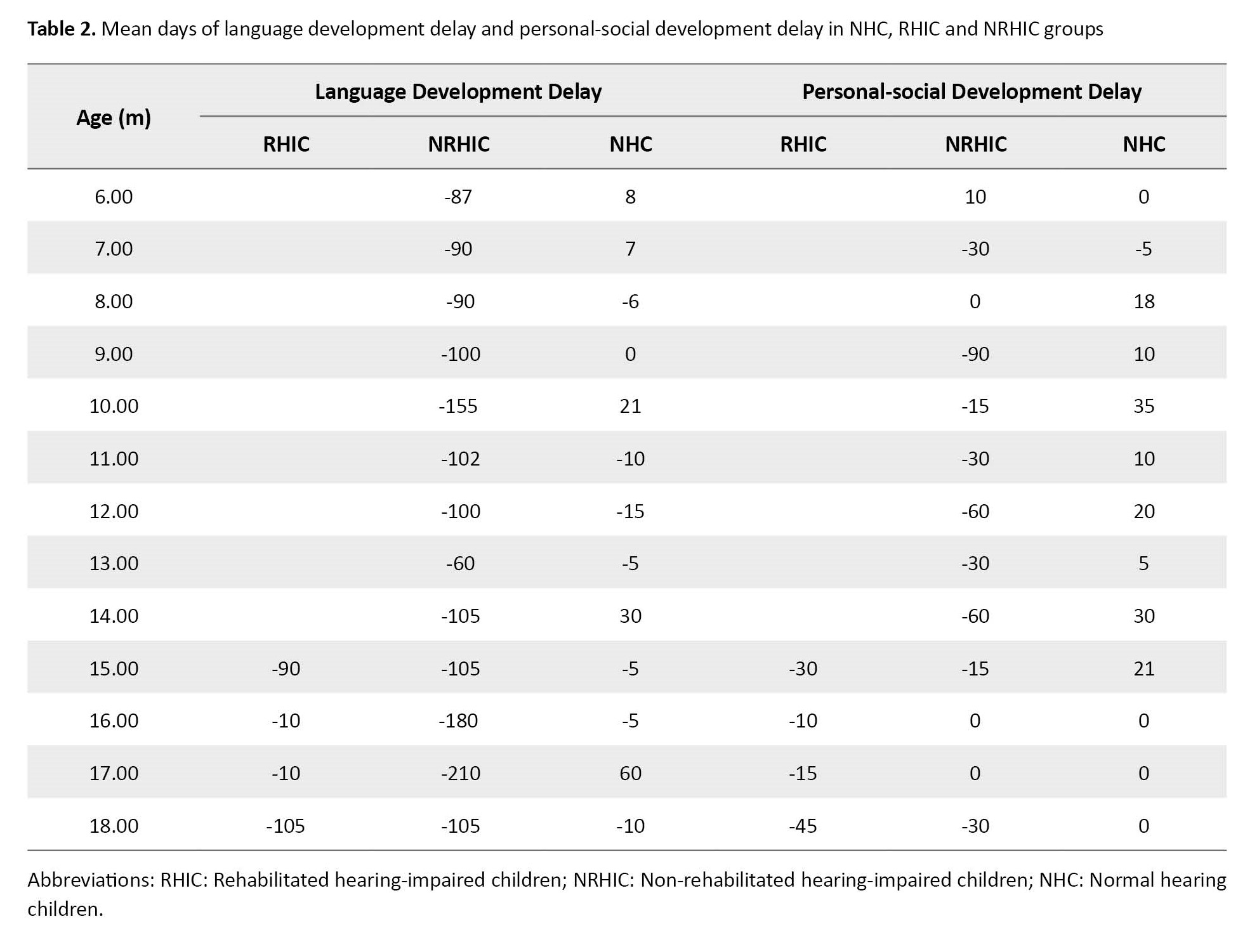
A positive symbol next to the number of days indicates improvement in the chosen developmental aspect compared to the Denver sample. Conversely, a negative symbol suggests a delay in the developmental aspect selected compared to the Denver sample (Figures 1 and 2).
A zero marks that the participant’s development is on par with the Denver sample.
Data analysis was performed based on the number of days of delay or progress of children’s personal-social and language skills development compared to the Denver scale (Table 2). The Kruskal-Wallis and Mann-Whitney non-parametric tests were used to analyze daily developmental data (Table 3).
Results
The results showed a statistically significant difference between language development in the NHC group and hearing-impaired children groups: NRIHC (P=0.001) and RIHC (P=0.016). The development of personal-social skills between the NHC group and RHIC (P=0.004) and NRHIC (P=0.001) was statistically significant. However, the difference in these two developmental aspects, language (P=0.770) and personal social (P=0.0421), between the two hearing-impaired groups was not significant (P≤0.05) (Tables 2 and 4).
Figures 1 and 2 show the participants’ delay, non-delay, or advanced development based on the day’s developmental data. NHC children are above the midline with a positive score, while some have a negative score below the midline. The statistical analysis reveals no significant difference between the language and personal-social development in NHC and Denver samples. Additionally, Figure 1 shows that the language development scores in NRHIC and RHIC groups are constantly below the midline with a negative score. Similarly, in Figure 2, the personal-social development scores in the NRHIC and RHIC groups are below the midline with a negative score.
Discussion
Based on the results of this study, the presence of hearing impairment in early childhood, in other words, in the pre-language stage, delays the development of language and social skills. Therefore, to compensate for this delay, solving the hearing problem and rehabilitating the affected children is necessary. The child should also be treated from the very beginning of childhood and immediately after the diagnosis of hearing loss. The global emphasis on timely hearing problem diagnosis and rehabilitation will be discussed in the following. Then, the causes of delay in rehabilitating the children participating in this study will be examined.
According to the American Hearing and Speech Association (ASHA), hearing-impaired children should undergo hearing rehabilitation following the diagnosis of hearing loss. Language and speech development are affected regardless of the cause of the hearing loss (whether acquired or congenital) [21]. It is recommended that hearing rehabilitation be begun within 6 months, as delayed participation may impact the results [16]. The age of children receiving hearing rehabilitation plays a significant role in the outcomes, affecting emotional, social, linguistic, and speech development [22].
Before implanting or using a hearing aid, children with pre-lingual deafness experience a period of auditory deprivation, limiting their speech access (vocabulary). It is often hypothesized that prolonged periods of auditory deprivation will result in significant delays in vocabulary size [23]. This hypothesis is supported by studies demonstrating a negative relationship between age at implantation and vocabulary size [24-26].
The length of auditory deprivation also appears to affect developmental rates in vocabulary. Studies by Shakrawal et al. (2022) showed that great communication benefits were achieved by early implantation without hearing aid use; the results exemplify the importance of enhanced social environments provided by everyday life experience for human brain development and reassure parents considering cochlear implants where hearing aid and speech training is unavailable [27].
The consensus among cochlear implant (CI) researchers is that receiving a CI after age two is late, whereas receiving a CI before one year is early [28]. There is a strong connection between language and motor systems, so young children can discover new objects and practice language through acquiring motor skills [29].
On the other hand, deaf children have delayed fine and gross motor development [30]. Thus, delays in language development can be related to delays in motor development.
In Khoramabad (project area), despite increasing knowledge about the importance of early intervention and rehabilitation in hearing care, many children have arrived too late to receive a hearing aid and begin a hearing rehabilitation program. We found that out of the 29 deaf children, 19 were diagnosed with hearing problems before 3 months, 8 between 3 and 6 months, and only one after 6 months. This finding highlights the effectiveness of the global hearing screening program. Timely and accurate assessment after diagnosis can prevent hearing loss from becoming a disability in the future for hearing-impaired children. However, only 5 children had access to rehabilitation services. Delays and deficiencies in hearing rehabilitation services impair the success of neonatal hearing screening programs. Among the 29 deaf children, 8 had a family member who was deaf (first or second degree), and 21 came from families without prior experience with hearing impairment, often leading to resistance in accepting their child’s hearing loss. This resistance can result in missed opportunities for timely treatment and rehabilitation for the child.
Finally, it is essential to underline that auditory training falls under hearing rehabilitation. However, the excessive focus of the rehabilitation team on this aspect has resulted in the neglect of other crucial components of auditory rehabilitation, such as motor development and personal-social skills.
Numerous studies have addressed the deficiencies in social skills among individuals with hearing impairments. These studies have highlighted the significance of education, acquisition, and application of social skills and their promotion [31]. Regrettably, the level of education among parents in all three participant groups was moderate, with a few having postgraduate education. Furthermore, concerning employment, the majority had unstable jobs, such as manual labor, gardening, painting, and seasonal work. These findings reflect the unfavorable economic conditions of households in the city under investigation. The rising costs of hearing aids, treatment, and rehabilitation classes may contribute to the limited number of children undergoing rehabilitation. Economic sanctions in Iran have increased expenses for hearing aids and cochlear implants. The COVID-19 pandemic has further exacerbated the situation by reducing resources available for children, as hearing training centers have closed, leaving only online education. The global neonatal hearing screening program advocates for prompt evaluation and intervention within the first few months after birth following a diagnosis of hearing loss for effective hearing rehabilitation.
Conclusion
Delays in language and social skills development are evident in hearing-impaired children at an early age, so rehabilitation should start early in childhood. Health is a complex and comprehensive system that requires an interdisciplinary approach to address its multiple determinants. In rehabilitating deaf children, attention should be paid to all aspects of development, which requires the cooperation of specialists in different treatment fields. Also, the Denver-II screening test is recommended to assess language and skills development in health centers and centers specialized for hearing-impaired children aged 6 to 18 months.
Study limitations
Due to the spread of COVID-19, families were unwilling to go to the center for hearing and developmental assessment tests, especially the parents of deaf children. On the other hand, children who were identified as having severe to profound hearing loss used online services due to the COVID-19 pandemic and the suspension of hearing training centers. However, the online programs were not as effective as face-to-face meetings. Therefore, very few children benefited from appropriate hearing training and the conditions for participating in the study.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Islamic Azad Unversity, Boroujerd Branch (Code: IR.IAU.B.REC.1400.007).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and supervision: Parvin Veisarami and Mehdi Roozbahai; Methodology: Parvin Veiskarami and Ideh Mortazavi; Funding acquisition and resources: Parvin Veiskarami, Mehdi Roozbahai and Ideh Mortazavi; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank the neonatal hearing screening program officials in the Welfare Organization of Lorestan Province for their cooperation in achieving the desired statistical population despite the limitations caused by the COVID-19 epidemic.
References
- Lipkin PH, Macias MM, Norwood KW, Brei TJ, Davidson LF, Davis BE, et al. Promoting optimal development: Identifying infants and young children with developmental disorders through developmental surveillance and screening. Pediatrics. 2020; 145(1):e20193449. [Link]
- Hirai AH, Kogan MD, Kandasamy V, Reuland C, Bethell C. Prevalence and variation of developmental screening and surveillance in early childhood. The Journal of the American Medical Association (JAMA) Pediatr. 2018; 172(9):857-66. [DOI:10.1001/jamapediatrics.2018.1524] [PMID] [PMCID]
- Canadian Task Force on Preventive Health Care. Recommendations on screening for developmental delay. Canadian Medical Association Journal (CMAJ). 2016; 188(8):579-87. [DOI:10.1503/cmaj.151437] [PMID] [PMCID]
- Shafinia P, Jahadiyan Sarvestani H. [Normalization of gross and fine movements of Denver II test in children 6-3 in Ahvaz-Iran (Persian)]. Scientific-Research Journal (ISC Ministry of Science). (2011); 14(9):83-96. [Link]
- Payne VG, Isaacs LD. Human motor development: A lifespan approach. New York: Routledge; 2017. [DOI:10.4324/9781315213040]
- Veiskarami P, Roozbahani M. Motor development in deaf children based on Gal-lahue’s model: A review study. Auditory and Vestibular Research. 2020; 29(1):10-25. [DOI:10.18502/avr.v29i1.2364]
- Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL, et al. Spoken language development in children following cochlear implantation. JAMA. 2010; 303(15):1498-506. [DOI:10.1001/jama.2010.451] [PMID] [PMCID]
- Vahab M, Shahim S, Avardiyani MM, Jafari S, Faham M. [The relationship between the development of expressive language and social skills in Persian children aged 4 to 6 years (Persian)]. Journal of Audiology. 2012; 21(4):28-36. [Link]
- Shaari Nejad AA. [Developmental psychology(Persian)]. Tehran: ETELAAT Publishing; 2009. [Link]
- Aly Z, Taj F, Ibrahim S. Missed opportunities in surveillance and screening systems to detect developmental delay: A developing country perspective. Brain and Development. 2010; 32 (2): 90-7. [DOI:10.1016/j.braindev.2009.06.004] [PMID]
- Council on Children With Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee; Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics. 2006; 118(1):405-20. [DOI:10.1542/peds.2006-1231] [PMID]
- Li Y, Zhang W, Yang Y, Liu B, Chen M, Liu W, et al. Comprehensive developments in deaf children aged 6 months to 6 years. Research square. 2020. [Link]
- De Kegel A, Maes L, Van Waelvelde H, Dhooge I. Examining the impact of cochlear implantation on the early gross motor development of children with a hearing loss. Ear and Hearing. 2015; 36(3):e113-21. [DOI:10.1097/AUD.0000000000000133] [PMID]
- Stevenson J, McCann D, Watkin P, Worsfold S, Kennedy C; Hearing Outcomes Study Team. The relationship between language development and behaviour problems in children with hearing loss. Journal of Child Psychology and Psychiatry, and Allied Disciplines,. 2010; 51(1):77-83. [DOI:10.1111/j.1469-7610.2009.02124.x] [PMID]
- Reid AM, Bolshakova MI, Guzick AG, Fernandez AG, Striley CW, Geffken GR, et al. Common barriers to the dissemination of exposure therapy for youth with anxiety disorders. Community Mental Health Journal. 2017; 53(4):432-7. [DOI:10.1007/s10597-017-0108-9] [PMID]
- Denmark T, Marshall J, Mummery C, Roy P, Woll B, Atkinson J. Detecting Memory Impairment in Deaf People: A New Test of Verbal Learning and Memory in British Sign Language. Archives of Clinical Neuropsychology. 2016; 31(8):855-67. [DOI:10.1093/arclin/acw032] [PMID] [PMCID]
- Haddadi Aval M, Abdollahi F, Jafarzadeh S. Auditory rehabilitation based on auditory verbal therapy approach on children with bilateral sensory-neural hearing loss. Auditory and Vestibular Research. 2020; 29(3):172-7. [DOI:10.18502/avr.v29i3.3850]
- Zhang X, Norton J, Carrière I, Ritchie K, Chaudieu I, Ancelin ML. Risk factors for late-onset generalized anxiety disorder: Results from a 12-year prospective cohort (The ESPRIT study). Translational Psychiatry. 2015; 5(3):e536. [DOI:10.1038/tp.2015.31] [PMID] [PMCID]
- Frankenburg WK, Dodds J, Archer P, Shapiro H, Bresnick B. The Denver II: A major revision and restandardization of the Denver Developmental Screening Test. Pediatrics. 1992; 89(1):91-7. [DOI:10.1542/peds.89.1.91] [PMID]
- Shahshahani S, Vameghi R, Azari N, Sajedi F, Kazemnejad A. [Has Denver Developmental Screening Test-II appropriate validity and reliability for screening of developmental disorders in 0-6 years old children in Tehran city (Persian)]? Payesh 2011; 10 (4):469-75. [Link]
- Abessa TG, Worku BN, Kibebew MW, Valy J, Lemmens J, Thijs H, et al. Adaptation and standardization of a Western tool for assessing child development in non-Western low-income context. BMC Public Health. 2016; 16:652. [PMID] [PMCID]
- Dieleman E, Percy-Smith L, Caye-Thomasen P. Language outcome in children with congenital hearing impairment: The influence of etiology. International Journal of Pediatric Otorhinolaryngology. 2019; 117:37-44. [DOI:10.1016/j.ijporl.2018.11.002] [PMID]
- Yang Y, Liu YH, Fu MF, Li CL, Wang LY, Wang Q, et al. Home-based early intervention on auditory and speech development in Mandarin-speaking deaf infants and toddlers with chronological aged 7-24 months. Chinese Medical Journal. 2015; 128(16):2202-7. [DOI:10.4103/0366-6999.162504] [PMID] [PMCID]
- Walker EA, McGregor KK. Word learning processes in children with cochlear implants. Journal of Speech, Language, and Hearing Research. 2013; 56(2):375-87. [PMID]
- Naik AN, Varadarajan VV, Malhotra PS. Early pediatric Cochlear implantation: An update. Laryngoscope Investigative Otolaryngology. 2021; 6(3):512-21. [DOI:10.1002/lio2.574] [PMID] [PMCID]
- Lund E. Vocabulary knowledge of children with cochlear implants: A meta-analysis. Journal of Deaf Studies and Deaf Education. 2016; 21(2):107-21. [DOI:10.1093/deafed/env060] [PMID] [PMCID]
- James D, Rajput K, Brinton J, Goswami U. Phonological awareness, vocabulary, and word reading in children who use cochlear implants: does age of implantation explain individual variability in performance outcomes and growth? Journal of Deaf Studies and Deaf Education. 2008; 13(1):117-37. [DOI:10.1093/deafed/enm042] [PMID]
- Shakrawal N, Sonkhya N, Agarwal S, Grover M. The effect of age at cochlear implantation on speech and auditory performances in prelingually deaf children. Indian Journal of Otolaryngology and Head And Neck Surgery. 2022; 74(Suppl 1):52-61. [DOI:10.1007/s12070-020-01821-0] [PMID] [PMCID]
- Ruben RJ. Language development in the pediatric cochlear implant patient. Laryngoscope Investigative Otolaryngology. 2018; 3(3):209-13. [DOI:10.1002/lio2.156] [PMID] [PMCID]
- Ertugrul G, Aslan F, Sennaroglu G, Sennaroglu L. Children with auditory brainstem implant: How do they perform in motor and language skills? Audiology & Neuro-Otology. 2021; 26(3):173-81.[DOI:10.1159/000510584] [PMID]
- Veiskarami, P, Roozbahani, M, Saedi, S, Ghadampour E. Comparing fine and gross motor development in normal hearing children, rehabilitated, and non-rehabilitated hearing-impaired children. Auditory and Vestibular Research. 2022; 31(3):208-17. [DOI:10.18502/avr.v31i3.9871]
Type of Study: Original Article |
Subject:
Pediatrics
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |