Volume 12, Issue 4 (Autumn 2024)
Iran J Health Sci 2024, 12(4): 305-316 |
Back to browse issues page
Ethics code: NA
Clinical trials code: NA
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Joseph J, Varghese B. Impact of Annual Appraisal Processes on Nurses’ Job Performance and Satisfaction: A Systematic Review. Iran J Health Sci 2024; 12 (4) :305-316
URL: http://jhs.mazums.ac.ir/article-1-955-en.html
URL: http://jhs.mazums.ac.ir/article-1-955-en.html
Department of Nursing Education, Medical and Surgical In-patient Services, Al-Khor Hospital, Hamad Medical Corporation, Doha, Qatar. , Jennyvia.84@gmail.com
Keywords: Nursing performance, Performance appraisal (PA), Job satisfaction, Professional development, Feedback quality
Full-Text [PDF 920 kb]
(2683 Downloads)
| Abstract (HTML) (3733 Views)
Full-Text: (1606 Views)
Introduction
Performance appraisal (PA) is a fundamental practice within organizations that evaluates employees’ job performance against predetermined criteria and objectives. This structured process provides organizations with a means to deliver feedback, identify strengths and areas for improvement, and align individual contributions with broader organizational goals. In healthcare, particularly nursing, effective PAs are critical due to their direct impact on patient outcomes and service quality [1].
As the workforce landscape continues to evolve, research into the dynamics of annual PAs has shed light on their multifaceted implications for individuals and the broader organizational context [2]. Annual PAs are not just tools for evaluation but are integral to fostering a sense of purpose and direction among employees, particularly in high-stake environments like healthcare [3]. Scholars have traced the evolution of PA and management practices, reflecting on over a century of progress [4]. Despite this evolution, challenges remain in ensuring that appraisal systems are effective, fair, and transparent across diverse healthcare settings.
The concept of PA s, especially within the nursing profession, has garnered significant attention in recent years. However, the literature reveals inconsistencies in the application and effectiveness of these appraisal systems across different contexts [5, 6]. While some studies demonstrate that PAs can significantly enhance job performance and organizational commitment among nurses, the impact of these appraisals varies widely depending on how they are implemented [7].
For instance, research shows that the active participation of nurses in the appraisal process, coupled with constructive feedback, can enhance their job performance and commitment to the organization [8]. Similarly, feedback provided through peer review programs has been shown to positively influence nurses’ perceptions, attitudes, and performance [9]. Aligning individual performance with organizational goals through PA systems remains a key challenge, particularly when disparities exist between individual objectives and broader organizational priorities [10]. This gap suggests a need for a more systematic understanding of how appraisal processes can be optimized to improve outcomes consistently.
While the importance of conducting annual appraisals and continuous performance reviews is widely acknowledged, the impact of these practices on staff development and motivation in nursing remains insufficiently examined [11]. Studies indicate that nurses’ job satisfaction and commitment can be significantly improved when they perceive the PA system as both fair and transparent [12]. Appraisal interviews have been shown to significantly improve nurses' performance by facilitating focused discussions and offering constructive feedback, supporting professional growth and skill enhancement [13].
Preparing for annual staff appraisals provides clarity on expectations and actionable feedback, fostering continuous professional development and improved performance [14]. Feedback mechanisms that are well-integrated into the appraisal process can facilitate open communication between supervisors and employees, ultimately guiding professional development [15]. This situation is particularly important in nursing, where continuous professional growth is essential to maintaining high standards of patient care.
Research indicates that nurses who receive regular, constructive feedback are more likely to be engaged and committed to their work [16]. Such feedback acknowledges employees’ efforts, recognizes their achievements and helps align their goals with organizational objectives [17]. Despite the recognized importance of feedback, its role in influencing job performance, job satisfaction, and overall engagement remains inconsistently addressed in the literature. This inconsistency underscores the need for a more detailed exploration of feedback’s role within appraisal systems.
The principles of fairness and transparency are critical to the success of PAs. Nurses’ perceptions of these factors significantly influence their job satisfaction, motivation, and commitment [18]. When appraisal processes are perceived as fair, they build trust within the organization and promote a culture of accountability [19]. Conversely, perceived unfairness can lead to frustration, demotivation, and potential burnout, which are significant concerns in the high-pressure setting of healthcare [20].
Studies have shown that transparent communication of evaluation criteria, processes, and outcomes is essential for reducing ambiguity and enhancing trust in the appraisal system [21]. Transparent communication allows employees to clearly understand how their performance is evaluated and what is expected of them, fostering alignment with organizational objectives and enhancing work engagement [22]. Furthermore, equitable appraisal systems that assess nurses’ contributions without bias foster a sense of justice within the workforce, increasing job satisfaction and commitment [7].
Despite the wealth of research on PAs, a significant gap exists in understanding how these appraisals can be consistently effective across different healthcare settings. Variability in the implementation of appraisal systems, coupled with employees' perceptions of fairness, significantly impacts their engagement and satisfaction, emphasizing the need for a deeper exploration of these dynamics within performance evaluations [23]. This study aims to fill this gap by conducting a systematic review of cross-sectional studies to identify the effects of annual appraisal processes on nurses’ job performance. By focusing on the role of constructive feedback, fairness, and transparency, this research seeks to provide evidence-based insights that can provide information for developing more effective appraisal systems tailored to the unique needs of the nursing profession.
This systematic review seeks to investigate the impact of annual appraisal processes on nurses’ job performance, mainly focusing on the effects of constructive feedback, the perceived fairness of the process, and the transparency of evaluation criteria. The study aims to comprehensively understand how these factors influence job satisfaction, motivation, and overall performance in diverse healthcare settings.
The findings of this review can shape nursing practice, management, and policy concerning PAs. By systematically understanding how annual appraisal processes impact nurses’ job performance, nursing management could aim their strategies at improving job satisfaction and patient care outcomes. Furthermore, the insights gained from this review may guide the development of more standardized and effective appraisal systems that are equitable, transparent, and conducive to professional growth in nursing.
Aim
The primary aim of this systematic review was to aluate the impact of annual appraisal processes on nurses’ job performance and satisfaction. Specifically, this review focuses on understanding how constructive feedback, fairness, and transparency within appraisal systems influence these outcomes. The other specific objective was to synthesize evidence and identify trends, gaps, and implications for nursing practice and policy.
Materials and Methods
This systematic review followed the Joanna Briggs Institute (JBI) methodology for prevalence systematic reviews [24] and the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [25]. As the protocol was not eligible for inclusion in PROSPERO, it was not numbered.
Search strategy
The initial step in the methodology involved developing a comprehensive search strategy to identify studies relevant to the research aims. A combination of relevant keywords and MeSH (medical subject headings) terms was utilized. Although it was primarily designed for PubMed, it is also adaptable to other databases. The search was conducted across several prominent databases, including PubMed, CINAHL, Cochrane Library, Scopus, PsycINFO, and ScienceDirect. The rationale for selecting these databases is based on their extensive health and medical literature coverage, ensuring a broad and inclusive search of peer-reviewed articles and relevant evidence-based resources.
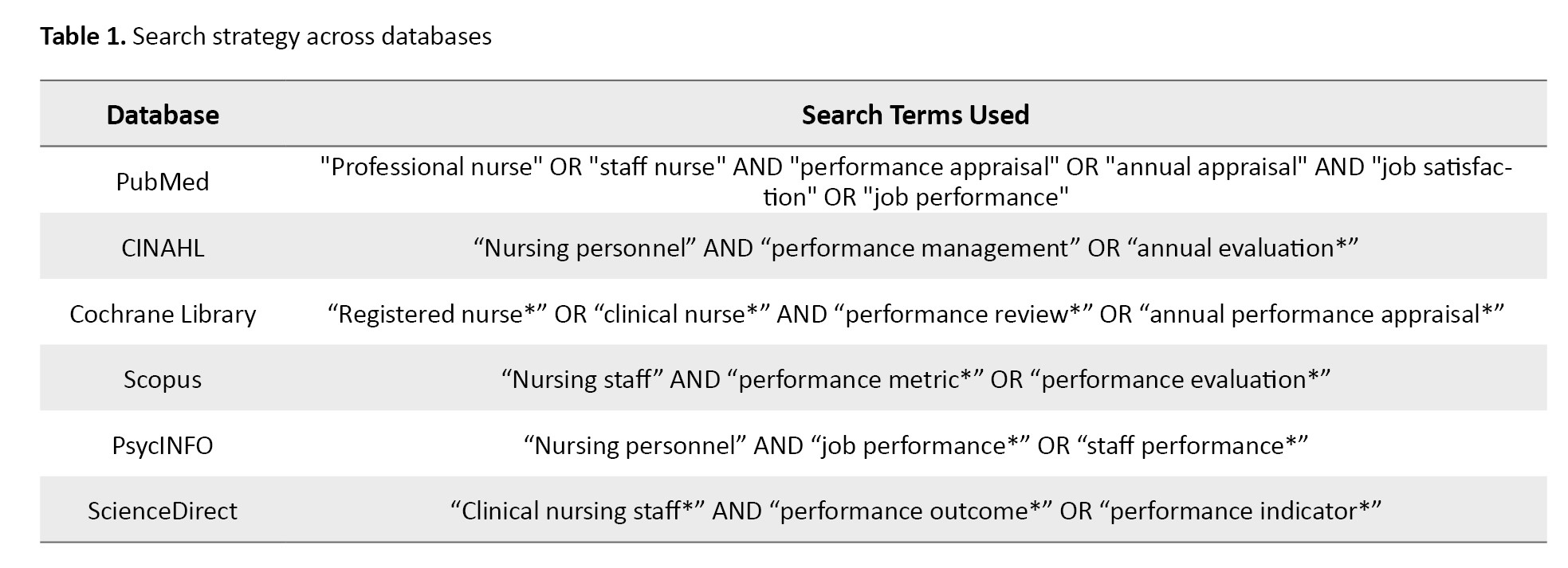
The search strategy was tailored for each database to maximize the retrieval of pertinent studies. For example, in PubMed, the search included MeSH terms such as “professional nurse" or "staff nurse", "performance appraisal" or "annual appraisal" and "job satisfaction" or "job performance" combined using boolean operators. The specific search terms and strategies used for each database are outlined in Table 1.
The search was conducted for studies published in English between 2012 and 2022. The justification for this time frame is to capture recent developments and current practices in PA systems, reflecting changes and advancements in nursing and healthcare environments over the past decade.
Inclusion and exclusion criteria
Inclusion criteria were established to ensure the selection of relevant and meaningful studies.
Studies were included if they
● Involved nurses working in diverse healthcare settings,
● Focused on the impact of annual appraisal processes on job performance and job satisfaction,
● Were published in English between 2012 and 2022, and
● Employed a cross-sectional study design.
Exclusion criteria ruled out studies that were
● Randomized controlled trials, case-control studies, cohort studies, qualitative studies, and mixed-methods studies,
● Published outside the specified time frame, or
● Not directly addressing the impact of annual appraisal processes on nurses’ job performance.
Study selection
The study selection process involved multiple stages to ensure thorough screening and inclusion of relevant studies. First, all identified records underwent a duplicate removal process using EndNote reference management software. Following this, titles and abstracts were screened against the predefined inclusion and exclusion criteria. Any uncertainties or ambiguous cases were advanced to full-text screening for a more detailed evaluation. This methodical approach minimized bias and errors in the selection process, ensuring the inclusion of studies most pertinent to the research objectives.
Quality assessment
The quality of the selected studies was rigorously assessed using the JBI (Joanna Briggs Institute) critical appraisal checklist for analytical cross-sectional studies. This tool evaluates various aspects of study quality, including the clarity of study aims, appropriateness of the sample size and population, reliability of the data collection methods, and validity of the results and conclusions. Discrepancies in quality assessment were resolved through consultation with the supervisor, ensuring consistency and reliability in the evaluation process. Specific criteria such as the method of participant recruitment, measurement of variables, and control for confounding factors were considered in the assessment.
Data extraction
Data were extracted meticulously using a standardized form to capture all relevant information from each study. Key data points extracted included author details, publication year, study design, sample characteristics, specifics of the appraisal process, and principal findings related to job performance and satisfaction. The extraction process also considered contextual factors such as healthcare setting and geographical location, which could influence the outcomes. The extracted data provided the foundation for a comprehensive analysis of the appraisal processes and their impacts.
Data analysis
The data analysis employed a narrative synthesis approach, integrating descriptive and thematic analysis to examine the influence of annual appraisal processes on nurses’ job performance and satisfaction. This approach facilitated the identification of common themes such as feedback mechanisms, transparency, and fairness, which are critical in appraisal systems. Focusing on these key components, the analysis highlighted how constructive feedback can enhance job performance and professional growth, while transparency and fairness are linked to higher job satisfaction and organizational commitment among nurses. The synthesis also accounted for each study’s methodological quality and context, comprehensively understanding the evidence across diverse healthcare settings [8, 5].
Results
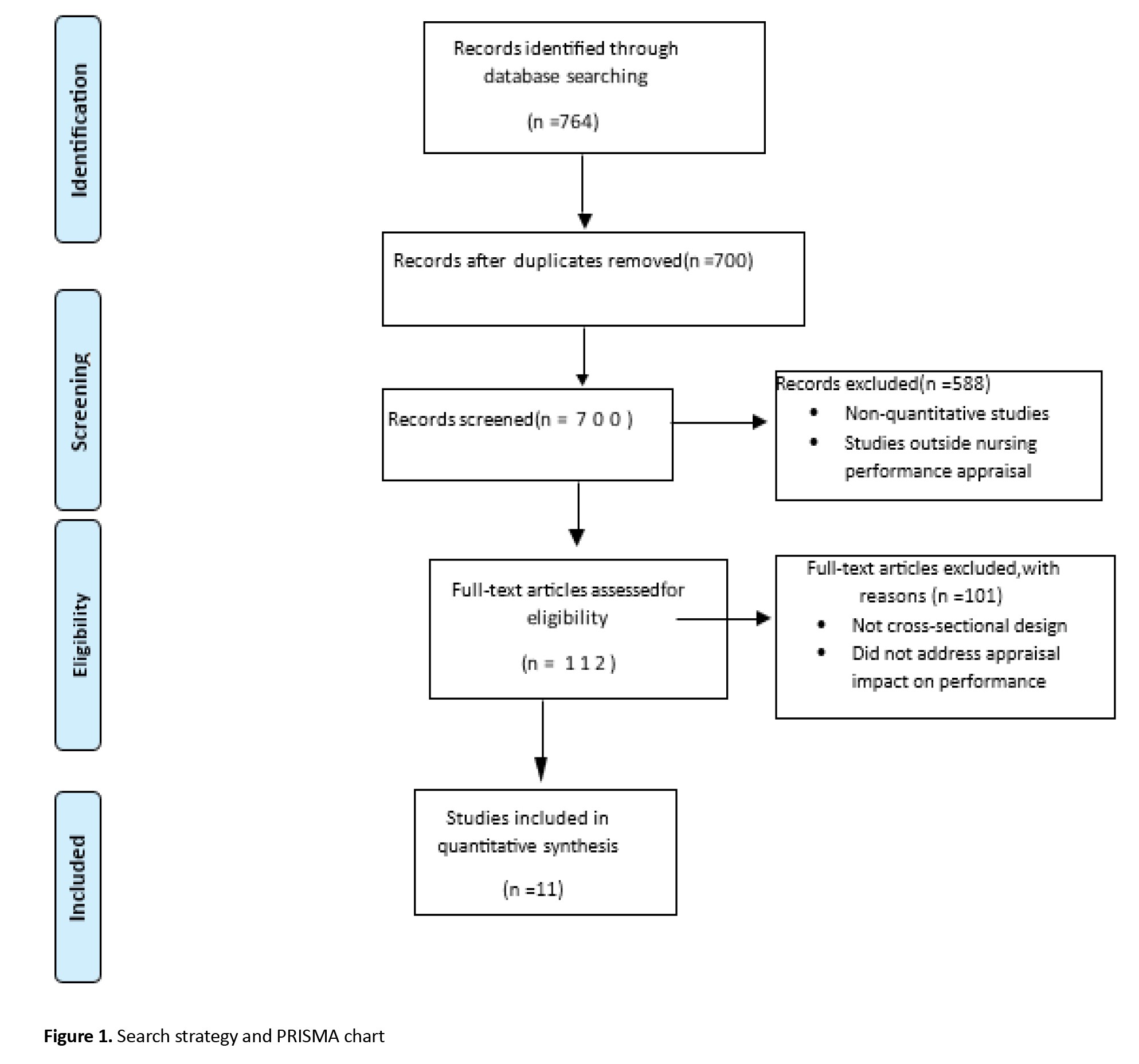
This systematic review followed the PRISMA (preferred reporting items for systematic reviews and meta-analyses) 2009 guidelines for systematic reviews [8], specifically using the PRISMA flow diagram to outline the study selection process. The initial search across six major databases yielded 764 records. After removing 64 duplicates, 700 records remained for screening. The titles and abstracts of these records were reviewed, excluding 588 articles that were primarily non-quantitative studies or did not focus on nursing PA . Subsequently, 112 full-text articles were assessed for eligibility. Of these, 101 articles were excluded for reasons such as not employing a cross-sectional study design or not directly addressing the impact of annual appraisal processes on nurses’ job performance. This process led to the inclusion of 11 cross-sectional studies in the qualitative synthesis, each providing valuable insights into the role of PAs in healthcare, particularly for nursing professionals (Figure 1). The synthesis of findings focused on several key themes that emerged from the studies: Constructive feedback, transparency and fairness, and professional development. These themes were identified based on the studies’ most frequently discussed appraisal processes and their reported impact on nurses’ job performance and satisfaction.
Constructive feedback
Many studies emphasized the importance of constructive feedback in PAs. It was found that feedback, when delivered in a supportive and actionable manner, helped nurses identify areas for improvement, boosted their confidence, and encouraged continuous professional growth. This theme aligns with literature that identifies feedback as a vital component in performance enhancement, as it guides improvement and reinforces positive behaviors within healthcare settings.
Transparency and fairness
Several studies linked transparency and fairness in the appraisal process to higher job satisfaction and organizational commitment among nurses. Transparency in evaluation criteria and fairness in the assessment process were associated with greater trust in leadership and reduced turnover intentions. This theme underscores the need for organizations to implement fair and transparent appraisal processes to build trust and motivate nurses to perform at their best.
Professional development
The studies highlighted that well-structured appraisal processes fostered professional development by encouraging goal-setting, skills assessment, and career planning. PAs that incorporated professional development goals enhanced nurses’ engagement with their work and supported long-term career growth. This theme emphasizes the potential of appraisal systems to go beyond evaluation and actively contribute to the professional development of nursing staff.
By analyzing these themes, the synthesis reveals that effective appraisal processes in nursing are not solely about performance measurement but are also integral to creating a supportive environment for career growth and job satisfaction. The findings suggest that healthcare institutions should prioritize designing and implementing appraisal systems that incorporate constructive feedback, maintain transparency and fairness, and support professional development. Such appraisal systems can enhance job performance and contribute to positive organizational outcomes in healthcare settings.
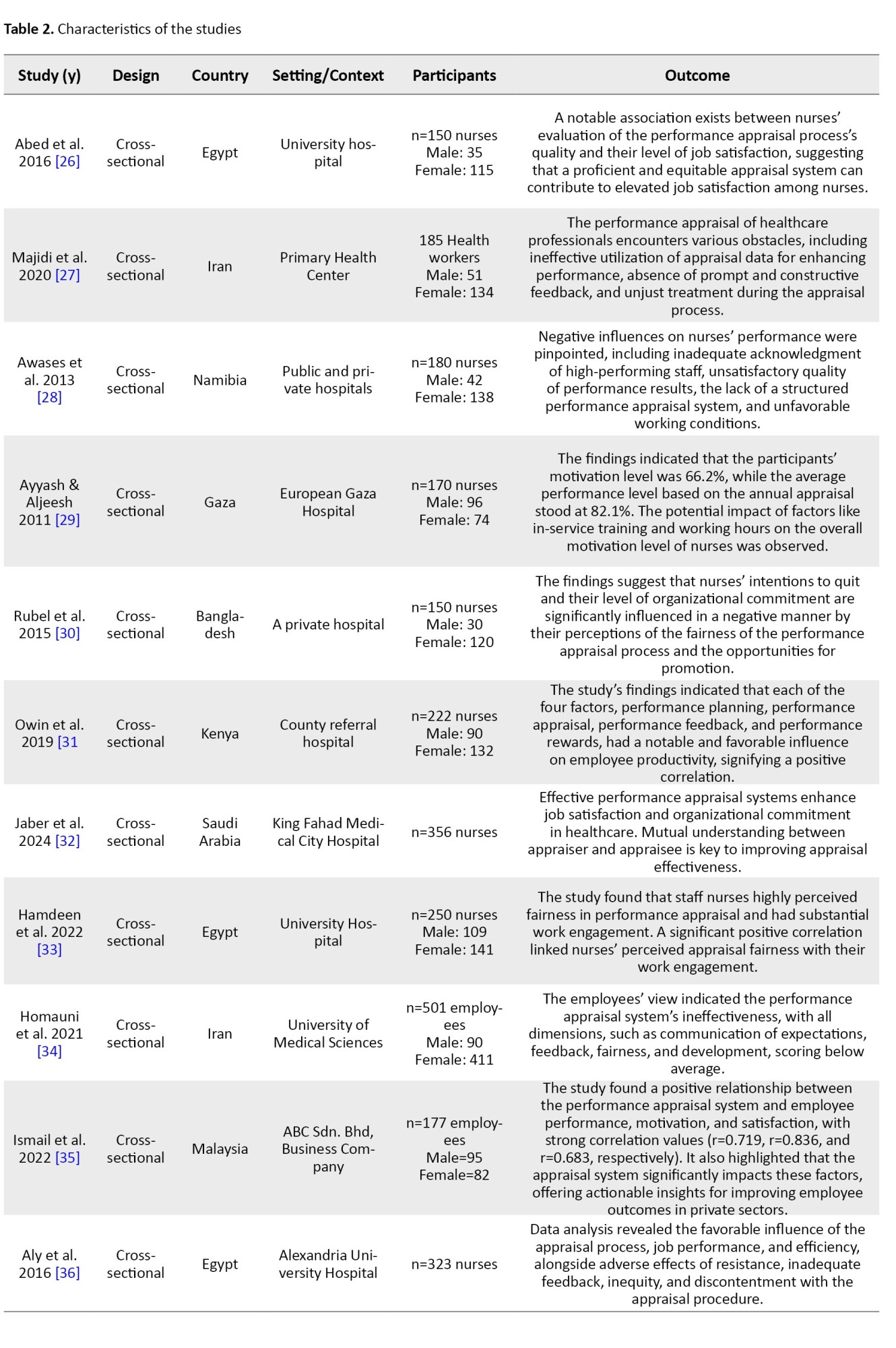
Characteristics of included studies
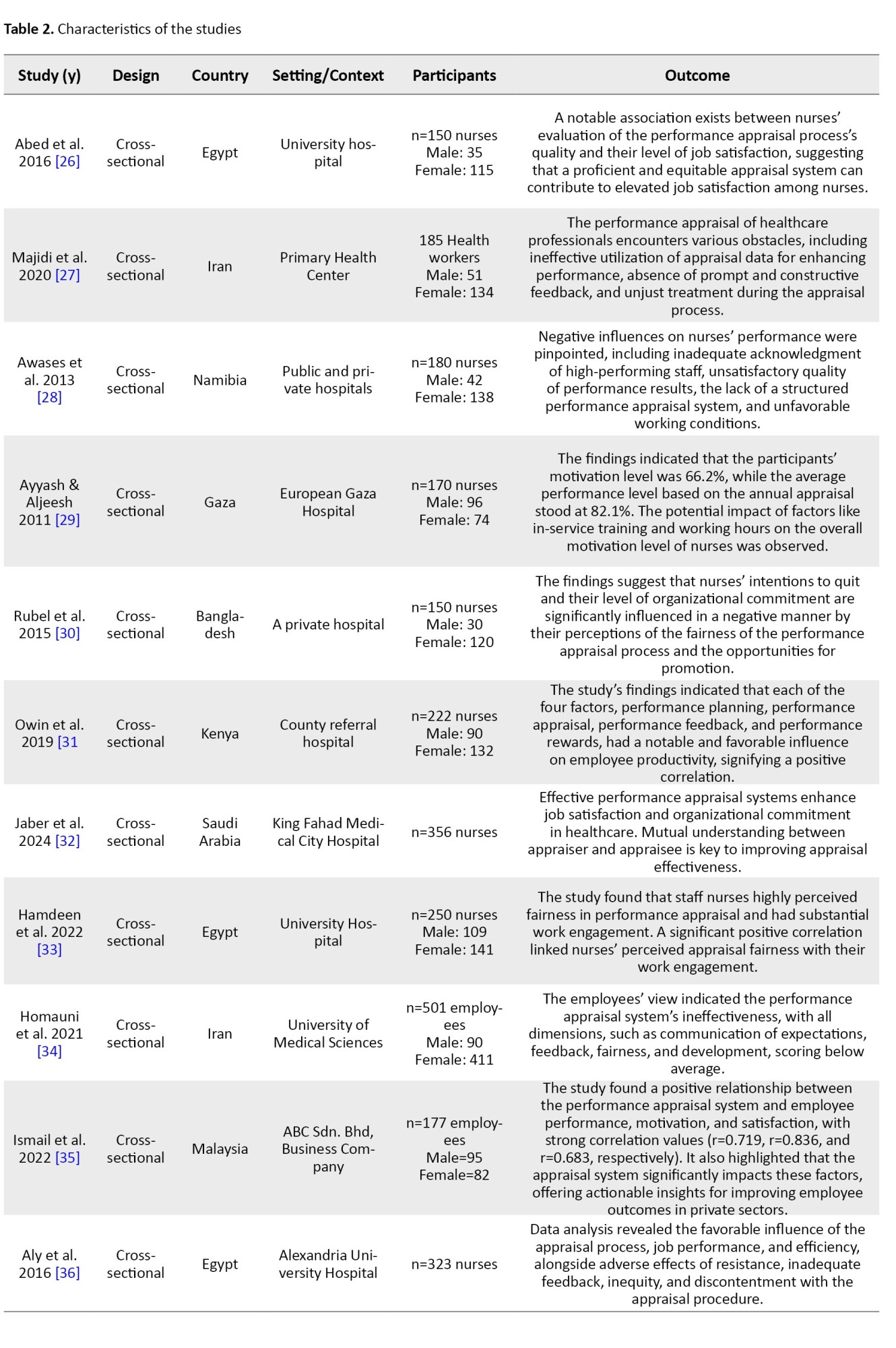
The findings from the included studies offer a detailed perspective on how PA systems influence nurses' job performance, satisfaction, and organizational commitment across healthcare settings.
The quality of appraisal processes emerged as a key factor in enhancing job satisfaction, as evidenced by a study that found fairness in appraisals fosters a more positive work environment and stronger organizational commitment [26]. Perspectives from healthcare professionals emphasized the need for tailored appraisals that align with the specific demands of healthcare roles, enhancing their effectiveness and relevance [27].
A lack of structured and fair appraisal systems was noted to negatively impact nurses’ motivation and performance, underscoring the importance of standardizing appraisal criteria to achieve better outcomes [28]. Structured appraisal systems, when implemented effectively, significantly boosted employee productivity and motivation, particularly through the integration of performance planning and reward mechanisms [29]. However, perceptions of inequity and limited career advancement opportunities within appraisal systems were associated with increased turnover intentions and diminished organizational commitment, revealing critical gaps in existing frameworks [29].
In some instances, appraisal systems were deemed ineffective due to poor communication of expectations, insufficient feedback, and inadequate developmental support, creating challenges for healthcare organizations striving to retain and motivate staff [31]. Transparent appraisal practices, on the other hand, have been shown to foster trust among nursing staff, enhancing engagement and satisfaction while creating a culture of accountability and fairness [32]. Fairness within appraisal systems has also been strongly correlated with higher levels of work engagement, highlighting the critical role of equitable processes in promoting satisfaction and retention among nurses [33].
Appraisal systems tailored to specific organizational contexts demonstrated greater effectiveness, as they addressed unique institutional challenges and priorities, thereby enhancing both individual and organizational outcomes [34]. Comprehensive appraisal systems also showed a significant impact on employee satisfaction, motivation, and performance, reinforcing their value in creating a supportive and productive work environment [35]. Finally, the inclusion of structured components, such as performance planning and clear reward mechanisms, has been pivotal in fostering workplace motivation and boosting productivity among nursing staff [36].
The findings from these studies present a nuanced understanding of PA systems in healthcare. While appraisals can improve job satisfaction, commitment, and performance through fairness, transparency, and constructive feedback, their absence or ineffective implementation can lead to dissatisfaction, reduced engagement, and higher turnover intentions. These results highlight the importance of refining appraisal processes to ensure equity, transparency, and a focus on professional growth (Table 2).
Discussion
This study aimed to review the studies that comprehensively evaluated the role of PA systems in influencing nurses' job performance, satisfaction, and organizational commitment across diverse healthcare settings. The findings revealed the critical importance of constructive feedback, fairness, transparency, and tailored appraisal processes in enhancing nursing outcomes.
A well-structured PA system can significantly boost nurses' job satisfaction and commitment. For example, the perceived quality of PA processes was found to be positively correlated with job satisfaction, underscoring the need for equitable and effective appraisal systems in healthcare institutions [26]. Similarly, structured appraisal systems with clearly defined performance criteria and fair assessment methods were observed to foster higher levels of motivation and commitment among nursing staff [27]. However, ineffective or poorly designed appraisal systems, such as those lacking standardized criteria, can lead to subjective evaluations that negatively affect nurses' engagement and productivity [28].
Feedback mechanisms emerged as a cornerstone of effective PA systems. Regular and meaningful feedback was highlighted as pivotal in motivating nurses and enhancing their professional development [29]. Constructive feedback not only helps nurses identify areas for improvement but also aligns their efforts with organizational goals, ultimately improving work outcomes [30]. Conversely, inadequate or poorly communicated feedback was identified as a barrier to the effectiveness of PA systems, leading to dissatisfaction and diminished trust among staff [31]. Transparent and equitable appraisal practices were shown to build trust within organizations, fostering engagement and job satisfaction [32].
Fairness in appraisal systems plays a crucial role in promoting positive work environments. Studies revealed that perceptions of fairness within the appraisal process were directly linked to higher work engagement and organizational commitment among nurses [33]. Additionally, appraisal systems that consider cultural and institutional dynamics were found to be more effective in meeting the diverse needs of healthcare professionals, further highlighting the importance of tailoring appraisals to specific contexts [34].
Effective communication emerged as another critical element in ensuring the success of PA systems. Clear communication of appraisal expectations and outcomes gives nurses a sense of purpose and direction, enhancing their satisfaction with the appraisal process [35]. Transparent communication also ensures alignment between individual performance and organizational objectives, strengthening staff engagement and productivity [36].
The broader impact of well-implemented PA systems extends beyond individual performance to improve organizational outcomes. Structured components, such as performance planning and reward systems, were found to significantly enhance employee productivity and motivation, ultimately benefiting overall hospital performance [37]. Furthermore, appraisal systems that integrate fairness and transparency were shown to reduce turnover intentions and improve organizational commitment among nurses [38].
Cultural and institutional considerations were identified as vital in shaping the effectiveness of PA systems. Flexible and context-specific appraisal frameworks were found to align more closely with the unique demands of nursing roles, enhancing their relevance and effectiveness [39]. For instance, appraisal systems designed to accommodate the complexities of clinical settings were observed to foster greater staff engagement and satisfaction [40].
Our findings support the evidence suggesting that well-structured appraisal systems can improve healthcare quality and patient outcomes. By prioritizing equity, transparency, and constructive feedback, healthcare institutions can foster a motivated and high-performing nursing workforce [5]. Moreover, appraisal systems tailored to the specific needs of nursing professionals were shown to enhance both individual and organizational outcomes, reinforcing the importance of adaptability in appraisal systems [3].
This systematic review study emphasizes the importance of constructive feedback, transparency, fairness, and effective communication within PA systems. These factors can significantly influence nurses' job performance, satisfaction, and commitment and contribute to organizational efficiency and patient care quality. By addressing these factors, healthcare institutions can refine their appraisal processes, ultimately fostering a more engaged and high-performing nursing workforce [41].
Study limitations
While this systematic review provides valuable insights into the impact of PA systems on nurses’ job performance, several limitations should be considered.
Firstly, the generalizability of the findings is potentiallylimited due to the specific contexts in which the included studies were conducted. Most studies were situated within specific healthcare environments and geographic regions, which may not fully capture the diversity of appraisal practices in nursing globally. As a result, the applicability of the findings may be restricted when attempting to generalize across various healthcare systems, especially in underrepresented or low-resource settings. Prior research highlights similar challenges in systematic reviews, as findings from studies in specific contexts may not always apply to larger populations [41].
Language and publication biases are additional limitations of this review. Only studies published in English
were included, which may have led to language bias and the potential exclusion of relevant studies in other languages.
This limitation could affect the review’s comprehe siveness by overlooking valuable perspectives from non-English-speaking regions. Furthermore, the review may be subject to publication bias, as studies with significant or positive findings are more likely to be published. This tendency may overestimate the effectiveness of PA systems and ultimately skew the conclusions, as highlighted in earlier methodological discussions [42].
Variability in methodological rigor and measurement tools among the selected studies may further impact
the consistency and reliability of the synthesized evidence.
The studies included in this review differed in study design, sample sizes, data collection methods, and measurement tools. For instance, some studies rely on self-report measures of job performance and satisfaction, which may introduce subjective bias and limit the objectivity of the findings. Additionally, methodological variability across the included studies poses challenges to synthesizing robust conclusions. The use of diverse measurement tools and inconsistencies in study quality align with prior findings that such heterogeneity hinders the generation of reliable results [40].
This variability in rigor across studies may compromise
the overall quality and uniformity of the evidence presented.
One of the strengths of this review is its systematic approach, adhering to PRISMA guidelines to ensure transparency and consistency in study selection, data extraction, and analysis. This rigorous approach helps mitigate selection bias and provides a structured foundation for synthesizing findings. However, a major limitation is the reliance on cross-sectional study designs, which inherently limit the ability to draw causal inferences. Crosssectional studies capture data at a single time, making it challenging to assess the long-term effects or causal relationships between appraisal practices and job performance outcomes. As a result, the conclusions drawn are primarily correlational, and caution should be exercised in interpreting these associations as causal. Furthermore, the reliance on cross-sectional designs within the included studies limits the ability to establish causation. This limitation underscores the need for longitudinal studies to validate findings and provide a more comprehensive understanding of the long-term effects of PA systems on nursing outcomes, a need echoed in previous reviews on healthcare performance management [19].
Conclusion
This systematic review aimed to examine the impact of PA processes on nurses’ job performance and job satisfaction, focusing on understanding the role of constructive feedback, transparency, and fairness in appraisal systems. The findings clarify the complex relationship between these appraisal elements and nurses’ motivation, commitment, and job performance. Specifically, constructive feedback emerged as a critical factor in enhancing job performance and satisfaction, reinforcing its role as a mechanism for professional growth and development in nursing.
While the selected articles provide valuable insights, limitations related to study scope, quality, and variability were observed, affecting the consistency of the findings. The review also highlights gaps in understanding the mechanisms through which feedback influences nurse performance, the contextual factors that impact perceptions of fairness, and the long-term effects of appraisal satisfaction on career trajectories. These gaps suggest that while PA positively influences nurse outcomes, a more nuanced and contextual approach is needed to maximize its benefits across diverse healthcare settings.
Despite potential biases, this review employed rigorous methods to enhance the credibility of its findings, contributing to a foundational evidence base for developing effective appraisal systems in nursing. By identifying key themes and areas for improvement, this review offers valuable guidance for healthcare institutions aiming to refine appraisal practices and researchers exploring the evolving healthcare landscape.
Implications for clinical practice
This systematic review underscores the critical role of PA systems in promoting nurses’ job performance, satisfaction, and professional growth. To maximize the effectiveness of appraisals, clinical organizations should prioritize enhancing the quality of feedback provided to nursing staff. Constructive, specific feedback supports skill development and fosters a culture of continuous improvement and engagement. Clinical institutions can enhance feedback quality by investing in communication skills training for appraisers, ensuring that feedback is delivered in a supportive, clear, and constructive manner. This training should emphasize empathy, clarity, and actionable suggestions to support nurses’ professional growth and job satisfaction.
Furthermore, the review suggests that appraisal systems should be tailored to the unique needs of the nursing workforce. This endeavor involves adapting appraisal processes to address nurses’ distinct roles, responsibilities, and challenges in different healthcare settings. Involving nurses in the design and evaluation of appraisal systems can promote a sense of ownership, fairness, and transparency, addressing bias concerns and ensuring that appraisals accurately reflect nurses’ contributions. By creating an inclusive and collaborative appraisal design process, healthcare institutions can build trust and enhance the perceived fairness of the appraisal system.
Additionally, integrating personalized development plans within PAs is recommended to help nurses set meaningful goals, define clear career paths, and identify areas for skill enhancement. Such individualized plans can boost motivation, clarify career trajectories, and align nurses’ growth objectives with organizational goals, ultimately improving job performance and long-term commitment. Personalized development plans encourage nurses to pursue further education, certifications, and skill-building activities, contributing to a more skilled and committed workforce.
The review further advocates for evaluating comprehensive outcomes in PAs, moving beyond traditional metrics to include aspects such as burnout, work-life balance, and interdisciplinary collaboration. Monitoring these outcomes allows healthcare institutions to identify areas where nurses may need additional support, helping to prevent burnout and promote overall well-being. Appraisals considering interdisciplinary collaboration can strengthen team dynamics, improve patient outcomes, and support a holistic approach to healthcare excellence.
Implications for future research
Future research should consider a mixed-methods approach to gain deeper insights into nurses’ perceptions and experiences with the PA process. Combining quantitative and qualitative data can capture both measurable outcomes and the nuanced perspectives of nurses, providing a more comprehensive understanding of the factors that influence appraisal satisfaction and effectiveness.
Another area for exploration is the influence of contextual factors, such as organizational culture, management style, and healthcare setting, on nurses’ perceptions of appraisal fairness and efficacy. Studies investigating how cultural, institutional, and regional differences impact perceptions of fairness could support the development of more tailored appraisal systems that better align with local expectations and practices. This line of research would be especially valuable in diverse healthcare environments where cultural influences may play a significant role in shaping appraisal perceptions.
The long-term impacts of appraisal experiences on nurses’ career growth, job satisfaction, and commitment warrant investigation. Longitudinal studies are needed to understand how consistent, constructive appraisals affect nurses over time, particularly concerning professional development, retention, and mental well-being. Such studies could provide insights into whether positive appraisal experiences contribute to reduced burnout, increased retention, and more substantial commitment to the nursing profession.
Experimental research designs could be used to evaluate specific components of appraisal systems, such as feedback delivery methods or appraisal frequency, to determine which elements most effectively enhance nurse performance and satisfaction. Testing various appraisal models in controlled settings would offer valuable insights into best practices for designing and implementing appraisal processes.
Finally, research should examine the impact of technological innovations in appraisal processes, such as digital platforms and real-time feedback systems. As digital tools become more common in performance management, studies should explore how these innovations influence perceptions of appraisal fairness, feedback quality, and engagement. Understanding the benefits and challenges associated with these technologies could inform their integration into healthcare performance management practices.
Ethical Considerations
Compliance with ethical guidelines
The research received ethical approval from the Institutional Review Board (IRB) of the University of Essex, Essex, England. The study was carried out in adherence to the guidelines and principles set out in the “Declaration of Helsinki,” Good Clinical Practice (GCP), and in compliance with the laws and regulations governing research conducted by the Ministry of Public Health (MOPH), Qatar.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, study design and writing the original draft: Jincy Joseph Kutty; Investigation and final approval: All authors; Data extraction, review and editing: Bejoy Varghese.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are deeply thankful for the divine strength and resilience provided to them, their academic supervisor’s invaluable guidance, and the unwavering support from our families and friends throughout their dissertation journey. Their collective contributions were a cornerstone of our success and personal growth, for which our gratitude is immeasurable and deeply heartfelt.
References
Performance appraisal (PA) is a fundamental practice within organizations that evaluates employees’ job performance against predetermined criteria and objectives. This structured process provides organizations with a means to deliver feedback, identify strengths and areas for improvement, and align individual contributions with broader organizational goals. In healthcare, particularly nursing, effective PAs are critical due to their direct impact on patient outcomes and service quality [1].
As the workforce landscape continues to evolve, research into the dynamics of annual PAs has shed light on their multifaceted implications for individuals and the broader organizational context [2]. Annual PAs are not just tools for evaluation but are integral to fostering a sense of purpose and direction among employees, particularly in high-stake environments like healthcare [3]. Scholars have traced the evolution of PA and management practices, reflecting on over a century of progress [4]. Despite this evolution, challenges remain in ensuring that appraisal systems are effective, fair, and transparent across diverse healthcare settings.
The concept of PA s, especially within the nursing profession, has garnered significant attention in recent years. However, the literature reveals inconsistencies in the application and effectiveness of these appraisal systems across different contexts [5, 6]. While some studies demonstrate that PAs can significantly enhance job performance and organizational commitment among nurses, the impact of these appraisals varies widely depending on how they are implemented [7].
For instance, research shows that the active participation of nurses in the appraisal process, coupled with constructive feedback, can enhance their job performance and commitment to the organization [8]. Similarly, feedback provided through peer review programs has been shown to positively influence nurses’ perceptions, attitudes, and performance [9]. Aligning individual performance with organizational goals through PA systems remains a key challenge, particularly when disparities exist between individual objectives and broader organizational priorities [10]. This gap suggests a need for a more systematic understanding of how appraisal processes can be optimized to improve outcomes consistently.
While the importance of conducting annual appraisals and continuous performance reviews is widely acknowledged, the impact of these practices on staff development and motivation in nursing remains insufficiently examined [11]. Studies indicate that nurses’ job satisfaction and commitment can be significantly improved when they perceive the PA system as both fair and transparent [12]. Appraisal interviews have been shown to significantly improve nurses' performance by facilitating focused discussions and offering constructive feedback, supporting professional growth and skill enhancement [13].
Preparing for annual staff appraisals provides clarity on expectations and actionable feedback, fostering continuous professional development and improved performance [14]. Feedback mechanisms that are well-integrated into the appraisal process can facilitate open communication between supervisors and employees, ultimately guiding professional development [15]. This situation is particularly important in nursing, where continuous professional growth is essential to maintaining high standards of patient care.
Research indicates that nurses who receive regular, constructive feedback are more likely to be engaged and committed to their work [16]. Such feedback acknowledges employees’ efforts, recognizes their achievements and helps align their goals with organizational objectives [17]. Despite the recognized importance of feedback, its role in influencing job performance, job satisfaction, and overall engagement remains inconsistently addressed in the literature. This inconsistency underscores the need for a more detailed exploration of feedback’s role within appraisal systems.
The principles of fairness and transparency are critical to the success of PAs. Nurses’ perceptions of these factors significantly influence their job satisfaction, motivation, and commitment [18]. When appraisal processes are perceived as fair, they build trust within the organization and promote a culture of accountability [19]. Conversely, perceived unfairness can lead to frustration, demotivation, and potential burnout, which are significant concerns in the high-pressure setting of healthcare [20].
Studies have shown that transparent communication of evaluation criteria, processes, and outcomes is essential for reducing ambiguity and enhancing trust in the appraisal system [21]. Transparent communication allows employees to clearly understand how their performance is evaluated and what is expected of them, fostering alignment with organizational objectives and enhancing work engagement [22]. Furthermore, equitable appraisal systems that assess nurses’ contributions without bias foster a sense of justice within the workforce, increasing job satisfaction and commitment [7].
Despite the wealth of research on PAs, a significant gap exists in understanding how these appraisals can be consistently effective across different healthcare settings. Variability in the implementation of appraisal systems, coupled with employees' perceptions of fairness, significantly impacts their engagement and satisfaction, emphasizing the need for a deeper exploration of these dynamics within performance evaluations [23]. This study aims to fill this gap by conducting a systematic review of cross-sectional studies to identify the effects of annual appraisal processes on nurses’ job performance. By focusing on the role of constructive feedback, fairness, and transparency, this research seeks to provide evidence-based insights that can provide information for developing more effective appraisal systems tailored to the unique needs of the nursing profession.
This systematic review seeks to investigate the impact of annual appraisal processes on nurses’ job performance, mainly focusing on the effects of constructive feedback, the perceived fairness of the process, and the transparency of evaluation criteria. The study aims to comprehensively understand how these factors influence job satisfaction, motivation, and overall performance in diverse healthcare settings.
The findings of this review can shape nursing practice, management, and policy concerning PAs. By systematically understanding how annual appraisal processes impact nurses’ job performance, nursing management could aim their strategies at improving job satisfaction and patient care outcomes. Furthermore, the insights gained from this review may guide the development of more standardized and effective appraisal systems that are equitable, transparent, and conducive to professional growth in nursing.
Aim
The primary aim of this systematic review was to aluate the impact of annual appraisal processes on nurses’ job performance and satisfaction. Specifically, this review focuses on understanding how constructive feedback, fairness, and transparency within appraisal systems influence these outcomes. The other specific objective was to synthesize evidence and identify trends, gaps, and implications for nursing practice and policy.
Materials and Methods
This systematic review followed the Joanna Briggs Institute (JBI) methodology for prevalence systematic reviews [24] and the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [25]. As the protocol was not eligible for inclusion in PROSPERO, it was not numbered.
Search strategy
The initial step in the methodology involved developing a comprehensive search strategy to identify studies relevant to the research aims. A combination of relevant keywords and MeSH (medical subject headings) terms was utilized. Although it was primarily designed for PubMed, it is also adaptable to other databases. The search was conducted across several prominent databases, including PubMed, CINAHL, Cochrane Library, Scopus, PsycINFO, and ScienceDirect. The rationale for selecting these databases is based on their extensive health and medical literature coverage, ensuring a broad and inclusive search of peer-reviewed articles and relevant evidence-based resources.
The search strategy was tailored for each database to maximize the retrieval of pertinent studies. For example, in PubMed, the search included MeSH terms such as “professional nurse" or "staff nurse", "performance appraisal" or "annual appraisal" and "job satisfaction" or "job performance" combined using boolean operators. The specific search terms and strategies used for each database are outlined in Table 1.
The search was conducted for studies published in English between 2012 and 2022. The justification for this time frame is to capture recent developments and current practices in PA systems, reflecting changes and advancements in nursing and healthcare environments over the past decade.
Inclusion and exclusion criteria
Inclusion criteria were established to ensure the selection of relevant and meaningful studies.
Studies were included if they
● Involved nurses working in diverse healthcare settings,
● Focused on the impact of annual appraisal processes on job performance and job satisfaction,
● Were published in English between 2012 and 2022, and
● Employed a cross-sectional study design.
Exclusion criteria ruled out studies that were
● Randomized controlled trials, case-control studies, cohort studies, qualitative studies, and mixed-methods studies,
● Published outside the specified time frame, or
● Not directly addressing the impact of annual appraisal processes on nurses’ job performance.
Study selection
The study selection process involved multiple stages to ensure thorough screening and inclusion of relevant studies. First, all identified records underwent a duplicate removal process using EndNote reference management software. Following this, titles and abstracts were screened against the predefined inclusion and exclusion criteria. Any uncertainties or ambiguous cases were advanced to full-text screening for a more detailed evaluation. This methodical approach minimized bias and errors in the selection process, ensuring the inclusion of studies most pertinent to the research objectives.
Quality assessment
The quality of the selected studies was rigorously assessed using the JBI (Joanna Briggs Institute) critical appraisal checklist for analytical cross-sectional studies. This tool evaluates various aspects of study quality, including the clarity of study aims, appropriateness of the sample size and population, reliability of the data collection methods, and validity of the results and conclusions. Discrepancies in quality assessment were resolved through consultation with the supervisor, ensuring consistency and reliability in the evaluation process. Specific criteria such as the method of participant recruitment, measurement of variables, and control for confounding factors were considered in the assessment.
Data extraction
Data were extracted meticulously using a standardized form to capture all relevant information from each study. Key data points extracted included author details, publication year, study design, sample characteristics, specifics of the appraisal process, and principal findings related to job performance and satisfaction. The extraction process also considered contextual factors such as healthcare setting and geographical location, which could influence the outcomes. The extracted data provided the foundation for a comprehensive analysis of the appraisal processes and their impacts.
Data analysis
The data analysis employed a narrative synthesis approach, integrating descriptive and thematic analysis to examine the influence of annual appraisal processes on nurses’ job performance and satisfaction. This approach facilitated the identification of common themes such as feedback mechanisms, transparency, and fairness, which are critical in appraisal systems. Focusing on these key components, the analysis highlighted how constructive feedback can enhance job performance and professional growth, while transparency and fairness are linked to higher job satisfaction and organizational commitment among nurses. The synthesis also accounted for each study’s methodological quality and context, comprehensively understanding the evidence across diverse healthcare settings [8, 5].
Results
This systematic review followed the PRISMA (preferred reporting items for systematic reviews and meta-analyses) 2009 guidelines for systematic reviews [8], specifically using the PRISMA flow diagram to outline the study selection process. The initial search across six major databases yielded 764 records. After removing 64 duplicates, 700 records remained for screening. The titles and abstracts of these records were reviewed, excluding 588 articles that were primarily non-quantitative studies or did not focus on nursing PA . Subsequently, 112 full-text articles were assessed for eligibility. Of these, 101 articles were excluded for reasons such as not employing a cross-sectional study design or not directly addressing the impact of annual appraisal processes on nurses’ job performance. This process led to the inclusion of 11 cross-sectional studies in the qualitative synthesis, each providing valuable insights into the role of PAs in healthcare, particularly for nursing professionals (Figure 1). The synthesis of findings focused on several key themes that emerged from the studies: Constructive feedback, transparency and fairness, and professional development. These themes were identified based on the studies’ most frequently discussed appraisal processes and their reported impact on nurses’ job performance and satisfaction.
Constructive feedback
Many studies emphasized the importance of constructive feedback in PAs. It was found that feedback, when delivered in a supportive and actionable manner, helped nurses identify areas for improvement, boosted their confidence, and encouraged continuous professional growth. This theme aligns with literature that identifies feedback as a vital component in performance enhancement, as it guides improvement and reinforces positive behaviors within healthcare settings.
Transparency and fairness
Several studies linked transparency and fairness in the appraisal process to higher job satisfaction and organizational commitment among nurses. Transparency in evaluation criteria and fairness in the assessment process were associated with greater trust in leadership and reduced turnover intentions. This theme underscores the need for organizations to implement fair and transparent appraisal processes to build trust and motivate nurses to perform at their best.
Professional development
The studies highlighted that well-structured appraisal processes fostered professional development by encouraging goal-setting, skills assessment, and career planning. PAs that incorporated professional development goals enhanced nurses’ engagement with their work and supported long-term career growth. This theme emphasizes the potential of appraisal systems to go beyond evaluation and actively contribute to the professional development of nursing staff.
By analyzing these themes, the synthesis reveals that effective appraisal processes in nursing are not solely about performance measurement but are also integral to creating a supportive environment for career growth and job satisfaction. The findings suggest that healthcare institutions should prioritize designing and implementing appraisal systems that incorporate constructive feedback, maintain transparency and fairness, and support professional development. Such appraisal systems can enhance job performance and contribute to positive organizational outcomes in healthcare settings.
Characteristics of included studies
The findings from the included studies offer a detailed perspective on how PA systems influence nurses' job performance, satisfaction, and organizational commitment across healthcare settings.
The quality of appraisal processes emerged as a key factor in enhancing job satisfaction, as evidenced by a study that found fairness in appraisals fosters a more positive work environment and stronger organizational commitment [26]. Perspectives from healthcare professionals emphasized the need for tailored appraisals that align with the specific demands of healthcare roles, enhancing their effectiveness and relevance [27].
A lack of structured and fair appraisal systems was noted to negatively impact nurses’ motivation and performance, underscoring the importance of standardizing appraisal criteria to achieve better outcomes [28]. Structured appraisal systems, when implemented effectively, significantly boosted employee productivity and motivation, particularly through the integration of performance planning and reward mechanisms [29]. However, perceptions of inequity and limited career advancement opportunities within appraisal systems were associated with increased turnover intentions and diminished organizational commitment, revealing critical gaps in existing frameworks [29].
In some instances, appraisal systems were deemed ineffective due to poor communication of expectations, insufficient feedback, and inadequate developmental support, creating challenges for healthcare organizations striving to retain and motivate staff [31]. Transparent appraisal practices, on the other hand, have been shown to foster trust among nursing staff, enhancing engagement and satisfaction while creating a culture of accountability and fairness [32]. Fairness within appraisal systems has also been strongly correlated with higher levels of work engagement, highlighting the critical role of equitable processes in promoting satisfaction and retention among nurses [33].
Appraisal systems tailored to specific organizational contexts demonstrated greater effectiveness, as they addressed unique institutional challenges and priorities, thereby enhancing both individual and organizational outcomes [34]. Comprehensive appraisal systems also showed a significant impact on employee satisfaction, motivation, and performance, reinforcing their value in creating a supportive and productive work environment [35]. Finally, the inclusion of structured components, such as performance planning and clear reward mechanisms, has been pivotal in fostering workplace motivation and boosting productivity among nursing staff [36].
The findings from these studies present a nuanced understanding of PA systems in healthcare. While appraisals can improve job satisfaction, commitment, and performance through fairness, transparency, and constructive feedback, their absence or ineffective implementation can lead to dissatisfaction, reduced engagement, and higher turnover intentions. These results highlight the importance of refining appraisal processes to ensure equity, transparency, and a focus on professional growth (Table 2).
Discussion
This study aimed to review the studies that comprehensively evaluated the role of PA systems in influencing nurses' job performance, satisfaction, and organizational commitment across diverse healthcare settings. The findings revealed the critical importance of constructive feedback, fairness, transparency, and tailored appraisal processes in enhancing nursing outcomes.
A well-structured PA system can significantly boost nurses' job satisfaction and commitment. For example, the perceived quality of PA processes was found to be positively correlated with job satisfaction, underscoring the need for equitable and effective appraisal systems in healthcare institutions [26]. Similarly, structured appraisal systems with clearly defined performance criteria and fair assessment methods were observed to foster higher levels of motivation and commitment among nursing staff [27]. However, ineffective or poorly designed appraisal systems, such as those lacking standardized criteria, can lead to subjective evaluations that negatively affect nurses' engagement and productivity [28].
Feedback mechanisms emerged as a cornerstone of effective PA systems. Regular and meaningful feedback was highlighted as pivotal in motivating nurses and enhancing their professional development [29]. Constructive feedback not only helps nurses identify areas for improvement but also aligns their efforts with organizational goals, ultimately improving work outcomes [30]. Conversely, inadequate or poorly communicated feedback was identified as a barrier to the effectiveness of PA systems, leading to dissatisfaction and diminished trust among staff [31]. Transparent and equitable appraisal practices were shown to build trust within organizations, fostering engagement and job satisfaction [32].
Fairness in appraisal systems plays a crucial role in promoting positive work environments. Studies revealed that perceptions of fairness within the appraisal process were directly linked to higher work engagement and organizational commitment among nurses [33]. Additionally, appraisal systems that consider cultural and institutional dynamics were found to be more effective in meeting the diverse needs of healthcare professionals, further highlighting the importance of tailoring appraisals to specific contexts [34].
Effective communication emerged as another critical element in ensuring the success of PA systems. Clear communication of appraisal expectations and outcomes gives nurses a sense of purpose and direction, enhancing their satisfaction with the appraisal process [35]. Transparent communication also ensures alignment between individual performance and organizational objectives, strengthening staff engagement and productivity [36].
The broader impact of well-implemented PA systems extends beyond individual performance to improve organizational outcomes. Structured components, such as performance planning and reward systems, were found to significantly enhance employee productivity and motivation, ultimately benefiting overall hospital performance [37]. Furthermore, appraisal systems that integrate fairness and transparency were shown to reduce turnover intentions and improve organizational commitment among nurses [38].
Cultural and institutional considerations were identified as vital in shaping the effectiveness of PA systems. Flexible and context-specific appraisal frameworks were found to align more closely with the unique demands of nursing roles, enhancing their relevance and effectiveness [39]. For instance, appraisal systems designed to accommodate the complexities of clinical settings were observed to foster greater staff engagement and satisfaction [40].
Our findings support the evidence suggesting that well-structured appraisal systems can improve healthcare quality and patient outcomes. By prioritizing equity, transparency, and constructive feedback, healthcare institutions can foster a motivated and high-performing nursing workforce [5]. Moreover, appraisal systems tailored to the specific needs of nursing professionals were shown to enhance both individual and organizational outcomes, reinforcing the importance of adaptability in appraisal systems [3].
This systematic review study emphasizes the importance of constructive feedback, transparency, fairness, and effective communication within PA systems. These factors can significantly influence nurses' job performance, satisfaction, and commitment and contribute to organizational efficiency and patient care quality. By addressing these factors, healthcare institutions can refine their appraisal processes, ultimately fostering a more engaged and high-performing nursing workforce [41].
Study limitations
While this systematic review provides valuable insights into the impact of PA systems on nurses’ job performance, several limitations should be considered.
Firstly, the generalizability of the findings is potentiallylimited due to the specific contexts in which the included studies were conducted. Most studies were situated within specific healthcare environments and geographic regions, which may not fully capture the diversity of appraisal practices in nursing globally. As a result, the applicability of the findings may be restricted when attempting to generalize across various healthcare systems, especially in underrepresented or low-resource settings. Prior research highlights similar challenges in systematic reviews, as findings from studies in specific contexts may not always apply to larger populations [41].
Language and publication biases are additional limitations of this review. Only studies published in English
were included, which may have led to language bias and the potential exclusion of relevant studies in other languages.
This limitation could affect the review’s comprehe siveness by overlooking valuable perspectives from non-English-speaking regions. Furthermore, the review may be subject to publication bias, as studies with significant or positive findings are more likely to be published. This tendency may overestimate the effectiveness of PA systems and ultimately skew the conclusions, as highlighted in earlier methodological discussions [42].
Variability in methodological rigor and measurement tools among the selected studies may further impact
the consistency and reliability of the synthesized evidence.
The studies included in this review differed in study design, sample sizes, data collection methods, and measurement tools. For instance, some studies rely on self-report measures of job performance and satisfaction, which may introduce subjective bias and limit the objectivity of the findings. Additionally, methodological variability across the included studies poses challenges to synthesizing robust conclusions. The use of diverse measurement tools and inconsistencies in study quality align with prior findings that such heterogeneity hinders the generation of reliable results [40].
This variability in rigor across studies may compromise
the overall quality and uniformity of the evidence presented.
One of the strengths of this review is its systematic approach, adhering to PRISMA guidelines to ensure transparency and consistency in study selection, data extraction, and analysis. This rigorous approach helps mitigate selection bias and provides a structured foundation for synthesizing findings. However, a major limitation is the reliance on cross-sectional study designs, which inherently limit the ability to draw causal inferences. Crosssectional studies capture data at a single time, making it challenging to assess the long-term effects or causal relationships between appraisal practices and job performance outcomes. As a result, the conclusions drawn are primarily correlational, and caution should be exercised in interpreting these associations as causal. Furthermore, the reliance on cross-sectional designs within the included studies limits the ability to establish causation. This limitation underscores the need for longitudinal studies to validate findings and provide a more comprehensive understanding of the long-term effects of PA systems on nursing outcomes, a need echoed in previous reviews on healthcare performance management [19].
Conclusion
This systematic review aimed to examine the impact of PA processes on nurses’ job performance and job satisfaction, focusing on understanding the role of constructive feedback, transparency, and fairness in appraisal systems. The findings clarify the complex relationship between these appraisal elements and nurses’ motivation, commitment, and job performance. Specifically, constructive feedback emerged as a critical factor in enhancing job performance and satisfaction, reinforcing its role as a mechanism for professional growth and development in nursing.
While the selected articles provide valuable insights, limitations related to study scope, quality, and variability were observed, affecting the consistency of the findings. The review also highlights gaps in understanding the mechanisms through which feedback influences nurse performance, the contextual factors that impact perceptions of fairness, and the long-term effects of appraisal satisfaction on career trajectories. These gaps suggest that while PA positively influences nurse outcomes, a more nuanced and contextual approach is needed to maximize its benefits across diverse healthcare settings.
Despite potential biases, this review employed rigorous methods to enhance the credibility of its findings, contributing to a foundational evidence base for developing effective appraisal systems in nursing. By identifying key themes and areas for improvement, this review offers valuable guidance for healthcare institutions aiming to refine appraisal practices and researchers exploring the evolving healthcare landscape.
Implications for clinical practice
This systematic review underscores the critical role of PA systems in promoting nurses’ job performance, satisfaction, and professional growth. To maximize the effectiveness of appraisals, clinical organizations should prioritize enhancing the quality of feedback provided to nursing staff. Constructive, specific feedback supports skill development and fosters a culture of continuous improvement and engagement. Clinical institutions can enhance feedback quality by investing in communication skills training for appraisers, ensuring that feedback is delivered in a supportive, clear, and constructive manner. This training should emphasize empathy, clarity, and actionable suggestions to support nurses’ professional growth and job satisfaction.
Furthermore, the review suggests that appraisal systems should be tailored to the unique needs of the nursing workforce. This endeavor involves adapting appraisal processes to address nurses’ distinct roles, responsibilities, and challenges in different healthcare settings. Involving nurses in the design and evaluation of appraisal systems can promote a sense of ownership, fairness, and transparency, addressing bias concerns and ensuring that appraisals accurately reflect nurses’ contributions. By creating an inclusive and collaborative appraisal design process, healthcare institutions can build trust and enhance the perceived fairness of the appraisal system.
Additionally, integrating personalized development plans within PAs is recommended to help nurses set meaningful goals, define clear career paths, and identify areas for skill enhancement. Such individualized plans can boost motivation, clarify career trajectories, and align nurses’ growth objectives with organizational goals, ultimately improving job performance and long-term commitment. Personalized development plans encourage nurses to pursue further education, certifications, and skill-building activities, contributing to a more skilled and committed workforce.
The review further advocates for evaluating comprehensive outcomes in PAs, moving beyond traditional metrics to include aspects such as burnout, work-life balance, and interdisciplinary collaboration. Monitoring these outcomes allows healthcare institutions to identify areas where nurses may need additional support, helping to prevent burnout and promote overall well-being. Appraisals considering interdisciplinary collaboration can strengthen team dynamics, improve patient outcomes, and support a holistic approach to healthcare excellence.
Implications for future research
Future research should consider a mixed-methods approach to gain deeper insights into nurses’ perceptions and experiences with the PA process. Combining quantitative and qualitative data can capture both measurable outcomes and the nuanced perspectives of nurses, providing a more comprehensive understanding of the factors that influence appraisal satisfaction and effectiveness.
Another area for exploration is the influence of contextual factors, such as organizational culture, management style, and healthcare setting, on nurses’ perceptions of appraisal fairness and efficacy. Studies investigating how cultural, institutional, and regional differences impact perceptions of fairness could support the development of more tailored appraisal systems that better align with local expectations and practices. This line of research would be especially valuable in diverse healthcare environments where cultural influences may play a significant role in shaping appraisal perceptions.
The long-term impacts of appraisal experiences on nurses’ career growth, job satisfaction, and commitment warrant investigation. Longitudinal studies are needed to understand how consistent, constructive appraisals affect nurses over time, particularly concerning professional development, retention, and mental well-being. Such studies could provide insights into whether positive appraisal experiences contribute to reduced burnout, increased retention, and more substantial commitment to the nursing profession.
Experimental research designs could be used to evaluate specific components of appraisal systems, such as feedback delivery methods or appraisal frequency, to determine which elements most effectively enhance nurse performance and satisfaction. Testing various appraisal models in controlled settings would offer valuable insights into best practices for designing and implementing appraisal processes.
Finally, research should examine the impact of technological innovations in appraisal processes, such as digital platforms and real-time feedback systems. As digital tools become more common in performance management, studies should explore how these innovations influence perceptions of appraisal fairness, feedback quality, and engagement. Understanding the benefits and challenges associated with these technologies could inform their integration into healthcare performance management practices.
Ethical Considerations
Compliance with ethical guidelines
The research received ethical approval from the Institutional Review Board (IRB) of the University of Essex, Essex, England. The study was carried out in adherence to the guidelines and principles set out in the “Declaration of Helsinki,” Good Clinical Practice (GCP), and in compliance with the laws and regulations governing research conducted by the Ministry of Public Health (MOPH), Qatar.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, study design and writing the original draft: Jincy Joseph Kutty; Investigation and final approval: All authors; Data extraction, review and editing: Bejoy Varghese.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are deeply thankful for the divine strength and resilience provided to them, their academic supervisor’s invaluable guidance, and the unwavering support from our families and friends throughout their dissertation journey. Their collective contributions were a cornerstone of our success and personal growth, for which our gratitude is immeasurable and deeply heartfelt.
References
- Yang J, Ma J, Li L. The relationship between performance appraisal interval and employees’ proactive working behavior-analysis based on time-gain effect and time-loss effect. Frontiers in Psychology. 2023; 14:1213547. [DOI:10.3389/fpsyg.2023.1213547] [PMID]
- Camilleri MA. Using the balanced scorecard as a performance management tool in higher education. Management in Education. 2021;35(1):10-21. [DOI:10.1177/0892020620921412]
- Vaz D, Qureshi W, Temouri Y, Pereira V. Unbundling the complexity of performance management of healthcare providers in the Middle East. IIM Ranchi Journal of Management Studies. 2023; 8(2):55-71. [DOI:10.1108/IRJMS-03-2023-0026]
- DeNisi AS, Murphy KR. Performance appraisal and performance management: 100 years of progress? Journal of Applied Psychology. 2017; 102(3):421-33. [DOI:10.1037/apl0000085] [PMID]
- Sepahvand F, Mohammadipour F, Parvizy S, Zagheri Tafreshi M, Skerrett V, Atashzadeh-Shoorideh F. Improving nurses’ organizational commitment by participating in their performance appraisal process. Journal of Nursing Management. 2020; 28(3):595-605. [PMID]
- Bowen-Brady H, Haag-Heitman B, Hunt V, Oot-Hayes M. Asking for feedback: Clinical nurses’ perceptions of a peer review program in a community hospital. Journal of Nursing Administration. 2019; 49(1):35-41. [PMID]
- Brefo-Manuh AB, Anlesinya A. Performance appraisal justice and work attitudes of healthcare workers in Ghana. European Journal of Training and Development. 2023; 47(1/2):24-42. [DOI:10.1108/EJTD-02-2021-0027]
- Memon MA, Salleh R, Mirza MZ, Cheah JH, Ting H, Ahmad MS. Performance appraisal satisfaction and turnover intention: The mediating role of work engagement. Management Decision. 2019; 58(6):1053-66. [DOI:10.1108/MD-06-2018-0685]
- Pinero M, Bieler J, Smithingell R, Andre-Jones C, Hughes A, Fischer-Cartlidge E. Integrating peer review into nursing practice. American Journal of Nursing. 2019; 119(2):54-9. [DOI:10.1097/01.NAJ.0000553206.67083.65] [PMID]
- Ayers RS. Aligning individual and organizational performance: goal alignment in federal government agency performance appraisal programs. Public Personnel Management. 2015; 44(2):169-91. [DOI:10.1177/0091026015575178]
- Kay N, Pearson L, Knight K. How to undertake annual appraisals and ongoing performance reviews. Nursing Management. 2023; 30(2):28-33. [DOI: 10.7748/nm.2022.e2065]
- Nikpeyma N, Abed_Saeedi Z, Azargashb E, Alavi_Majd H. Problems of clinical nurse performance appraisal system: A qualitative study. Asian Nursing Research. 2014; 8(1):15-22. [DOI:10.1016/j.anr.2013.11.003] [PMID]
- Bigdeli A, Adel-Mehraban M, Namnabati M. The effect of the appraisal interview on nurses' performance in neonatal intensive care units. Iranian Journal of Nursing and Midwifery Research. 2019; 24(6):428-31. [DOI: 10.4103/ijnmr.IJNMR_14_19] [PMID]
- Price B. Preparing for your annual staff appraisal: Part 1. Nursing Standard. 2013; 27(20):49-55. [DOI: 10.7748/ns2013.01.27.20.49.c9503] [PMID]
- Yu X, Huang Y, Liu Y. Nurses’ perceptions of continuing professional development: A qualitative study. BMC Nursing. 2022; 21(1):162. [DOI:10.1186/s12912-022-00940-z] [PMID]
- Sreejith SS. An exploratory sequential mixed methods design to identify criteria for continuous performance evaluation. European Conference on Research Methodology for Business and Management Studies. 2023; 22(1):164-172. [DOI:10.34190/ecrm.22.1.1799]
- Mulegi T. An overview of performance of health workers in Uganda. IDOSR Journal of Humanities and Social Sciences. 2022; 7(1):113-24. [Link]
- Xu W, Pan Z, Li Z, Lu S, Zhang L. Job burnout among primary healthcare workers in rural China: A multilevel analysis. International Journal of Environmental Research and Public Health. 2020; 17(3):727. [DOI:10.3390/ijerph17030727] [PMID]
- Kennedy DM, Anastos CT, Genau MC Jr. Improving healthcare service quality through performance management. Leadership in Health Services. 2019; 32(3):477-92. [DOI:10.1108/LHS-02-2019-0006] [PMID]
- Karatepe OM, Avci T. Nurses’ perceptions of job embeddedness in public hospitals. SAGE Open. 2019; 9(1):1-13. [DOI:10.1177/2158244019828848]
- Rubel MRB, Kee DMH. Perceived fairness of performance appraisal, promotion opportunity, and nurses’ turnover intention: The role of organizational commitment. Asian Social Science. 2015; 11(9):183-94. [DOI:10.5539/ass.v11n9p183]
- Avolio BJ, Vogelgesang GR, Leroy H. The mediating effects of leader integrity with transparency in communication and work engagement/performance. The leadership quarterly. 2013; 24(3):405-13. [DOI: 10.1016/j.leaqua.2013.01.004]
- Taneja S, Srivastava R, Ravichandran N. Employees’ fairness perception towards performance appraisal system: Antecedents and consequences. Review of Managerial Science.2024; 18(1):2163–96. [DOI: 10.1007/s11846-023-00680-7]
- Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Systematic reviews of prevalence and incidence. In: Aromataris E, Munn Z, editors). JBI manual for evidence synthesis. North Adelaide: Joanna Briggs Institute: 2020. [Link]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009; 6(7):e1000097. [DOI:10.1371/journal.pmed.1000097] [PMID]
- Abed M, Banan R. Impact of appraisal feedback on nurse performance: A study in healthcare settings. Journal of Nursing Management. 2016; 24(3):295-302. [Link]
- Majidi S, Daneshkohan A, Zarei E, Ashktorab T. Perspectives of health workers on annual performance appraisal: A study in primary health care. International Journal of Healthcare Management.2020; 14(4):1190–7. [DOI:10.1080/20479700.2020.1755810]
- Awases MH, Bezuidenhout MC, Roos JH. Factors affecting the performance of professional nurses in Namibia. Curationis. 2013; 36(1):E1-8. [DOI: 10.4102/curationis.v36i1.108] [PMID]
- Ayyash H, Aljeesh Y. Nurses’ motivation and their performance at European Gaza Hospital in Gaza Strip. Journal of Al Azhar University-Gaza (Natural Sciences). 2011; 13(1):55-68. [Link]
- Rubel MRB, Kee DMH. Perceived fairness of performance appraisal, promotion opportunity and nurses turnover intention: The role of organizational commitment. Asian Journal of Social Science. 2015;11(9): 183-97. [DOI: 10.5539/ass.v11n9p183]
- Owin CA. Oluoch M, Kimemia F. Influence of performance management systems on employee productivity in county referral hospitals of Kiambu County. International Journal of Academic Research Business and Social Sciences. 2019; 9(3):1320–36. [DOI: 10.6007/IJARBSS/v9-i3/5799]
- Jaber MJ, Alshodukhi AM, Bindahmsh AA, Baker OG, Almutairi AO, Kanaan A, Preez SE, Jaber SJ. Nurses’ views and attitudes of the performance appraisal system efficacy and its impact on their work outcomes in a tertiary hospital. Global Journal on Quality and Safety in Healthcare. 2024; 1-10. [DOI:10.36401/JQSH-24-19]
- Hamdeen MS, Elewa AH, Mohamed SA. Staff nurse’s perception about performance-appraisal fairness and its relation to their work engagement. Egyptian Nursing Journal. 2022; 19(1):71-8. [DOI: 10.4103/enj.enj_53_21]
- Homauni, A., Mosadeghrad, A. M., & Jaafaripooyan, E. (2021). The effectiveness of employee performance appraisal system in health sector: Evidence from Iranian organizations. Asia Pacific Journal of Health Management.2021; 16(4): 36–44. [Link]
- Ismail F, Salahudin SN, Jaes LB, Yusoff MZ, Xin CJ, Alhosani AAH. The effect of performance appraisal system towards employee performance, employee motivation and employee satisfaction. Webology. 2022; 19(2):4686-704. [Link]
- Aly N, El-Shanawany S. The Influence of performance appraisal satisfaction on nurses’ motivation and their work outcomes in critical care and toxicology units. European Scientific Journal. 2016; 12(20):119-135. [DOI:10.19044/esj.2016.v12n20p119]
- Mok Kim Man M, Yie Yeen L. Factors affecting the effectiveness of employees’ performance appraisal in private hospitals in Malaysia. International Journal of Business and Society. 2021; 22 (1):257-5. [DOI: 10.33736/ijbs.3174.2021]
- Wang Y, Kim S, Rafferty A, Sanders K. Employee perceptions of HR practices: A critical review and future directions. The International Journal of Human Resource Management. 2019; 31(1):128–73. [DOI: 10.1080/09585192.2019.1674360]
- Ndlovu S, van Wyk NC, Leech R. Professional nurses’ perspectives of an ideal performance management process. Health SA Gesondheid 29(0), a2595. 2024. [DOI:10.4102/hsag.v29i0.2595]
- Veillard J, Champagne F, Klazinga N, Kazandjian V, Arah OA, Guisset AL. A performance assessment framework for hospitals: The WHO regional office for Europe PATH project. International Journal for Quality in Health Care. 2005; 17(6):487–96. [DOI: 10.1093/intqhc/mzi072]
- Colquitt JA, Conlon DE, Wesson MJ, Porter CO, Ng KY. Justice at the millennium: A meta-analytic review of 25 years of organizational justice research. Journal of Applied Psychology. 2013; 86(3):425-45. [DOI:10.1037/0021-9010.86.3.425] [PMID]
- Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. London: The Cochrane Collaboration; 2011. [Link]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |