Volume 13, Issue 1 (Winter 2025)
Iran J Health Sci 2025, 13(1): 11-22 |
Back to browse issues page
Ethics code: IR.MAZUMS.REC.1400.335
Clinical trials code: 0000
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Solimani Z, Mahmoudi H, Amiri H, Rezapour M. Typology of Knowledge, Attitudes, and Practices Toward Vaccines Among Medical Science Students in the Latest Epidemic. Iran J Health Sci 2025; 13 (1) :11-22
URL: http://jhs.mazums.ac.ir/article-1-987-en.html
URL: http://jhs.mazums.ac.ir/article-1-987-en.html
Department of Paramedicine, Amol Paramedical Sciences School, Mazandaran University of Medical Sciences, Sari, Iran. , maysam.rezapour@gmail.com
Keywords: Knowledge, Attitude, Practices, Concerns, COVID-19, Vaccine, Latent profile analysis (LPA), Iran
Full-Text [PDF 1061 kb]
(607 Downloads)
| Abstract (HTML) (2070 Views)
Full-Text: (607 Views)
Introduction
Originating in China and rapidly spreading worldwide, COVID-19 was declared a public health emergency of international concern by the World Health Organization (WHO) on January 30, 2020 [1]. Due to its rapid transmission from person to person, initial global strategies focused on early detection, isolation, and treatment of patients to curb the virus’s spread [2].
As the pandemic continued, it became evident that preventive measures such as social distancing and personal protective equipment alone were insufficient to control the virus’s widespread impact. This realization underscored the urgent need for effective vaccines to prevent transmission and mitigate severe outcomes associated with COVID-19 [3]. Vaccination has long been recognized as one of the most effective public health interventions, playing a crucial role in reducing mortality and controlling infectious diseases such as polio and measles. Besides providing individual protection, widespread vaccination establishes herd immunity, thereby protecting vulnerable populations who cannot be vaccinated [4].
However, the success of vaccination depends on its acceptance by society, given the production of vaccines by many countries [5]. Despite many efforts to produce a safe and effective vaccine, people are reluctant to accept the vaccine [6]. The WHO’s Strategic Advisory Group on Immunization (SAGE) [7] defined vaccine hesitancy as a “delay in accepting or rejecting vaccination despite the availability of vaccination services,” which could vary in form, time, place, and intensity [7, 8, 9]. Concerns and hesitancy about vaccines are growing worldwide, and WHO identified it as one of the top ten global health threats in 2019 [10]. In many countries, misinformation and hesitancy about vaccination create fundamental barriers to achieving community coverage and immunity [11, 12]. Vaccine acceptance is influenced by several factors, including knowledge of the potential for COVID-19 release, perceived safety of the vaccine, perceived effectiveness of the vaccine, perceived risk as well as negative perceptions, fear of transmission to relatives, fear of long-term side effects, and depression symptoms [11, 13]. Silva et al. indicated that older people’s perceptions, knowledge, and attitudes were significantly associated with acceptance of COVID-19 vaccination, and also, concerns about the safety and efficacy of COVID-19 vaccines were significant predictors of higher vaccination rates [14].
We rely on vaccines to help us return to normal circumstances, so addressing the issue of vaccine rejection is essential. Hence, interpreting people’s knowledge, attitudes, practices, and concerns (KAPC) about the COVID-19 vaccine is crucial to improving its widespread acceptance [15]. Although some previous studies [16, 17]examined the association between KAPC and vaccine injection, there is no study of the relationship between the typology of KAPC and vaccine injection among medical students. The typology of KAPC refers to categorizing people into discrete groups according to patterns of knowledge, attitudes, practices, and concerns about the COVID-19 vaccine [18]. In addition, information about examining the relationship between the typology of KAPC and vaccine acceptance can help manage the COVID-19 vaccine program. Also, the findings of this study can provide health care professionals insight into ways to encourage vaccination uptake by uncovering patterns of KAPC about the vaccine among the student population.
Therefore, this study pursues two specific objectives: Classification of Mazandaran University of Medical Sciences students based on KAPC about the COVID-19 vaccine and determining the relationship between these patterns and performing COVID-19 vaccination.
Materials and Methods
Study setting and population
A cross-sectional study design was used to collect the data about the students’ injection of
COVID-19 vaccine and their perception of KAPC toward COVID-19 vaccine.
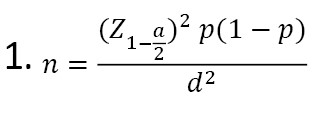
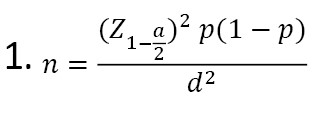
Students were recruited from the Public Health, Medicine, Dentistry, Nursing, Pharmacy, and Paramedicine faculties at Mazandaran University of Medical Sciences in north Iran from May 22 to June 23, 2021. A sample of 413 students was chosen from various academic levels, ranging from the second semester of undergraduate programs to final-year students. Pre-clinical and clinical students were included to capture diverse knowledge, attitudes, and practices regarding vaccination. The sample size was determined using the single population proportion formula (Equation 1), assuming a 5% margin of error, a 95% confidence interval, and 50% the expected proportion of vaccine acceptance.
The current study collected the data using the Google Form platform as an online survey, and the generated link was shared with the WhatsApp Group of each college and the students’ email addresses. The link was also shared personally to the contact list of investigators and research assistants. The inclusion criterion was students currently enrolled in the Mazandaran University of Medical Sciences faculties. The exclusion criteria were students actively attending classes or clinical rotations and incomplete questionnaires. Also, students who could not receive the COVID-19 vaccine due to medical contraindications were excluded from the analysis. Informed consent was obtained from study participants by including the details of the study objectives at the beginning of the survey and expressing voluntary and confidential information via anonymous filling of the questionnaire.
Study measures
The questionnaire in this study had two sections. The first section included sociodemographic variables such as age, gender, field, and a question regarding getting the COVID-19 vaccine (vaccine injection: “No” with code=0; “yes (one dose)” with code=1; and “yes (two doses) with code=2”).
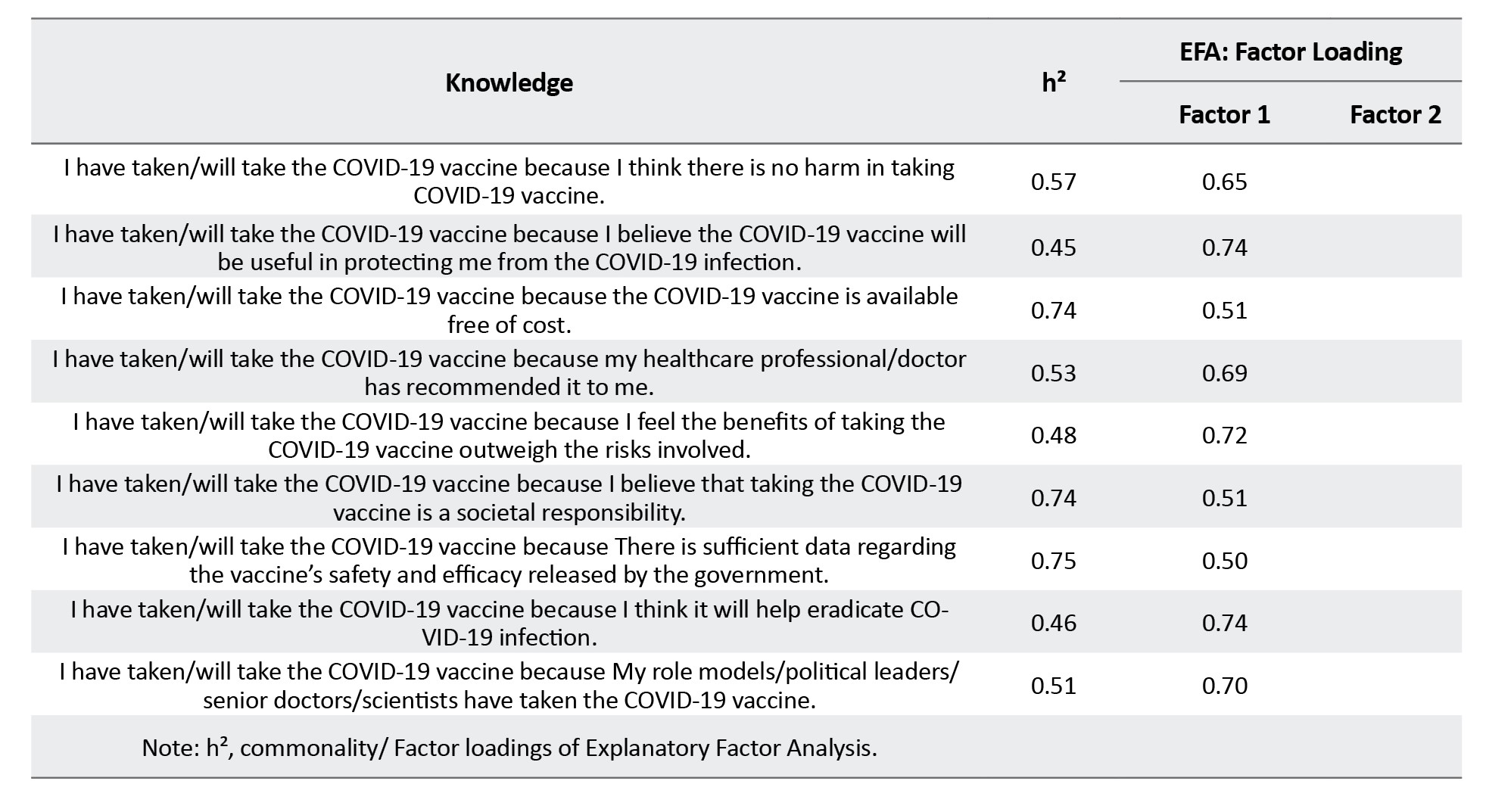
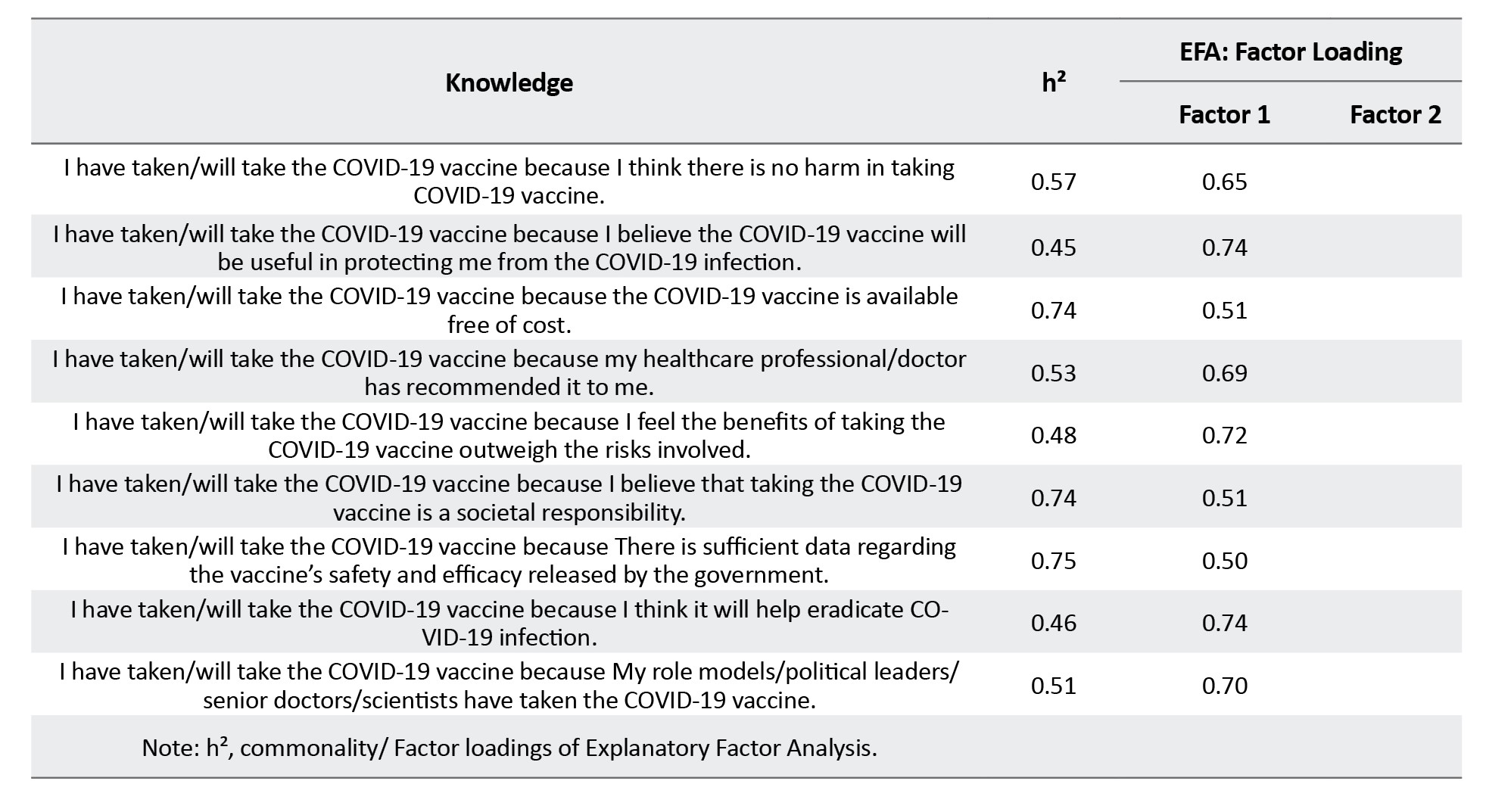
The second section of the questionnaire was the items related to KAPC toward the COVID-19 vaccine that was developed and validated among the Indian general population aged above 18 years by Kumari et al. [19]. The Persian version of the COVID-19 vaccine KAPC questionnaire was validated by explanatory factor analysis (EFA) [20]. The internal consistency reliability subscales were acceptable (Appendix 1).

The questionnaire comprised 10 questions for the knowledge scale, 5 for the attitude scale, 10 for the practice scale, and 6 for the concerns scale. The response options for knowledge scale questions were “eligible” (code=2)/ “not eligible” (code=0) and “do not know” (code=1). The response options of attitude, practices, and concerns scale questions were “strongly agree” (code=5)/ “agree” (code=4), “neither agree nor disagree” (code=3), “disagree” (code=2), and “strongly disagree” (code=1). The scores for related questions of each subscale were summed to calculate the total score of each subscale. Higher scores indicate more positive knowledge, attitudes, and practices toward vaccination. Lower total scores on the concern scale reflect fewer concerns or hesitancies regarding the vaccine.
Data analysis
The analysis of data was conducted in two steps. First, we conducted a latent profile analysis (LPA) to identify subgroups of the COVID-19 vaccine KAPC patterns. Second, the association between the typology of KAPC and vaccine injection was measured by logistic regression analysis. Also, the scores of KAPC were compared by one-way analysis of variance (ANOVA) and Bonferroni post hoc test. In addition, the chi-square was performed to examine the typology of the relationship between KAPC and gender.
To identify the optimal typology of KAPC by LPA, we used an iterative approach with an increasing number of profiles. The KAPC subscales were converted to z-scores for ease of interpretation. The analysis started with a 2-profile model, gradually increasing successive models until the model was no longer interpretable. Fit was assessed using the Akaike information criterion (AIC), Bayesian information criterion (BIC), sample size adjusted Bayesian information criterion (aBIC), Lo–Mendell–Rubin likelihood ratio test (LMR-LRT), and Vuong-Lo–Mendell–Rubin likelihood ratio test (VLMR-LRT) [21]. Low BIC, AIC, and aBIC values show a better model fit. Nylund et al., in a simulation study, showed that aBIC is a superior index compared to BIC and AIC. A significant LMR-LRT and VLMR-LRT indicate that the latent profile model with k profiles was better than the simpler k - 1 profile model [22].
Furthermore, the entropy value (0–1) was considered to assess the quality of the classification of individuals into profiles, and values closer to 1 showed a more desirable classification [23]. LPA was performed using Mplus software, version 8.3, and ANOVA and logistic regression were performed by STATA software, version 16.
Results
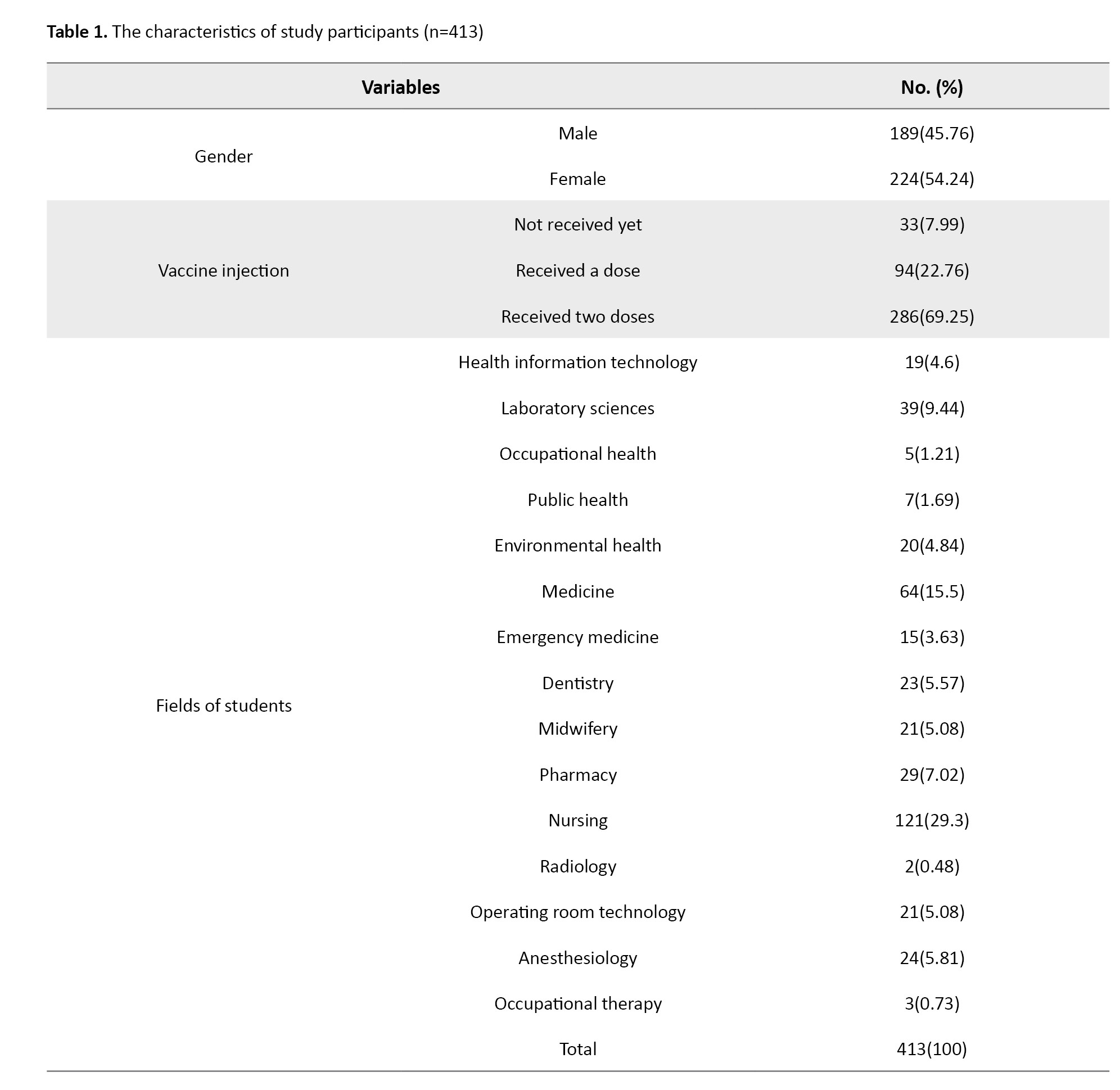
A total of 413 (189 male and 224 female) medical science students from various fields participated in the study (Table 1).
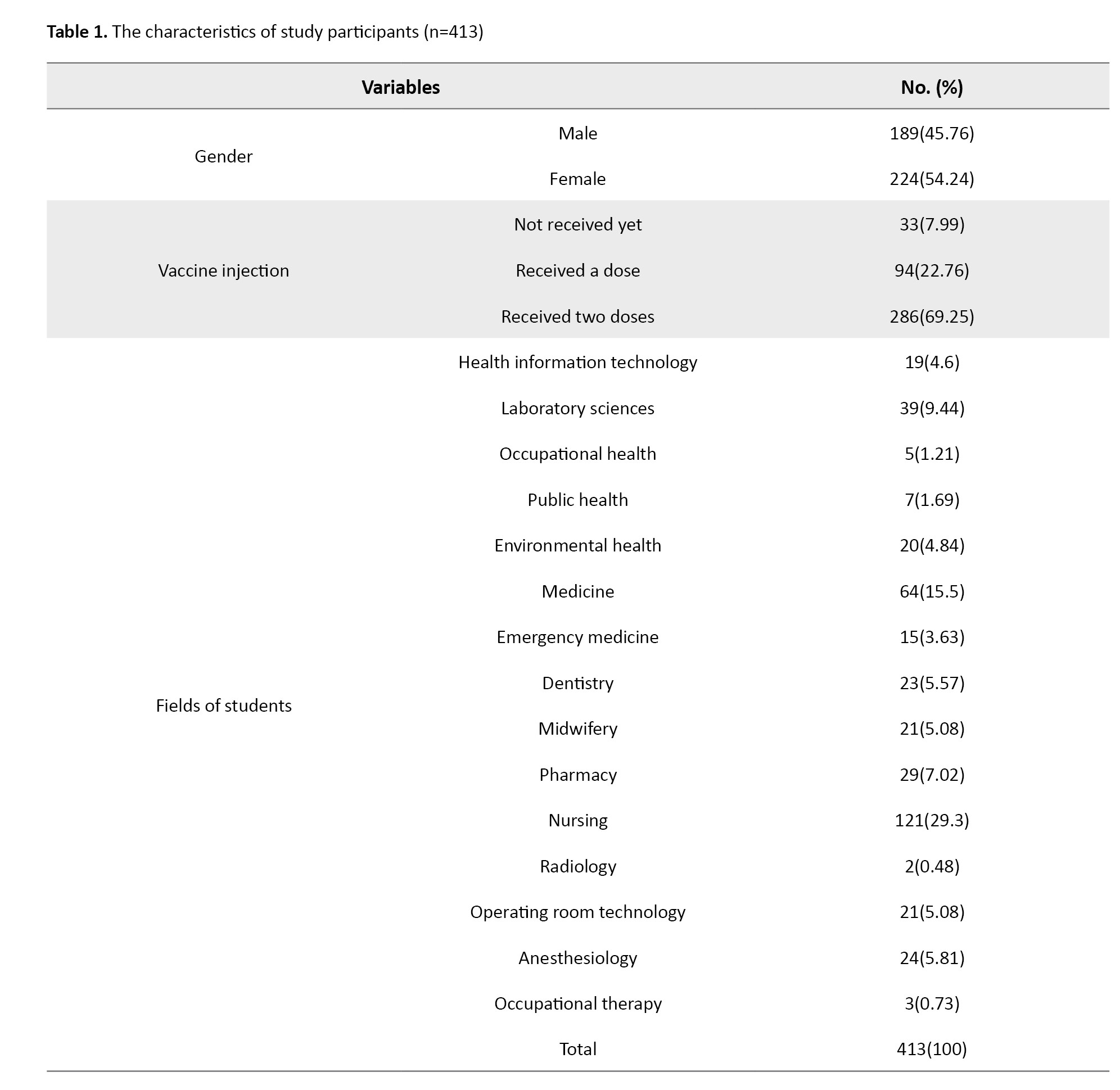
The Mean±SD age of students was 22.4±2.5 years (ranges 18 to 38).
A series of 2 to 5 latent profile models were estimated based on the KAPC scales (Table 2).
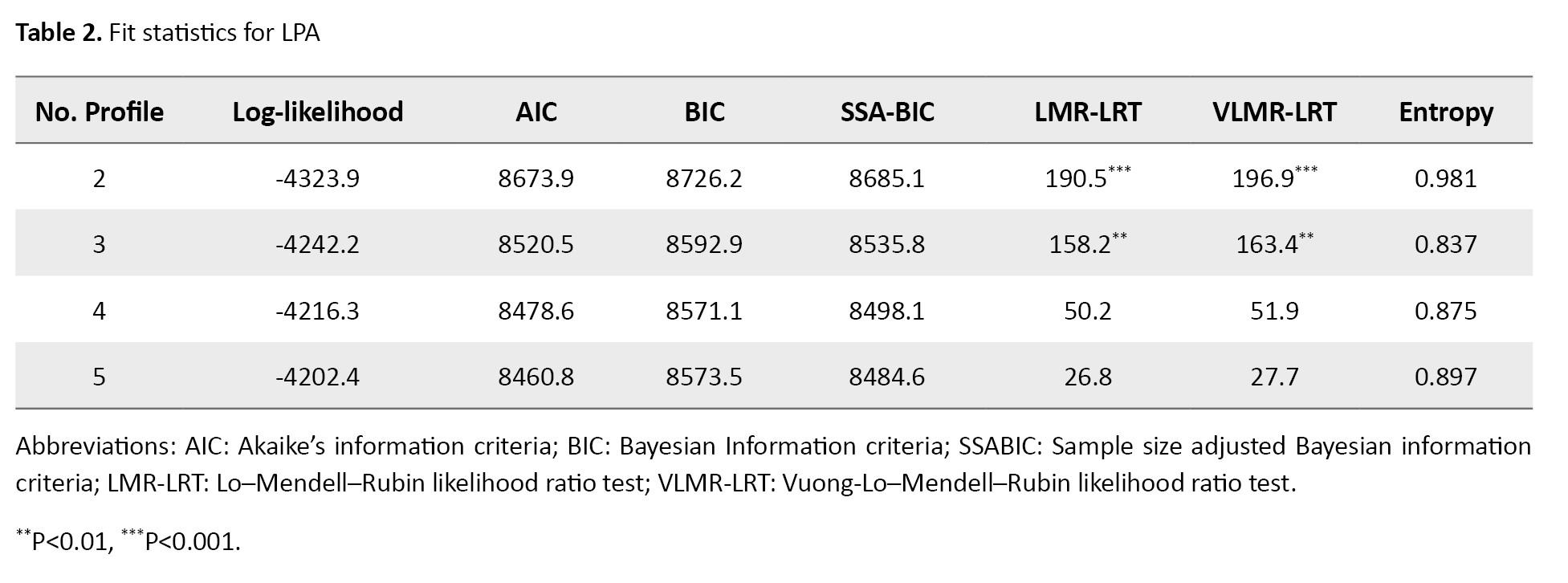
The AIC, BIC, and a-BIC had a decreasing trend with the increase in the number of profile models, and they never reached a minimum value, so they did not identify the best-fitting model. However, the LMR-LRT and VLMR-LRT were favored for the 3-profile model as the greatest number of profiles for which the P of the test was significant. The nonsignificant P for the 3-profile model indicated that a 4-profile model would not improve model fit over a 3-profile model. The entropy values were high for all the latent profile models, although they were highest for the 2-profile model.
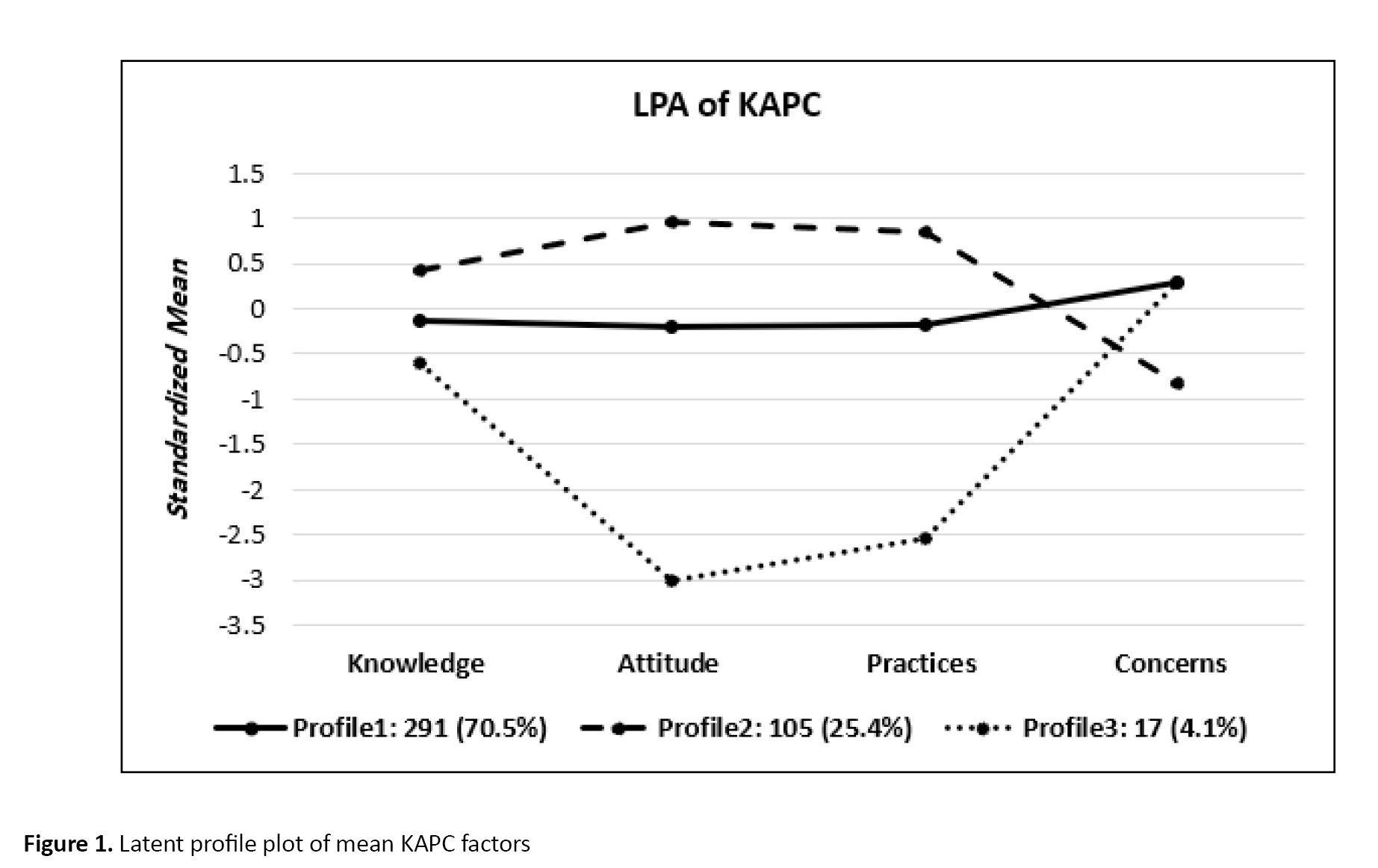
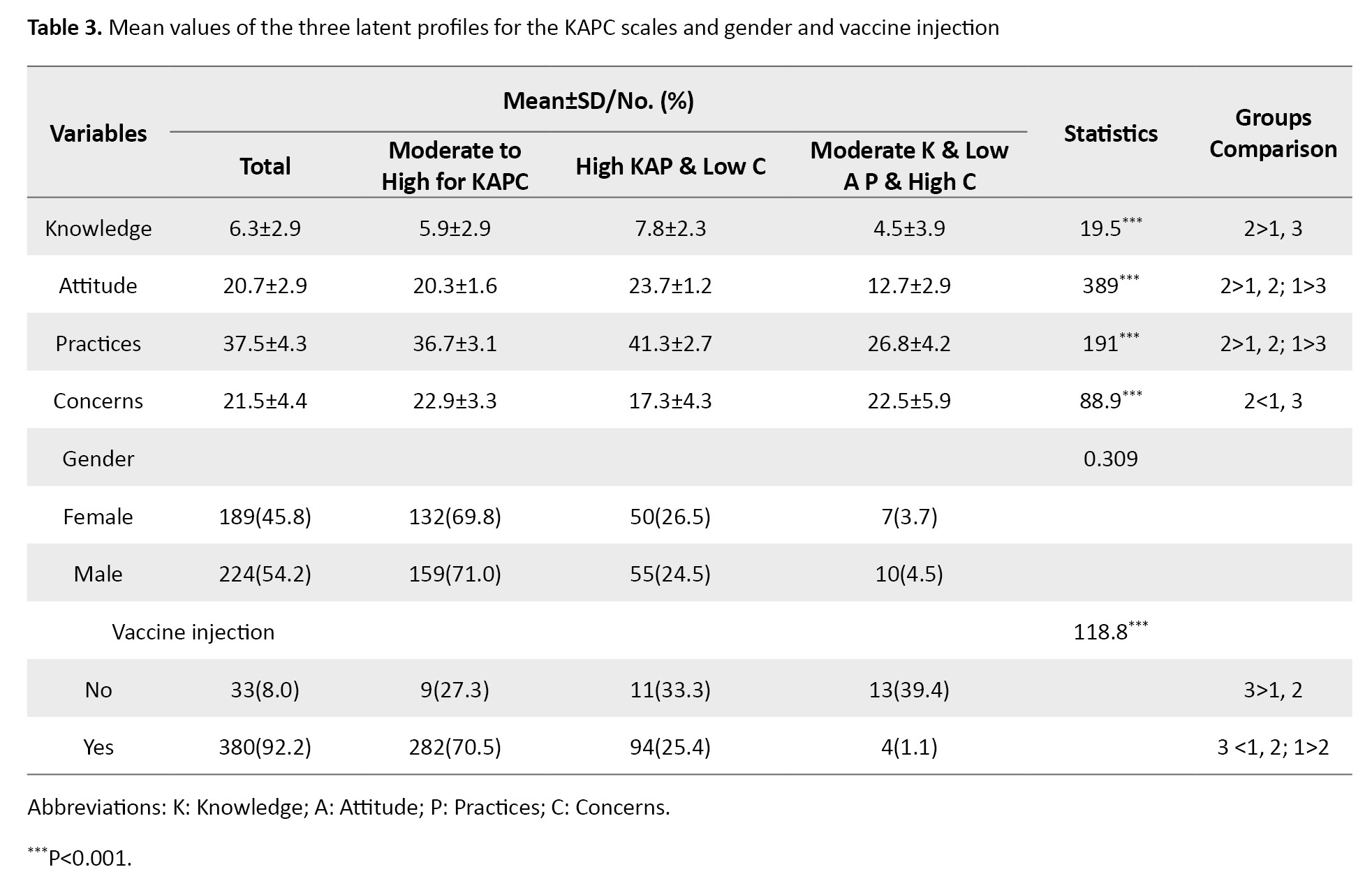
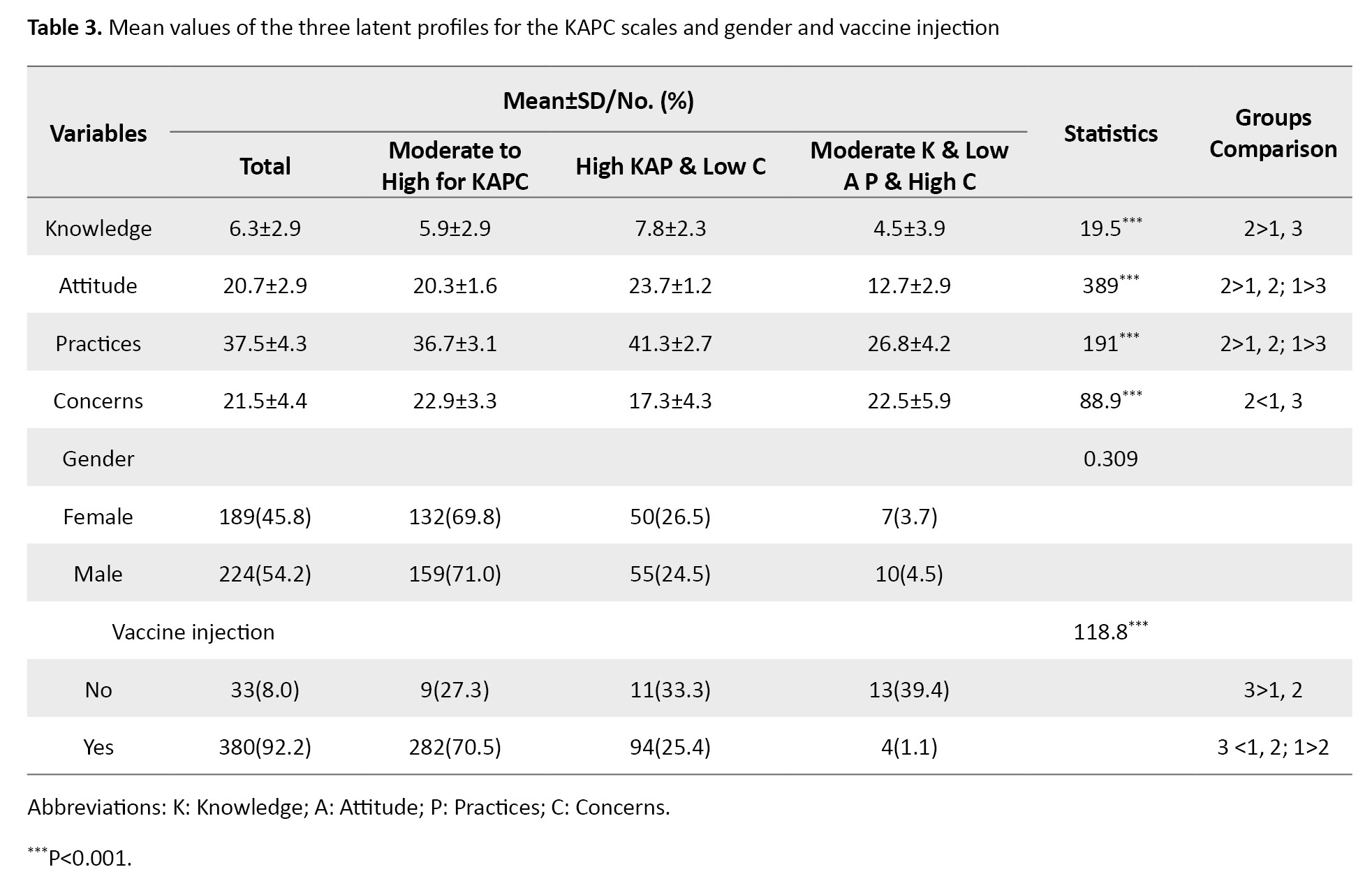
Considering both fit indices and substantive interpretation, the 3-profile model was selected as the preferred model. Figure 1 shows the latent indicator means for the 3-profile model. As shown in Figure 1, Profile 1 (70.5% of the sample, n=291) w::as char::acterized by low moderate to up for KAPC scales and was labeled as “moderate to up for KAPC.” Profile 2 (25.4% of the sample, n=105) w::as char::acterized by high knowledge, attitude, practices, and low concerns scales and was labeled as “high KAP & low C.” Profile 3 (4.1% of the sample, n=17) w::as char::acterized by moderate knowledge, low attitude, practices, and high concerns, and was labeled as “moderate K & low AP & high C.”
Also, the mean scores of the COVID-19 vaccine KAPC scales are compared within- profiles and presented in Table 3.
The associations of the COVID-19 vaccine KAPC typologies with vaccine injection by logistic regression are given in Table 4.
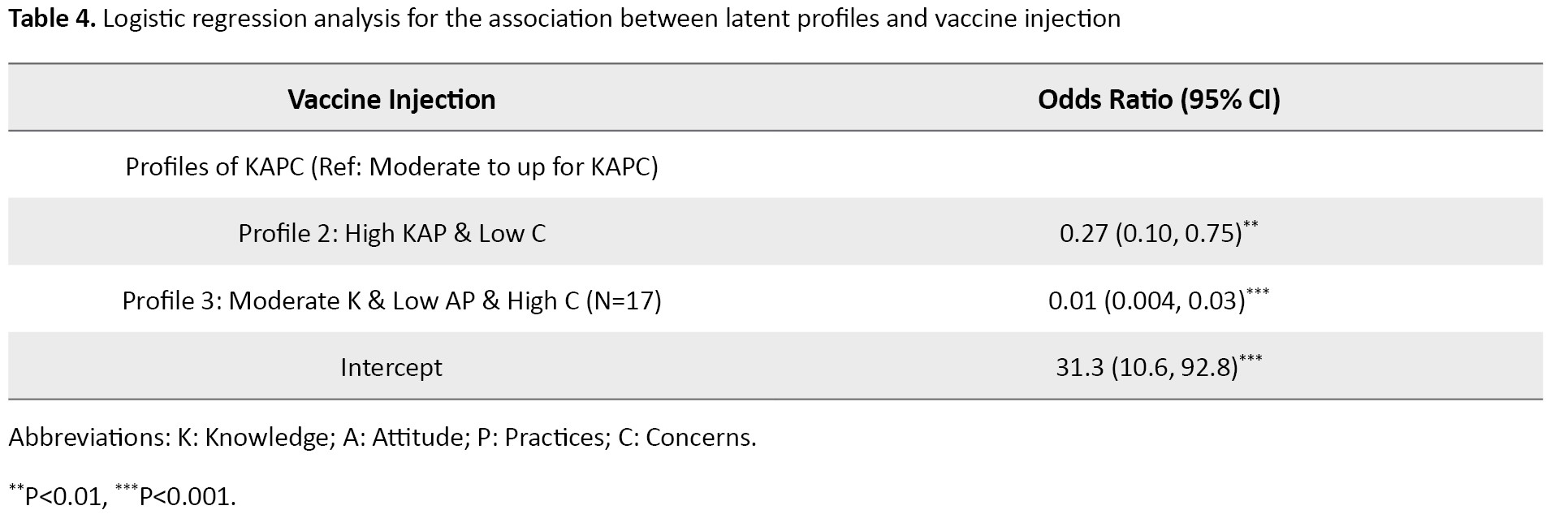
The individuals with membership in profile 2 relative to profile 1 have 73% less odds of injecting the vaccine. Also, individuals with membership in profile 3 relative to profile 1 have 99% less odds of injecting the vaccine.
Discussion
The current study showed three profiles (patterns) of the COVID-19 vaccine KAPC. These patterns included “moderate to up for KAPC,” “high KAP & low C,” and “moderate K & low AP & high C.” Students in the three profiles differed significantly in their KAPC factors. In other words, important heterogeneity or diversity of KAPC factors among students provides posterior probabilities of each individual’s membership in each profile. The most common pattern was “moderate to high for KAPC,” which included 70% of the study population, while the lowest pattern was “moderate K & low AP & high C,” with 4% of the study population.
Profile 3 was especially characterized by a very negative attitude towards COVID-19. Profile 3’s knowledge was almost similar but lower than that of the other two profiles. In addition, profile 3 had the highest value regarding the level of concern compared to profile 1. However, one of the characteristics of profile 2 was their highest level of knowledge, practices, and attitude. Profile 1 had a moderate attitude, knowledge, practices, and concern. The results showed that profile 3 had a 99% lower chance of vaccination than group 1. Moreover, the chance of vaccination in profile 2 was 63% lower than in profile 1.
Numerous studies have been performed on different strata of the medical staff, from physicians, nurses, dentists, and public health specialists, indicating an appropriate level of knowledge and attitude toward COVID-19 [24-27]. However, in the current study, participants were categorized according to knowledge, attitudes, and practices related to COVID-19. Classifying individuals in homogeneous groups can help create interventions for increasing the tendency to accept and subsequently for injection vaccines. Interventions should be comprehensive and specific to the target population. Intervenors should apply appropriate strategies for the best combination of interventions based on the typology.
As mentioned, profile 1, with a medium to a high level in terms of KAPC, is more inclined to receive vaccines than the others. Therefore, an average KAPC about COVID-19 increases the chance of receiving the vaccine. These findings are consistent with a previous study in Korea, which showed that individuals’ knowledge of COVID-19 and their concern and attitudes toward preventive measures can affect their performance concerning vaccination [28]. The finding is reasonable because high KAP leads to low concerns and vaccine acceptance.
Knowledge is a prerequisite for creating prevention beliefs, forming a positive attitude, and promoting positive behaviors, and people’s knowledge and attitude toward the disease can affect their coping strategies and behaviors [29]. Naturally, the audience of the present study (medical students) is expected to have an acceptable knowledge of COVID-19 and its vaccine. Also, various training sources at different levels, from university to society, have increased their knowledge about this epidemic, and usually, increasing knowledge leads to a change in people’s attitudes and consequently changes their practice [30].
Another studied component is attitude. It is influenced by knowledge, which can be obtained through experience [31]. Attitude in social psychology is evaluating a subject, which varies from negative to very positive [32]. Each person’s complex and unique psychological structure is acquired through individual experience and modeling. Attitude combines beliefs and emotions to evaluate different concepts in different ways and predict future behaviors [33]. According to the theory of planned behavior, attitude plays a vital role in health care behaviors [34], such as having a better function and receiving the vaccine because they feel optimistic about dealing with COVID-19, socially and individually.
Another component is concerns, which occur when a stimulus or event threatens our physical, mental, or social health. Thus, concerns and fear have an external source as a common emotion to increase energy to preserve life [35, 36]. The fear and concern about the recurrence of the disease persist even after treatment. COVID-19 concern means anxiety about being infected due to anonymity and cognitive ambiguity [37]. A moderate level of concern and anxiety creates the motivation to pursue treatment and seek prevention.
Therefore, students should have a reasonable understanding of what behaviors are appropriate for the prevention and control of COVID-19 disease (awareness and knowledge). This knowledge benefits their attitude and practice [38] to promote their health and show a greater willingness to be vaccinated for improvement. According to profile 1, acceptable knowledge about COVID-19 changes attitudes, and moderate attitude and concern affect the practice and, consequently, the desire to receive the COVID-19 vaccine.
Conclusion
This study divided individuals into three categories according to KAPC about COVID-19. The relationships between these categories and the receiving COVID-19 vaccine were found to be significant. These patterns of KAPC have various distributions in vaccine injection and even in controlling the pandemic. It seems that governmental authorities should take measures to improve the knowledge, attitude, and practice of the people appropriate to each profile and identify any obstacles to their promotion.
Study limitations
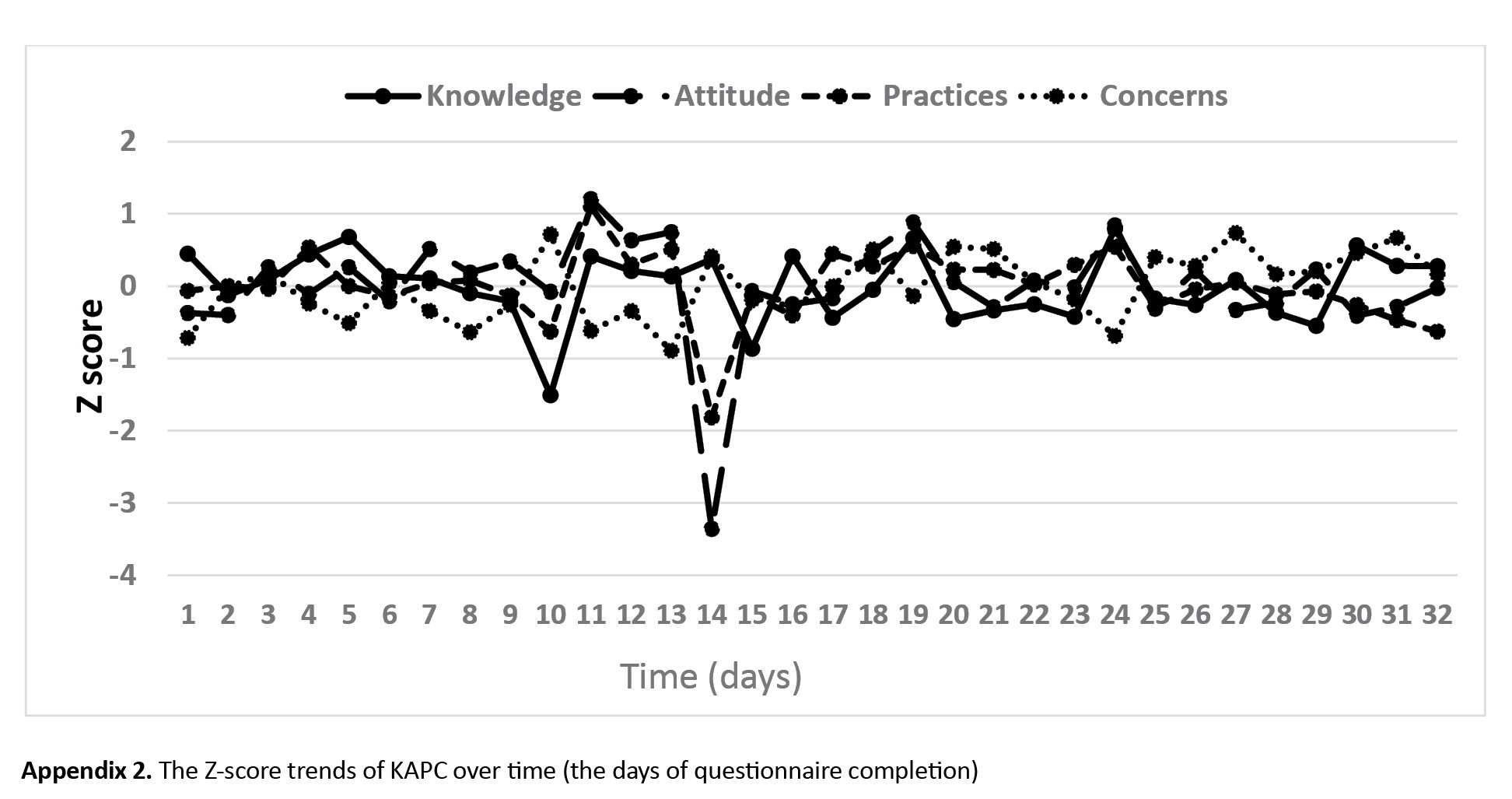
The current study has several limitations. First, knowledge and attitude in epidemic conditions are unstable. However, our study showed that the knowledge and attitude for participation during data collection was stable (Appendix 2). Second, the survey was conducted online, so respondents may not represent all medical sciences students. Third, this study’s population was medical students, so the generalizability of these findings to other population subgroups is with caution. Finally, the study design was cross-sectional, and the extracted profiles of KPAC were extracted simultaneously. Some ambiguities, such as “Is there change between latent profiles across time? If so, how can this change be characterized?” Need to be addressed in future research by longitudinal study design.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics in Research Committee of Mazandaran University of Medical Sciences, Sari, Iran (Code: IR.MAZUMS.REC.1400.335). The inquired data were anonymous and unidentifiable. Informed consent was obtained from all participants, and all methods were followed, following the relevant guidelines and regulations.
Funding
This study was supported by Mazandaran University of Medical Sciences, Sari, Iran (Code: 10283).
Authors contributions
Conceptualization, visualization, and funding acquisition: Zeinab Solimani and Maysam Rezapour; Data curation, writing the original draft: Zeinab Solimani and Hamed Mahmoodi; Supervision, formal analysis, methodology, project administration, and software: Maysam Rezapour; Investigation and validation: Zeinab Solimani and Hadis Amiri; Resources: Hamed Mahmoodi and Hadis Amiri; Review, and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank all participants in this study and the Student Research Committee (SRC) of Mazandaran University of Medical Sciences, Sari, Iran.
References
Originating in China and rapidly spreading worldwide, COVID-19 was declared a public health emergency of international concern by the World Health Organization (WHO) on January 30, 2020 [1]. Due to its rapid transmission from person to person, initial global strategies focused on early detection, isolation, and treatment of patients to curb the virus’s spread [2].
As the pandemic continued, it became evident that preventive measures such as social distancing and personal protective equipment alone were insufficient to control the virus’s widespread impact. This realization underscored the urgent need for effective vaccines to prevent transmission and mitigate severe outcomes associated with COVID-19 [3]. Vaccination has long been recognized as one of the most effective public health interventions, playing a crucial role in reducing mortality and controlling infectious diseases such as polio and measles. Besides providing individual protection, widespread vaccination establishes herd immunity, thereby protecting vulnerable populations who cannot be vaccinated [4].
However, the success of vaccination depends on its acceptance by society, given the production of vaccines by many countries [5]. Despite many efforts to produce a safe and effective vaccine, people are reluctant to accept the vaccine [6]. The WHO’s Strategic Advisory Group on Immunization (SAGE) [7] defined vaccine hesitancy as a “delay in accepting or rejecting vaccination despite the availability of vaccination services,” which could vary in form, time, place, and intensity [7, 8, 9]. Concerns and hesitancy about vaccines are growing worldwide, and WHO identified it as one of the top ten global health threats in 2019 [10]. In many countries, misinformation and hesitancy about vaccination create fundamental barriers to achieving community coverage and immunity [11, 12]. Vaccine acceptance is influenced by several factors, including knowledge of the potential for COVID-19 release, perceived safety of the vaccine, perceived effectiveness of the vaccine, perceived risk as well as negative perceptions, fear of transmission to relatives, fear of long-term side effects, and depression symptoms [11, 13]. Silva et al. indicated that older people’s perceptions, knowledge, and attitudes were significantly associated with acceptance of COVID-19 vaccination, and also, concerns about the safety and efficacy of COVID-19 vaccines were significant predictors of higher vaccination rates [14].
We rely on vaccines to help us return to normal circumstances, so addressing the issue of vaccine rejection is essential. Hence, interpreting people’s knowledge, attitudes, practices, and concerns (KAPC) about the COVID-19 vaccine is crucial to improving its widespread acceptance [15]. Although some previous studies [16, 17]examined the association between KAPC and vaccine injection, there is no study of the relationship between the typology of KAPC and vaccine injection among medical students. The typology of KAPC refers to categorizing people into discrete groups according to patterns of knowledge, attitudes, practices, and concerns about the COVID-19 vaccine [18]. In addition, information about examining the relationship between the typology of KAPC and vaccine acceptance can help manage the COVID-19 vaccine program. Also, the findings of this study can provide health care professionals insight into ways to encourage vaccination uptake by uncovering patterns of KAPC about the vaccine among the student population.
Therefore, this study pursues two specific objectives: Classification of Mazandaran University of Medical Sciences students based on KAPC about the COVID-19 vaccine and determining the relationship between these patterns and performing COVID-19 vaccination.
Materials and Methods
Study setting and population
A cross-sectional study design was used to collect the data about the students’ injection of
COVID-19 vaccine and their perception of KAPC toward COVID-19 vaccine.
Students were recruited from the Public Health, Medicine, Dentistry, Nursing, Pharmacy, and Paramedicine faculties at Mazandaran University of Medical Sciences in north Iran from May 22 to June 23, 2021. A sample of 413 students was chosen from various academic levels, ranging from the second semester of undergraduate programs to final-year students. Pre-clinical and clinical students were included to capture diverse knowledge, attitudes, and practices regarding vaccination. The sample size was determined using the single population proportion formula (Equation 1), assuming a 5% margin of error, a 95% confidence interval, and 50% the expected proportion of vaccine acceptance.
The current study collected the data using the Google Form platform as an online survey, and the generated link was shared with the WhatsApp Group of each college and the students’ email addresses. The link was also shared personally to the contact list of investigators and research assistants. The inclusion criterion was students currently enrolled in the Mazandaran University of Medical Sciences faculties. The exclusion criteria were students actively attending classes or clinical rotations and incomplete questionnaires. Also, students who could not receive the COVID-19 vaccine due to medical contraindications were excluded from the analysis. Informed consent was obtained from study participants by including the details of the study objectives at the beginning of the survey and expressing voluntary and confidential information via anonymous filling of the questionnaire.
Study measures
The questionnaire in this study had two sections. The first section included sociodemographic variables such as age, gender, field, and a question regarding getting the COVID-19 vaccine (vaccine injection: “No” with code=0; “yes (one dose)” with code=1; and “yes (two doses) with code=2”).
The second section of the questionnaire was the items related to KAPC toward the COVID-19 vaccine that was developed and validated among the Indian general population aged above 18 years by Kumari et al. [19]. The Persian version of the COVID-19 vaccine KAPC questionnaire was validated by explanatory factor analysis (EFA) [20]. The internal consistency reliability subscales were acceptable (Appendix 1).

The questionnaire comprised 10 questions for the knowledge scale, 5 for the attitude scale, 10 for the practice scale, and 6 for the concerns scale. The response options for knowledge scale questions were “eligible” (code=2)/ “not eligible” (code=0) and “do not know” (code=1). The response options of attitude, practices, and concerns scale questions were “strongly agree” (code=5)/ “agree” (code=4), “neither agree nor disagree” (code=3), “disagree” (code=2), and “strongly disagree” (code=1). The scores for related questions of each subscale were summed to calculate the total score of each subscale. Higher scores indicate more positive knowledge, attitudes, and practices toward vaccination. Lower total scores on the concern scale reflect fewer concerns or hesitancies regarding the vaccine.
Data analysis
The analysis of data was conducted in two steps. First, we conducted a latent profile analysis (LPA) to identify subgroups of the COVID-19 vaccine KAPC patterns. Second, the association between the typology of KAPC and vaccine injection was measured by logistic regression analysis. Also, the scores of KAPC were compared by one-way analysis of variance (ANOVA) and Bonferroni post hoc test. In addition, the chi-square was performed to examine the typology of the relationship between KAPC and gender.
To identify the optimal typology of KAPC by LPA, we used an iterative approach with an increasing number of profiles. The KAPC subscales were converted to z-scores for ease of interpretation. The analysis started with a 2-profile model, gradually increasing successive models until the model was no longer interpretable. Fit was assessed using the Akaike information criterion (AIC), Bayesian information criterion (BIC), sample size adjusted Bayesian information criterion (aBIC), Lo–Mendell–Rubin likelihood ratio test (LMR-LRT), and Vuong-Lo–Mendell–Rubin likelihood ratio test (VLMR-LRT) [21]. Low BIC, AIC, and aBIC values show a better model fit. Nylund et al., in a simulation study, showed that aBIC is a superior index compared to BIC and AIC. A significant LMR-LRT and VLMR-LRT indicate that the latent profile model with k profiles was better than the simpler k - 1 profile model [22].
Furthermore, the entropy value (0–1) was considered to assess the quality of the classification of individuals into profiles, and values closer to 1 showed a more desirable classification [23]. LPA was performed using Mplus software, version 8.3, and ANOVA and logistic regression were performed by STATA software, version 16.
Results
A total of 413 (189 male and 224 female) medical science students from various fields participated in the study (Table 1).
The Mean±SD age of students was 22.4±2.5 years (ranges 18 to 38).
A series of 2 to 5 latent profile models were estimated based on the KAPC scales (Table 2).
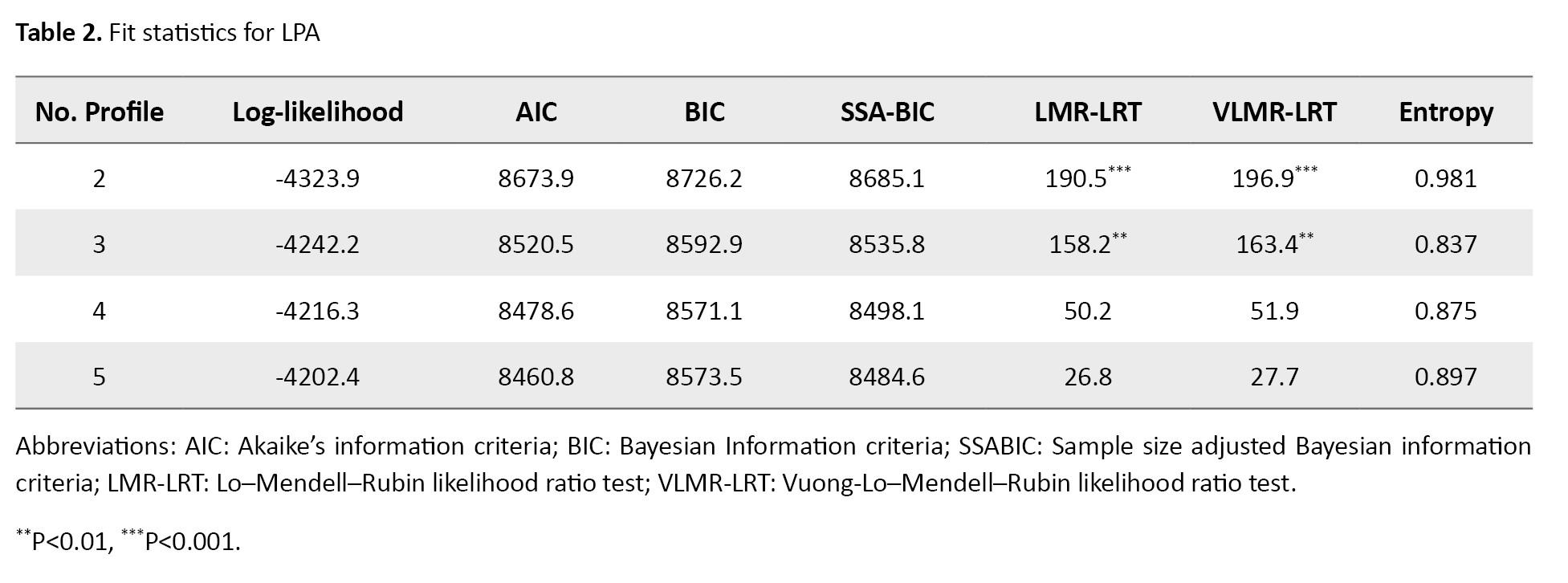
The AIC, BIC, and a-BIC had a decreasing trend with the increase in the number of profile models, and they never reached a minimum value, so they did not identify the best-fitting model. However, the LMR-LRT and VLMR-LRT were favored for the 3-profile model as the greatest number of profiles for which the P of the test was significant. The nonsignificant P for the 3-profile model indicated that a 4-profile model would not improve model fit over a 3-profile model. The entropy values were high for all the latent profile models, although they were highest for the 2-profile model.
Considering both fit indices and substantive interpretation, the 3-profile model was selected as the preferred model. Figure 1 shows the latent indicator means for the 3-profile model. As shown in Figure 1, Profile 1 (70.5% of the sample, n=291) w::as char::acterized by low moderate to up for KAPC scales and was labeled as “moderate to up for KAPC.” Profile 2 (25.4% of the sample, n=105) w::as char::acterized by high knowledge, attitude, practices, and low concerns scales and was labeled as “high KAP & low C.” Profile 3 (4.1% of the sample, n=17) w::as char::acterized by moderate knowledge, low attitude, practices, and high concerns, and was labeled as “moderate K & low AP & high C.”
Also, the mean scores of the COVID-19 vaccine KAPC scales are compared within- profiles and presented in Table 3.
The associations of the COVID-19 vaccine KAPC typologies with vaccine injection by logistic regression are given in Table 4.
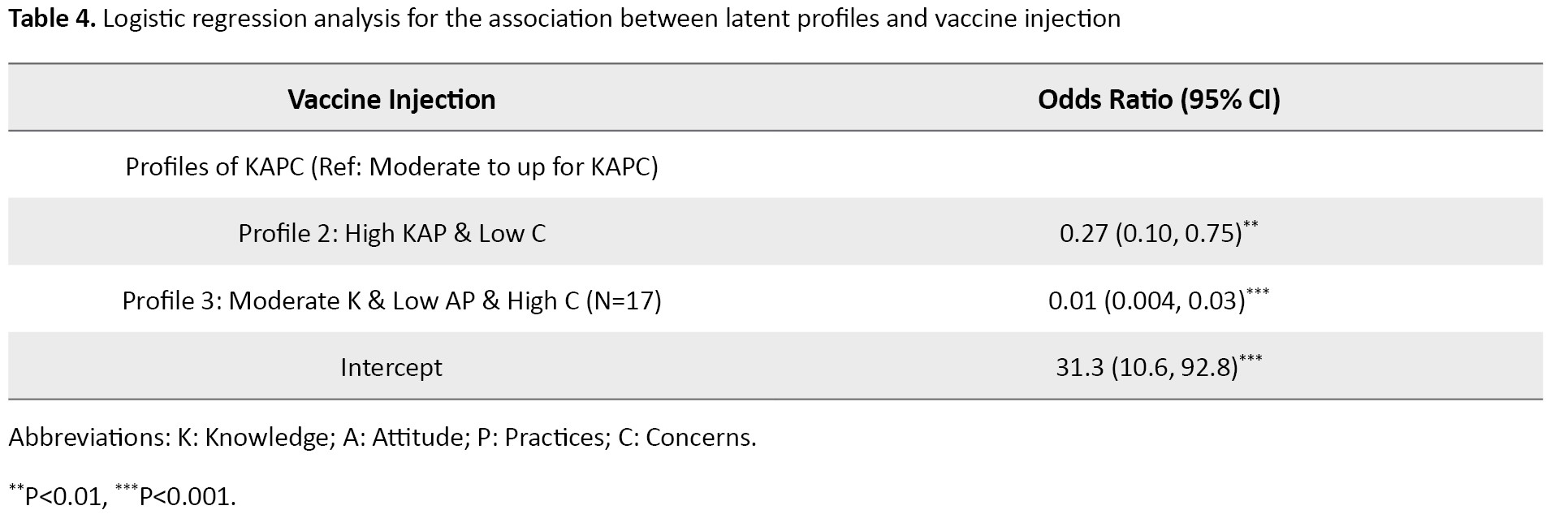
The individuals with membership in profile 2 relative to profile 1 have 73% less odds of injecting the vaccine. Also, individuals with membership in profile 3 relative to profile 1 have 99% less odds of injecting the vaccine.
Discussion
The current study showed three profiles (patterns) of the COVID-19 vaccine KAPC. These patterns included “moderate to up for KAPC,” “high KAP & low C,” and “moderate K & low AP & high C.” Students in the three profiles differed significantly in their KAPC factors. In other words, important heterogeneity or diversity of KAPC factors among students provides posterior probabilities of each individual’s membership in each profile. The most common pattern was “moderate to high for KAPC,” which included 70% of the study population, while the lowest pattern was “moderate K & low AP & high C,” with 4% of the study population.
Profile 3 was especially characterized by a very negative attitude towards COVID-19. Profile 3’s knowledge was almost similar but lower than that of the other two profiles. In addition, profile 3 had the highest value regarding the level of concern compared to profile 1. However, one of the characteristics of profile 2 was their highest level of knowledge, practices, and attitude. Profile 1 had a moderate attitude, knowledge, practices, and concern. The results showed that profile 3 had a 99% lower chance of vaccination than group 1. Moreover, the chance of vaccination in profile 2 was 63% lower than in profile 1.
Numerous studies have been performed on different strata of the medical staff, from physicians, nurses, dentists, and public health specialists, indicating an appropriate level of knowledge and attitude toward COVID-19 [24-27]. However, in the current study, participants were categorized according to knowledge, attitudes, and practices related to COVID-19. Classifying individuals in homogeneous groups can help create interventions for increasing the tendency to accept and subsequently for injection vaccines. Interventions should be comprehensive and specific to the target population. Intervenors should apply appropriate strategies for the best combination of interventions based on the typology.
As mentioned, profile 1, with a medium to a high level in terms of KAPC, is more inclined to receive vaccines than the others. Therefore, an average KAPC about COVID-19 increases the chance of receiving the vaccine. These findings are consistent with a previous study in Korea, which showed that individuals’ knowledge of COVID-19 and their concern and attitudes toward preventive measures can affect their performance concerning vaccination [28]. The finding is reasonable because high KAP leads to low concerns and vaccine acceptance.
Knowledge is a prerequisite for creating prevention beliefs, forming a positive attitude, and promoting positive behaviors, and people’s knowledge and attitude toward the disease can affect their coping strategies and behaviors [29]. Naturally, the audience of the present study (medical students) is expected to have an acceptable knowledge of COVID-19 and its vaccine. Also, various training sources at different levels, from university to society, have increased their knowledge about this epidemic, and usually, increasing knowledge leads to a change in people’s attitudes and consequently changes their practice [30].
Another studied component is attitude. It is influenced by knowledge, which can be obtained through experience [31]. Attitude in social psychology is evaluating a subject, which varies from negative to very positive [32]. Each person’s complex and unique psychological structure is acquired through individual experience and modeling. Attitude combines beliefs and emotions to evaluate different concepts in different ways and predict future behaviors [33]. According to the theory of planned behavior, attitude plays a vital role in health care behaviors [34], such as having a better function and receiving the vaccine because they feel optimistic about dealing with COVID-19, socially and individually.
Another component is concerns, which occur when a stimulus or event threatens our physical, mental, or social health. Thus, concerns and fear have an external source as a common emotion to increase energy to preserve life [35, 36]. The fear and concern about the recurrence of the disease persist even after treatment. COVID-19 concern means anxiety about being infected due to anonymity and cognitive ambiguity [37]. A moderate level of concern and anxiety creates the motivation to pursue treatment and seek prevention.
Therefore, students should have a reasonable understanding of what behaviors are appropriate for the prevention and control of COVID-19 disease (awareness and knowledge). This knowledge benefits their attitude and practice [38] to promote their health and show a greater willingness to be vaccinated for improvement. According to profile 1, acceptable knowledge about COVID-19 changes attitudes, and moderate attitude and concern affect the practice and, consequently, the desire to receive the COVID-19 vaccine.
Conclusion
This study divided individuals into three categories according to KAPC about COVID-19. The relationships between these categories and the receiving COVID-19 vaccine were found to be significant. These patterns of KAPC have various distributions in vaccine injection and even in controlling the pandemic. It seems that governmental authorities should take measures to improve the knowledge, attitude, and practice of the people appropriate to each profile and identify any obstacles to their promotion.
Study limitations
The current study has several limitations. First, knowledge and attitude in epidemic conditions are unstable. However, our study showed that the knowledge and attitude for participation during data collection was stable (Appendix 2). Second, the survey was conducted online, so respondents may not represent all medical sciences students. Third, this study’s population was medical students, so the generalizability of these findings to other population subgroups is with caution. Finally, the study design was cross-sectional, and the extracted profiles of KPAC were extracted simultaneously. Some ambiguities, such as “Is there change between latent profiles across time? If so, how can this change be characterized?” Need to be addressed in future research by longitudinal study design.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics in Research Committee of Mazandaran University of Medical Sciences, Sari, Iran (Code: IR.MAZUMS.REC.1400.335). The inquired data were anonymous and unidentifiable. Informed consent was obtained from all participants, and all methods were followed, following the relevant guidelines and regulations.
Funding
This study was supported by Mazandaran University of Medical Sciences, Sari, Iran (Code: 10283).
Authors contributions
Conceptualization, visualization, and funding acquisition: Zeinab Solimani and Maysam Rezapour; Data curation, writing the original draft: Zeinab Solimani and Hamed Mahmoodi; Supervision, formal analysis, methodology, project administration, and software: Maysam Rezapour; Investigation and validation: Zeinab Solimani and Hadis Amiri; Resources: Hamed Mahmoodi and Hadis Amiri; Review, and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank all participants in this study and the Student Research Committee (SRC) of Mazandaran University of Medical Sciences, Sari, Iran.
References
- Tang X, Wu C, Li X, Song Y, Yao X, Wu X, et al. On the origin and continuing evolution of SARS-CoV-2. National Science Review. 2020; 7(6):1012-23. [PMID]
- Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). International Journal of Surgery. 2020; 76:71-6. [DOI:10.1016/j.ijsu.2020.02.034] [PMID]
- Huang Y, Yang ZY, Kong WP, Nabel GJ. Generation of synthetic severe acute respiratory syndrome coronavirus pseudoparticles: Implications for assembly and vaccine production. Journal of Virology. 2004; 78(22):12557-65. [DOI:10.1128/JVI.78.22.12557-12565.2004] [PMID]
- Khan ZA, Allana R, Afzal I, Ali AS, Mariam O, Aslam R, et al. Assessment of attitude and hesitancy toward vaccine against COVID-19 in a Pakistani population: A mix methods survey. Vacunas. 2022; 23:S26-32. [DOI:10.1016/j.vacun.2021.08.002] [PMID]
- Latkin CA, Dayton L, Yi G, Konstantopoulos A, Boodram B. Trust in a COVID-19 vaccine in the US: A social-ecological perspective. Social Science & Medicine (1982). 2021; 270:113684. [DOI:10.1016/j.socscimed.2021.113684] [PMID]
- Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. European Journal of Epidemiology. 2020; 35(4):325-30. [DOI:10.1007/s10654-020-00634-3] [PMID]
- MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015; 33(34):4161-4. [DOI:10.1016/j.vaccine.2015.04.036] [PMID]
- Karafillakis E, Larson HJ; ADVANCE consortium. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017; 35(37):4840-50. [DOI:10.1016/j.vaccine.2017.07.061] [PMID]
- Cobos Muñoz D, Monzón Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low-and middle-income countries: A systematic review. International Journal of Public Health. 2015; 60(7):767-80. [DOI:10.1007/s00038-015-0715-6] [PMID]
- Kennedy J. Vaccine hesitancy: A growing concern. Paediatric Drugs. 2020; 22(2):105-11. [DOI:10.1007/s40272-020-00385-4] [PMID]
- Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007-2012. Vaccine. 2014; 32(19):2150-9. [DOI:10.1016/j.vaccine.2014.01.081] [PMID]
- Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015-2017. Vaccine. 2018; 36(26):3861-7. [DOI:10.1016/j.vaccine.2018.03.063] [PMID]
- Dubé E, MacDonald NE. How can a global pandemic affect vaccine hesitancy? Expert Review of Vaccines. 2020; 19(10):899-901. [DOI:10.1080/14760584.2020.1825944] [PMID]
- Silva TM, Estrela M, Roque V, Gomes ER, Figueiras A, Roque F, et al. Perceptions, knowledge and attitudes about COVID-19 vaccine hesitancy in older Portuguese adults. Age and Ageing. 2022; 51(3):afac013. [DOI:10.1093/ageing/afac013] [PMID]
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine. 2021; 27(2):225-8. [DOI:10.1038/s41591-020-1124-9]
- Sengupta M, Dutta S, Roy A, Chakrabarti S, Mukhopadhyay I. Knowledge, attitude and practice survey towards COVID-19 vaccination: A mediation analysis. The International Journal of Health Planning and Management. 2022; 37(4):2063-80. [DOI:10.1002/hpm.3449] [PMID]
- Al Awaidy ST, Khatiwada M, Castillo S, Al Siyabi H, Al Siyabi A, Al Mukhaini S, et al. Knowledge, attitude, and acceptability of covid-19 vaccine in Oman: A Cross-sectional Study. Oman Medical Journal. 2022; 37(3):e380. [PMID]
- Rhead R, Elliot M, Upham P. Using latent class analysis to produce a typology of environmental concern in the UK. Social Science Research. 2018; 74:210-22. [DOI:10.1016/j.ssresearch.2018.06.001] [PMID]
- Kumari A, Ranjan P, Chopra S, Kaur D, Upadhyay AD, Kaur T, et al. Development and validation of a questionnaire to assess knowledge, attitude, practices, and concerns regarding COVID-19 vaccination among the general population. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2021; 15(3):919-25. [DOI:10.1016/j.dsx.2021.04.004] [PMID]
- Watkins MW. Exploratory factor analysis: A guide to best practice. Journal of Black Psychology. 2018; 44(3):219-46. [DOI:10.1177/0095798418771807]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001; 88(3):767-78. [DOI:10.1093/biomet/88.3.767]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007; 14(4):535-69. [DOI:10.1080/10705510701575396]
- Finch WH, Bronk KC. Conducting confirmatory latent class analysis using mplus. Structural Equation Modeling: A Multidisciplinary Journal. 2011; 18(1):132-51. [DOI:10.1080/10705511.2011.532732]
- Zhang M, Zhou M, Tang F, Wang Y, Nie H, Zhang L, et al. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. Journal of Hospital Infection. 2020; 105(2):183-7. [DOI:10.1016/j.jhin.2020.04.012] [PMID]
- Shi Y, Wang J, Yang Y, Wang Z, Wang G, Hashimoto K, et al. Knowledge and attitudes of medical staff in Chinese psychiatric hospitals regarding COVID-19. Brain, Behavior, & Immunity-Health. 2020; 4:100064. [DOI:10.1016/j.bbih.2020.100064] [PMID]
- Kamate SK, Sharma S, Thakar S, Srivastava D, Sengupta K, Hadi AJ, et al. Assessing knowledge, attitudes and practices of dental practitioners regarding the covid-19 pandemic: A multinational study. Dental and Medical Problems. 2020; 57(1):11-7. [DOI:10.17219/dmp/119743] [PMID]
- Vickers NJ. Animal communication: When i’m calling you, will you answer too? Current Biology. 2017; 27(14):R713-5. [DOI:10.1016/j.cub.2017.05.064] [PMID]
- Lee M, Kang BA, You M. Association between knowledge, attitudes and practices (KAP) towards the covid-19: A cross-sectional study in South Korea [Preprint]. 2020. [DOI:10.21203/rs.3.rs-73653/v1]
- AlAmodi AA, Al-Kattan K, Shareef MA. The current global perspective of the knowledge-attitude-behavior of the general public towards the corona virus disease -19 pandemic: Systematic review and meta-analysis on 67,143 participants. Plos One. 2021; 16(12):e0260240. [DOI:10.1371/journal.pone.0260240] [PMID]
- Arcury T. Environmental attitude and environmental knowledge. Human organization. 1990; 49(4):300-4. [DOI:10.17730/humo.49.4.y6135676n433r880]
- Perloff RM. The dynamics of persuasion: Communication and attitudes in the twenty-first century. New York: Routledge; 2020. [DOI:10.4324/9780429196959]
- Minson JA, Dorison CA. Toward a psychology of attitude conflict. Current Opinion in Psychology. 2022; 43:182-8. [DOI:10.1016/j.copsyc.2021.07.002] [PMID]
- Rucker DD. Attitudes and attitude strength as precursors to object attachment. Current Opinion in Psychology. 2021; 39:38-42. [DOI:10.1016/j.copsyc.2020.07.009] [PMID]
- Gibson LP, Magnan RE, Kramer EB, Bryan AD. Theory of planned behavior analysis of social distancing during the COVID-19 pandemic: Focusing on the intention-behavior gap. Annals of Behavioral Medicine. 2021; 55(8):805-12. [DOI:10.1093/abm/kaab041] [PMID]
- Fillenbaum GG, Blay SL, Mello MF, Quintana MI, Mari JJ, Bressan RA, et al. Use of mental health services by community-resident adults with DSM-IV anxiety and mood disorders in a violence-prone area: Sao Paulo, Brazil. Journal of Affective Disorders. 2019; 250:145-52. [DOI:10.1016/j.jad.2019.03.010] [PMID]
- Melnyk BM. Reducing healthcare costs for mental health hospitalizations with the evidence-based COPE program for child and adolescent depression and anxiety: A cost analysis. Journal of Pediatric Health Care. 2020; 34(2):117-21. [DOI:10.1016/j.pedhc.2019.08.002] [PMID]
- Alipour A, Ghadami A, Alipour Z, Abdollahzadeh H. [Preliminary validation of the Corona Disease Anxiety Scale (CDAS) in the Iranian sample (Persian)]. Quarterly Journal of Health Psychology. 2020; 8(32):163-75. [DOI:10.30473/hpj.2020.52023.4756]
- McKenzie JF, Neiger BL, Thackeray R. Planning, implementing, and evaluating health promotion programs : A Primer. New Jersey: Pearson; 2017. [Link]
Type of Study: Original Article |
Subject:
Epidemiology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |