Volume 11, Issue 2 (Spring 2023)
Iran J Health Sci 2023, 11(2): 127-136 |
Back to browse issues page
Ethics code: 261399
Clinical trials code: 261399
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahmoudi Sefidkouhi H, Najafi E, Haji A, Arasteh A. Identification and Introduction of a New Classification of Key Performance Shaping Factors in Staff Performance in the Healthcare System. Iran J Health Sci 2023; 11 (2) :127-136
URL: http://jhs.mazums.ac.ir/article-1-853-en.html
URL: http://jhs.mazums.ac.ir/article-1-853-en.html
Department of Industrial Engineering, Faculty of Industrial Engineering, Science and Research Branch, Islamic Azad University, Tehran, Iran. , esmaeilnajafi1400@gmail.com
Keywords: Healthcare system, Safety management, Classification, Employee performance appraisal, Risk management
Full-Text [PDF 1234 kb]
(1002 Downloads)
| Abstract (HTML) (2382 Views)
Full-Text: (979 Views)
1. Introduction
Different studies demonstrate that errors and incidents emerge in the healthcare (hospital) system mainly during the diagnosis of diseases, prescription of medications, anesthesiology, intensive care, emergency, operating room, radiology, clinical experimentation, radiotherapy, and medical equipment, where the human factor alone is responsible for the emergence of 70% of undesirable incidents [1]. Alarming reports of mistakes are extensively reflected every day in the press and mass media, including the patient’s mistaken transfer to the operating room, surgery performed on the wrong organ, excessive administration of chemotherapy, improper organ transplantation, a surgical object left inside the patient’s body, etc. In the United States, the annual mortality due to medical errors amounts to 44000 to 98000 [2]. Since not all medical errors lead to death, the number of errors must be several times the mortality [3]. All around the world, the statistics indicate sustainable improvements in the safety of the healthcare system in recent years. Despite these constant improvements, there is still a high rate of errors in the system, leading to unpleasant and irreparable incidents every year. Research has been conducted in the nuclear, petrochemical, aviation, and railway industries to analyze errors and present the performance shaping factors (PSFs), which is inappropriate and hardly applicable to healthcare, as it fails to consider all healthcare aspects to obtain highly accurate results. Therefore, it can significantly improve the healthcare system safety by performing a comprehensive study and analysis of errors and incidents that arise and presenting the performance-shaping factors particular to that entire system.
Comprehensive research that considers the healthcare system as coherent and integrated and introduces its PSFs has not been done, and this issue is a research gap in the field under investigation. To cover the research-mentioned gap, we conducted this study. The importance of this issue is that it can be a road map for the managers of the healthcare system in formulating a general and comprehensive policy of the healthcare system for decision-making.
Several studies have been conducted to analyze the emergence of errors and incidents or human reliability and present the relevant PSF sets in industries other than healthcare [2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]. There are also comprehensive studies regardless of specific industries, including an approach presented to investigate human reliability analysis given the dependency between human errors [15] and an assessment of human reliability in theory and practice [16]. Also, several studies have been conducted in the healthcare field on the analysis of errors and incidents and human reliability analysis, medical errors management before and after implementation of accreditation in hospitals [17], investigation of the role of patients in the provision of safety and occurrence of medical errors, analysis of medication errors and presentation of approaches to their mitigation [18], a taxonomy of human-induced medical errors [19], presentation of the most significant PSFs concerning the operating room [20], consideration of several PSFs in the aviation industry as ones in the healthcare and their validation [21], human reliability analysis for laparoscopic rectal cancer surgery [22], and investigation of common errors in medication
Chana et al. investigated the relationship between healthcare worker and patient health and safety [23]. Faiella et al. used the healthcare failure mode and effect analysis for mitigation of human errors [24]. Abbaspour et al. specified the optimal method of human reliability analysis in health care systems using fuzzy ANP and fuzzy TOPSIS (Technique for Order Preference by Similarity to Ideal Solution) [1]. Also, some studies assessed the human reliability in patients COVID-19 [25] and in health care workers during the COVID-19 pandemic [26]. Some of the stated studies apply solely to the industry where they were created. Some have wrongly considered just tiny elements of the system. This study proposes a new, complete, suitable taxonomy of performance shaping factors (H-PSF) for the whole healthcare system, including mistakes other than those committed by system personnel and their causes.
Therefore, the most important difference between this research and other research studies is providing specialized PSFs for the healthcare system and considering the entire healthcare system as a coherent and integrated whole.
The major assumption for extracting H-PSFs in this work was that only mistakes and events from the patient’s (or their family’s) hospitalization till discharge counted. For a complete and acceptable PSF set for the healthcare business, additional PSF studies were explored. Using the Delphi technique, 10 healthcare specialists and 10 human reliability experts were consulted on the consistency of PSFs in healthcare and the inclusion of specific ones. The inquiry and expert consultation selected 43 H-PSFs in 8 key classes. The 8 key classes and their H-PSFs are as follows:
1. Static personal factors include any factor that affects individuals’ performance with little association with the exact time of the incident. The H-PSFs of this class are provided here.
• Experience: Defined as a series of emotional effects recorded in an individual’s mind during or after an incident. It is described as information and knowledge accumulated due to teaching and interaction with the system.
• Familiarity: Defined as an individual’s proper knowledge and information in a particular area relevant to their duties. It may overlap experience, but there is a clear distinction between the two.
• Fit for the job: Defined as an individual’s ability to perform their tasks safely, confidently, and efficiently without being confronted with physical or mental health problems.
• Motivation: Motives are a series of factors that cause an individual to behave or attempt in a particular way and achieve the intended purposes.
• Individual characteristics: Individual characteristics include age, gender, physical capabilities, and cultural and behavioral traits, etc., such as extraversion and introversion.
2. Dynamic personal factors include any factor that affects individuals’ performance in close association with the exact time of the incident or a short while beforehand. The H-PSFs of this class are provided below.
• Distraction: Distraction is a loss of concentration for any internal or external reason. Distraction means diversion from the ordinary procedure of performing a task and daydreaming or performing other tasks.
• Perception: Perception is the process of identifying and obtaining sensory information. It is an individual’s ability to recognize any external phenomenon or object using the five senses.
• Interpretation: Interpretation is an individual’s ability to explain the meaning of information to themselves.
• Stress: When the requirements of activity lie beyond an individual’s personal and social capabilities, or they are in undesirable environmental conditions, responses are provided that are referred to as stress.
• Fatigue: Fatigue refers to physical fatigue arising from long-term activity. Fatigue is a prevalent signal for those who perform their duties in shifts or work in emergency conditions with insufficient rest.
• Vigilance: Vigilance is closely associated with feelings of physical and mental fatigue and monotony. Loss of vigilance may occur when an individual is engaged in a monotonous, repetitive activity for a long while.
• Decision-making skills: Decision-making skills are defined as an individual’s ability, based on their knowledge and experience, to make the best decision at the right time from among several alternatives.
• Precaution: Precaution is necessary to avoid definite or probable risk, even in cases with no scientific or technical confidence that specific measures are harmful.
• Self-confidence: Self-confidence is a mental condition where the individual relies on and believes in their capabilities and talents to successfully perform tasks due to previous experience.
• Management of experience: Not only inexperienced individuals but also experienced ones are prone to errors. Therefore, the aspects of management of experience should be considered, as the experience itself, to prevent experienced individuals’ errors. Management of experience is sub-classified as a dynamic individual factor.
3. Task factors concern the elements of tasks and their methods of performance by individuals. Any incident due to task features and performance methods is classified as a task factor. The H-PSFs of this class are resented here.
• Workload: Defined as the amount of work an individual performs within a specific period. It can be physical or mental, depending on the type of work.
• Monotony: Described as lack of variety and tedious repetition of a task, leading to a feeling of monotony, loss of interest, lack of consciousness, and lack of precaution in the individuals involved in the task.
• Time pressure: Defined as the time available for performing a task from a specific task process. This PSF can negatively affect others, particularly stress, consciousness, experience management, perception, and interpretation.
• Task complexity: Concerns about how a specific task is performed. It should be noted that this PSF addresses the complexity of a particular task in a process rather than that of the process as a whole.
• Task instructions: Commands or rules established to guide or support individuals in the process of performing a duty or task. Incomplete or defective instructions sometimes cause incidents.
4. Team factors concern the performance of individuals as team members who interact to achieve a common purpose and the final consequence of all team members’ collaboration. The H-PSFs of this class are presented below.
• Communication between employees (CBE): It denotes individuals’ ability to exchange information via verbal and nonverbal media. The quick, clear, justified, and approved exchange indicates efficient communication.
• Teamwork: It is described as a clear division of roles and responsibilities upon the performance of a task. The definition also includes the quality of feedback among team members, level of trust, team structure and stability, consideration of team members’ needs and support, and mutually respectful behavior.
5. Organizational factors include any factors defined and controlled by an organization. These factors concern organizational features, attitudes, and behaviors affecting staff performance. The H-PSFs of this class are presented here.
• Safety culture: It denotes what is developed due to organizational effort to transfer all cultural elements to bring about safety for organization members, systems, and professional activities. It involves a series of values and priorities specified for all safety aspects by the entire staff at any level of the organization.
• Safety management systems (SMS): It concerns the set of methods and instructions devised for supervision and improvement, if needed, of operational safety.
• Training: It is defined as a constant process an organization provides to the staff to ensure they hold the appropriate knowledge, skills, and perspectives by the set standards.
• Quality and availability of the procedures, standards, and regulations (QA-PSR): It concerns the existence and application of official operating methods for the intended duties. A high-quality procedure is characterized by clarity, simplicity, and availability, given its strategy of description.
• Leadership: Leaders help themselves and others to do the right thing. They specify the route to achieve the purposes, generate an inspiring perspective, provide new ways to improve the conditions of the organization, and identify what the team or organization needs to succeed.
• Supervision: It is defined as applying management, development, and support to the staff.
• Shift pattern: It consists of working hours different from the routine working period, sometimes including irregular working hours.
• Relations within an organization: It indicates the social atmosphere among all the organization members and their interactions at different hierarchy levels.
• Incentives for employees: Incentives are tools organizations use to increase the staff’s motivation to perform their activities and tasks. The staff’s incentives are strongly correlated with their motivation.
6. System factors include any factors that specify the healthcare system features and the quality of individuals’ interaction with them that may affect their performance. The H-PSFs of this class are presented below.
• System design: It is described as achieving high quality and optimal efficiency in terms of components, modules, interfaces, and data to meet specific predetermined requirements of the system.
• Human-machine interface (HMI): It addresses how information is communicated among operators and equipment and assessed based on the clarity and validity of the information obtained by the equipment and its performance.
• Equipment: It includes everything associated with the equipment, such as performance, precision, shortage, and breakdown.
• Workplace: It includes everything associated with the equipment, such as performance, precision, shortage, and breakdown.
• Trust in equipment: It is described the extent to which operators trust the information output by particular equipment. Trust is affected by factors such as the duration of application, history of failure, and equipment reliability.
• Communication systems: It involves facilities consisting of physical units and equipment for the propagation of information among the staff.
• Similarity: It includes cases where errors occur due to the similarity between names, symptoms, etc.
7. Environmental factors include any factor outside the healthcare organization and over which there can be no control, such as weather conditions and third parties. The H-PSFs of this class are presented here.
• Weather conditions: Describe the atmospheric conditions each day, expressed in temperature, wind, cloud, precipitation, etc.
• Third parties: It concerns cases where individuals outside the organization cause an incident.
• Urban design: It concerns urban street conditions in terms of traffic, fitness (particularly for streets ending in hospitals), traffic lights, speed bumps, etc., and may cause errors in some instances.
8. Factors associated with the patient include any factor particular to the healthcare field, not applicable to others, involving those concerning the patient, one for the patient and one for their companion. The H-PSFs of this class are presented here.
• Patient: It is considered if an incident arises where the patient himself/herself plays a role.
• Patient’s companion: It is considered if an incident arises where the patient’s companion or family plays a role.
2. Materials and Methods
A total of 318 complaints of medical mistakes from March 2020 to March 2021 at 17 hospitals in Iran were analyzed for the planned H-PSFs. With and without repeats, the number of H-PSFs activations was assessed. These 17 hospitals were chosen because they gave the Health Ministry detailed descriptions of mistakes and occurrences that occurred over the time described above, including all the variables and personnel involved, reasons, etc. In the mode with repetition, a given H-PSF might be considered more than once in a medical mistake or event report. In the approach without repetition, a given H-PSF might be evaluated just once in a medical mistake or event report, even if the error was repeated. Also, this article’s graphs and statistical analysis results were obtained using Minitab software.
3. Result
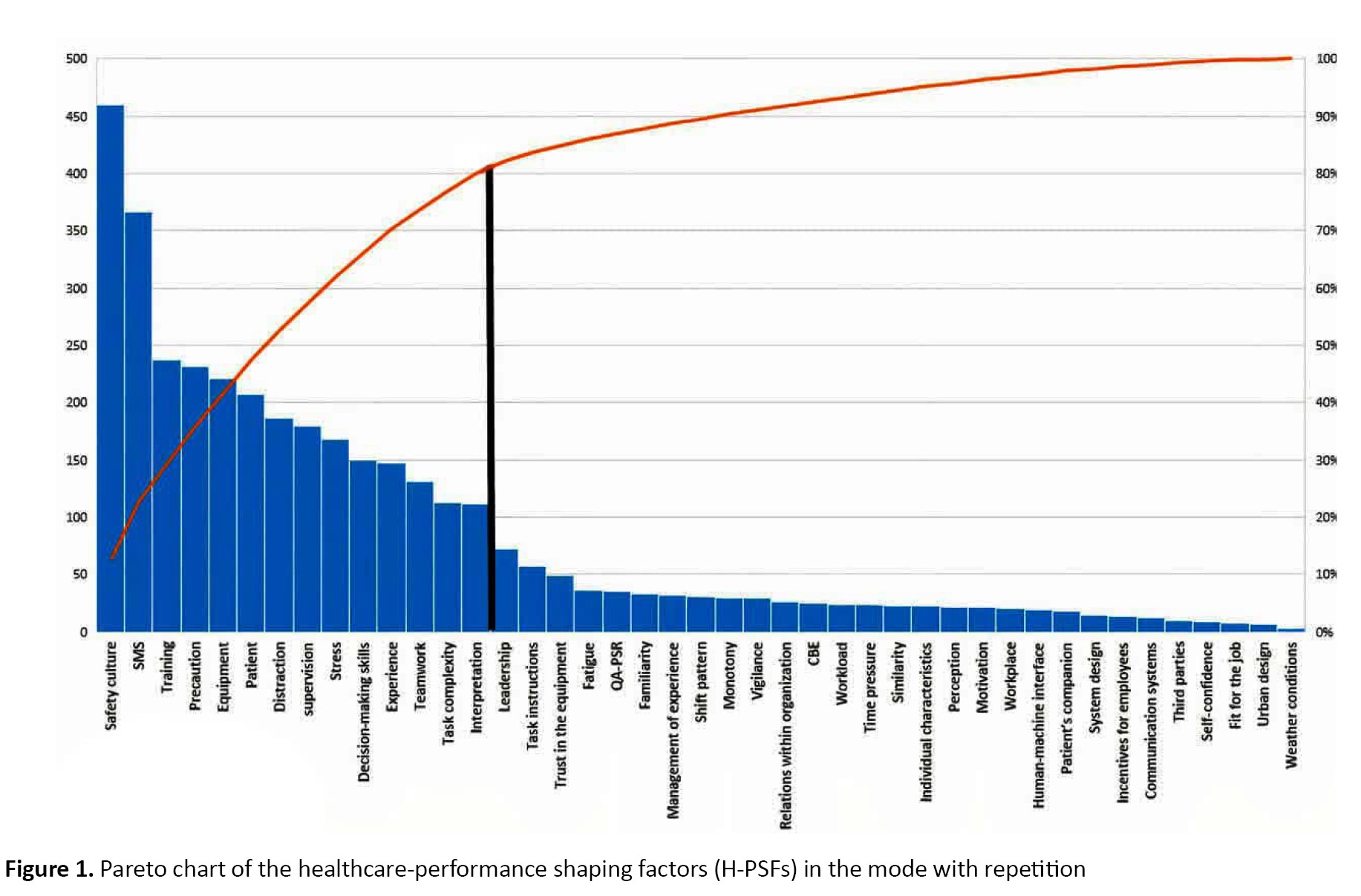
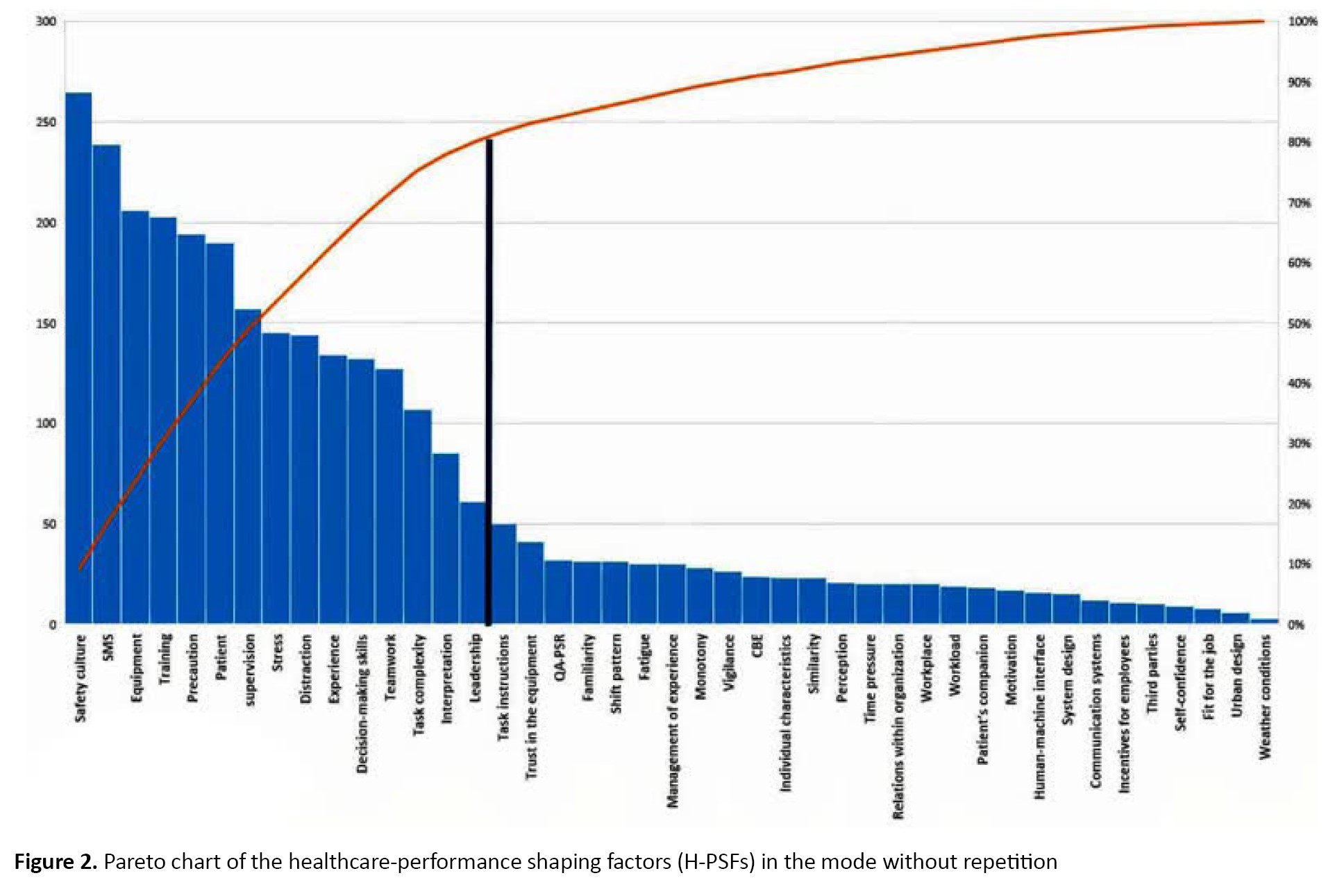
Table 1 presents 318 medical mistake findings.
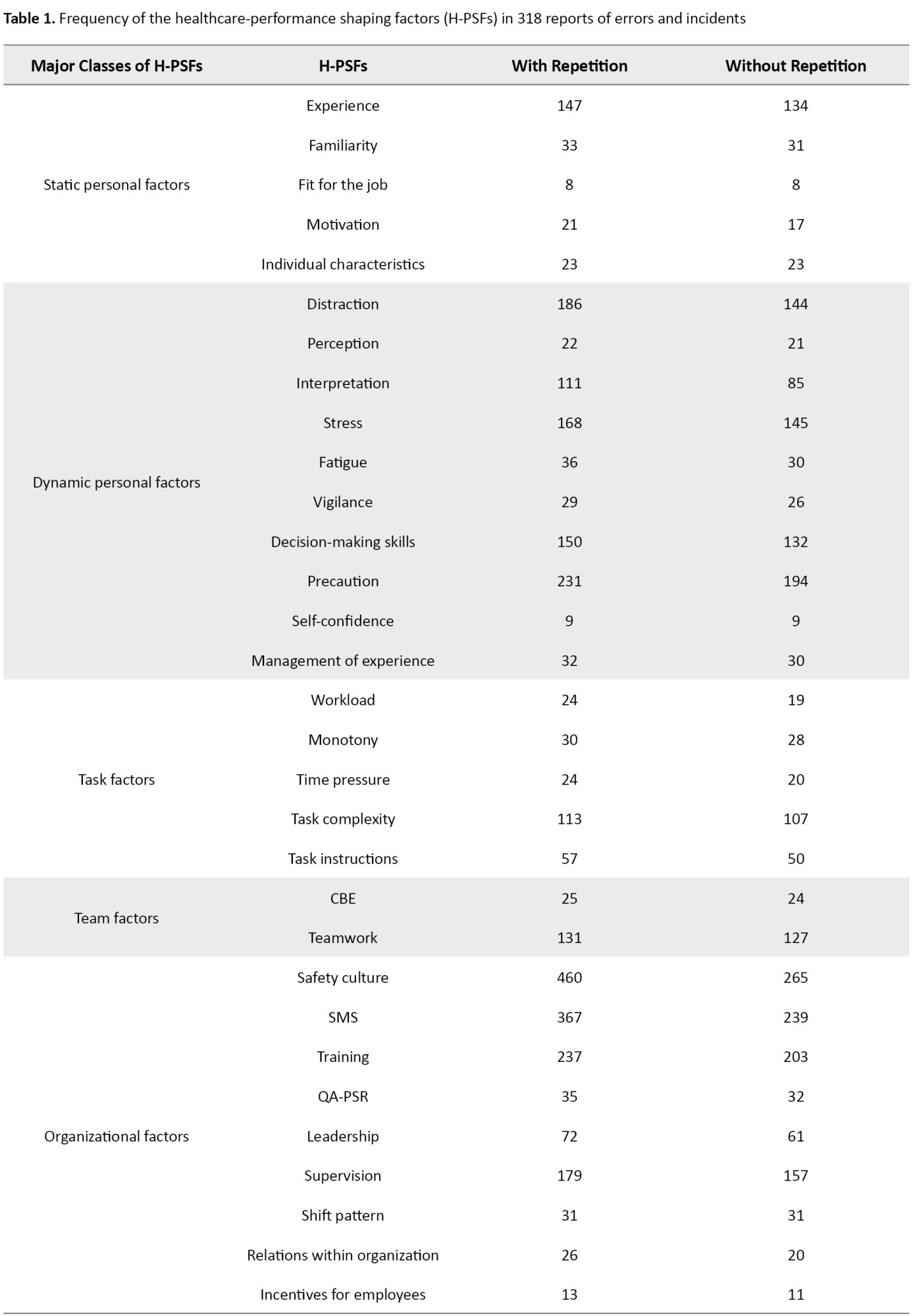
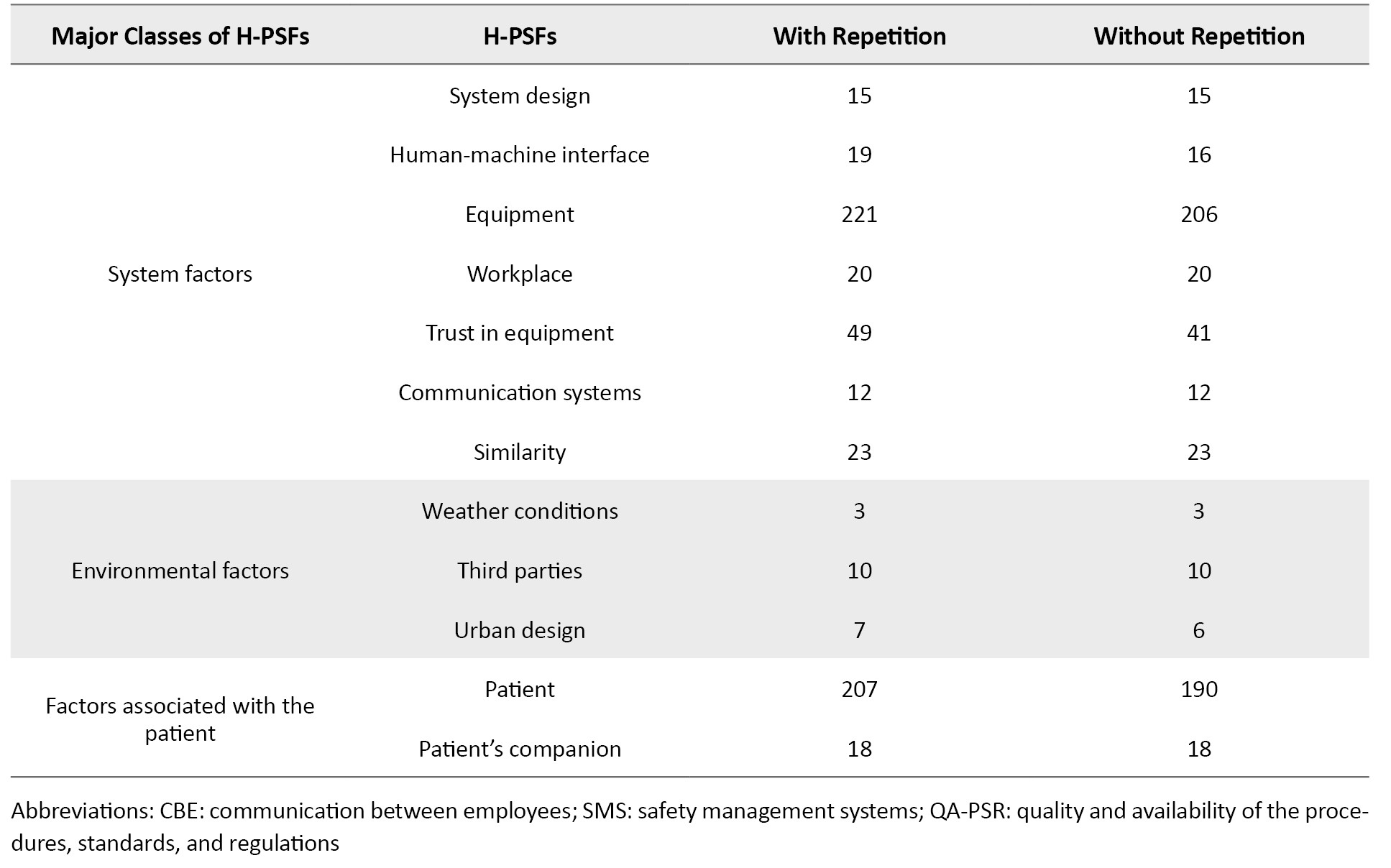
Figures 1 and 2 illustrate the H-PSF Pareto charts based on Table 1 for modes with and without repetition. Based on Figure 1, 14 H-PSFs led to 80% of mistakes or accidents. Figure 2 shows that 15 H-PSFs led to mistakes or occurrences. The Pareto charts show that focusing on a few H-PSFs may reduce healthcare mistakes and occurrences. The taxonomy of H-PSFs may help healthcare management reduce mistakes and occurrences.
With the help of H-PSFs classification, healthcare system managers can make better decisions in formulating general and comprehensive policies and policies to reduce errors and accidents.
To validate the proposed H-PSFs and their applications to health systems, we use the Chi-square goodness-of-fit test with the help of Minitab software. The null hypothesis and alternate hypothesis for this test are as follows:
H0: The results of the examination of the preliminary reports have good validity to be generalized to other healthcare systems.
H1: The results of the examination of the preliminary reports do not have good validity to be generalized to other healthcare systems. The type I error rate, α, was assumed to be 0.05.
For that purpose, 141 reports of medical errors that had occurred from March 21, 2021, to August 6, 2021, at 14 hospitals different from the primary 17 were examined as secondary reports, and the number of occurrences of each PSF in those reports was also extracted, where 1361 occurrences were identified in the way with repetition and 1190 in the mode without repetition. It should be noted that the reports were collected directly at the hospitals. The 14 hospitals were selected as they were different from the primary 17, for the results obtained from the goodness of fit test to be of greater validity.
In the mode with repetition, the Chi-square statistic was 40.8381. Since , there was no reason for rejection of the null hypothesis, which was therefore retained. In the mode without repetition, the value of the Chi-square statistic was 46.9218. Since , there was no reason for rejection of the null hypothesis, which was therefore retained. Thus, the findings in section 3 were validated by the results obtained from the goodness of fit test, and it can be said that the results of this article have enough validity to generalize the results to all healthcare systems.
4. Discussion
The emergence of medical errors and incidents is inevitable in healthcare. However, they affect people’s health as well as harm them financially. Therefore, it can significantly contribute to improving the conditions and minimizing these errors and incidents to analyze and investigate them and their causes. An appropriate approach to investigating errors and incidents in any area of expertise is to examine their causes, i.e. performance-shaping factors. For that purpose, a comprehensive, appropriate taxonomy was presented in this paper to explore the causes of errors and incidents in the healthcare field, i.e. introducing the shaping factors specific to the healthcare system, considering it as an integrated and coherent whole (H-PSF).
According to experts, 43 PSF were identified for the healthcare system. Using the medical error reports, the number of times that errors and mistakes were related to each of these 43 PSFs was calculated in two cases with and without repetition. To identify the most important PSFs, the Pareto principle has been used, and the results indicate that 14 H-PSFs in the non-repetitive mode and 15 H-PSFs in the repeated mode are responsible for the occurrence of errors.
5. Conclusion
Field managers can largely mitigate errors and incidents by considering these factors because the goodness of fit test was used to validate the proposed set of H-PSFs and examine its generalizability to all healthcare systems. The results demonstrated the great validity of the set to be generalized to similar systems.
Using the classification presented in this article, considering the healthcare system as an integrated whole to analyze human reliability is a suitable topic for future research.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and Supervision: Hossein Mahmoudi Sefidkouhi, Esmaeil Najafi, and Alireza Haji; Methodology: Hossein Mahmoudi Sefidkouhi; Investigation, Writing-original draft, and Writing-review & editing: All authors; Data collection: Hossein Mahmoudi Sefidkouhi; Data analysis: Hossein Mahmoudi Sefidkouhi and Abdollah Arasteh.
Conflict of interest
All authors declared no conflict of interest.
Acknowledgements
The authors appreciate all participants in the study.
References
Different studies demonstrate that errors and incidents emerge in the healthcare (hospital) system mainly during the diagnosis of diseases, prescription of medications, anesthesiology, intensive care, emergency, operating room, radiology, clinical experimentation, radiotherapy, and medical equipment, where the human factor alone is responsible for the emergence of 70% of undesirable incidents [1]. Alarming reports of mistakes are extensively reflected every day in the press and mass media, including the patient’s mistaken transfer to the operating room, surgery performed on the wrong organ, excessive administration of chemotherapy, improper organ transplantation, a surgical object left inside the patient’s body, etc. In the United States, the annual mortality due to medical errors amounts to 44000 to 98000 [2]. Since not all medical errors lead to death, the number of errors must be several times the mortality [3]. All around the world, the statistics indicate sustainable improvements in the safety of the healthcare system in recent years. Despite these constant improvements, there is still a high rate of errors in the system, leading to unpleasant and irreparable incidents every year. Research has been conducted in the nuclear, petrochemical, aviation, and railway industries to analyze errors and present the performance shaping factors (PSFs), which is inappropriate and hardly applicable to healthcare, as it fails to consider all healthcare aspects to obtain highly accurate results. Therefore, it can significantly improve the healthcare system safety by performing a comprehensive study and analysis of errors and incidents that arise and presenting the performance-shaping factors particular to that entire system.
Comprehensive research that considers the healthcare system as coherent and integrated and introduces its PSFs has not been done, and this issue is a research gap in the field under investigation. To cover the research-mentioned gap, we conducted this study. The importance of this issue is that it can be a road map for the managers of the healthcare system in formulating a general and comprehensive policy of the healthcare system for decision-making.
Several studies have been conducted to analyze the emergence of errors and incidents or human reliability and present the relevant PSF sets in industries other than healthcare [2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]. There are also comprehensive studies regardless of specific industries, including an approach presented to investigate human reliability analysis given the dependency between human errors [15] and an assessment of human reliability in theory and practice [16]. Also, several studies have been conducted in the healthcare field on the analysis of errors and incidents and human reliability analysis, medical errors management before and after implementation of accreditation in hospitals [17], investigation of the role of patients in the provision of safety and occurrence of medical errors, analysis of medication errors and presentation of approaches to their mitigation [18], a taxonomy of human-induced medical errors [19], presentation of the most significant PSFs concerning the operating room [20], consideration of several PSFs in the aviation industry as ones in the healthcare and their validation [21], human reliability analysis for laparoscopic rectal cancer surgery [22], and investigation of common errors in medication
Chana et al. investigated the relationship between healthcare worker and patient health and safety [23]. Faiella et al. used the healthcare failure mode and effect analysis for mitigation of human errors [24]. Abbaspour et al. specified the optimal method of human reliability analysis in health care systems using fuzzy ANP and fuzzy TOPSIS (Technique for Order Preference by Similarity to Ideal Solution) [1]. Also, some studies assessed the human reliability in patients COVID-19 [25] and in health care workers during the COVID-19 pandemic [26]. Some of the stated studies apply solely to the industry where they were created. Some have wrongly considered just tiny elements of the system. This study proposes a new, complete, suitable taxonomy of performance shaping factors (H-PSF) for the whole healthcare system, including mistakes other than those committed by system personnel and their causes.
Therefore, the most important difference between this research and other research studies is providing specialized PSFs for the healthcare system and considering the entire healthcare system as a coherent and integrated whole.
The major assumption for extracting H-PSFs in this work was that only mistakes and events from the patient’s (or their family’s) hospitalization till discharge counted. For a complete and acceptable PSF set for the healthcare business, additional PSF studies were explored. Using the Delphi technique, 10 healthcare specialists and 10 human reliability experts were consulted on the consistency of PSFs in healthcare and the inclusion of specific ones. The inquiry and expert consultation selected 43 H-PSFs in 8 key classes. The 8 key classes and their H-PSFs are as follows:
1. Static personal factors include any factor that affects individuals’ performance with little association with the exact time of the incident. The H-PSFs of this class are provided here.
• Experience: Defined as a series of emotional effects recorded in an individual’s mind during or after an incident. It is described as information and knowledge accumulated due to teaching and interaction with the system.
• Familiarity: Defined as an individual’s proper knowledge and information in a particular area relevant to their duties. It may overlap experience, but there is a clear distinction between the two.
• Fit for the job: Defined as an individual’s ability to perform their tasks safely, confidently, and efficiently without being confronted with physical or mental health problems.
• Motivation: Motives are a series of factors that cause an individual to behave or attempt in a particular way and achieve the intended purposes.
• Individual characteristics: Individual characteristics include age, gender, physical capabilities, and cultural and behavioral traits, etc., such as extraversion and introversion.
2. Dynamic personal factors include any factor that affects individuals’ performance in close association with the exact time of the incident or a short while beforehand. The H-PSFs of this class are provided below.
• Distraction: Distraction is a loss of concentration for any internal or external reason. Distraction means diversion from the ordinary procedure of performing a task and daydreaming or performing other tasks.
• Perception: Perception is the process of identifying and obtaining sensory information. It is an individual’s ability to recognize any external phenomenon or object using the five senses.
• Interpretation: Interpretation is an individual’s ability to explain the meaning of information to themselves.
• Stress: When the requirements of activity lie beyond an individual’s personal and social capabilities, or they are in undesirable environmental conditions, responses are provided that are referred to as stress.
• Fatigue: Fatigue refers to physical fatigue arising from long-term activity. Fatigue is a prevalent signal for those who perform their duties in shifts or work in emergency conditions with insufficient rest.
• Vigilance: Vigilance is closely associated with feelings of physical and mental fatigue and monotony. Loss of vigilance may occur when an individual is engaged in a monotonous, repetitive activity for a long while.
• Decision-making skills: Decision-making skills are defined as an individual’s ability, based on their knowledge and experience, to make the best decision at the right time from among several alternatives.
• Precaution: Precaution is necessary to avoid definite or probable risk, even in cases with no scientific or technical confidence that specific measures are harmful.
• Self-confidence: Self-confidence is a mental condition where the individual relies on and believes in their capabilities and talents to successfully perform tasks due to previous experience.
• Management of experience: Not only inexperienced individuals but also experienced ones are prone to errors. Therefore, the aspects of management of experience should be considered, as the experience itself, to prevent experienced individuals’ errors. Management of experience is sub-classified as a dynamic individual factor.
3. Task factors concern the elements of tasks and their methods of performance by individuals. Any incident due to task features and performance methods is classified as a task factor. The H-PSFs of this class are resented here.
• Workload: Defined as the amount of work an individual performs within a specific period. It can be physical or mental, depending on the type of work.
• Monotony: Described as lack of variety and tedious repetition of a task, leading to a feeling of monotony, loss of interest, lack of consciousness, and lack of precaution in the individuals involved in the task.
• Time pressure: Defined as the time available for performing a task from a specific task process. This PSF can negatively affect others, particularly stress, consciousness, experience management, perception, and interpretation.
• Task complexity: Concerns about how a specific task is performed. It should be noted that this PSF addresses the complexity of a particular task in a process rather than that of the process as a whole.
• Task instructions: Commands or rules established to guide or support individuals in the process of performing a duty or task. Incomplete or defective instructions sometimes cause incidents.
4. Team factors concern the performance of individuals as team members who interact to achieve a common purpose and the final consequence of all team members’ collaboration. The H-PSFs of this class are presented below.
• Communication between employees (CBE): It denotes individuals’ ability to exchange information via verbal and nonverbal media. The quick, clear, justified, and approved exchange indicates efficient communication.
• Teamwork: It is described as a clear division of roles and responsibilities upon the performance of a task. The definition also includes the quality of feedback among team members, level of trust, team structure and stability, consideration of team members’ needs and support, and mutually respectful behavior.
5. Organizational factors include any factors defined and controlled by an organization. These factors concern organizational features, attitudes, and behaviors affecting staff performance. The H-PSFs of this class are presented here.
• Safety culture: It denotes what is developed due to organizational effort to transfer all cultural elements to bring about safety for organization members, systems, and professional activities. It involves a series of values and priorities specified for all safety aspects by the entire staff at any level of the organization.
• Safety management systems (SMS): It concerns the set of methods and instructions devised for supervision and improvement, if needed, of operational safety.
• Training: It is defined as a constant process an organization provides to the staff to ensure they hold the appropriate knowledge, skills, and perspectives by the set standards.
• Quality and availability of the procedures, standards, and regulations (QA-PSR): It concerns the existence and application of official operating methods for the intended duties. A high-quality procedure is characterized by clarity, simplicity, and availability, given its strategy of description.
• Leadership: Leaders help themselves and others to do the right thing. They specify the route to achieve the purposes, generate an inspiring perspective, provide new ways to improve the conditions of the organization, and identify what the team or organization needs to succeed.
• Supervision: It is defined as applying management, development, and support to the staff.
• Shift pattern: It consists of working hours different from the routine working period, sometimes including irregular working hours.
• Relations within an organization: It indicates the social atmosphere among all the organization members and their interactions at different hierarchy levels.
• Incentives for employees: Incentives are tools organizations use to increase the staff’s motivation to perform their activities and tasks. The staff’s incentives are strongly correlated with their motivation.
6. System factors include any factors that specify the healthcare system features and the quality of individuals’ interaction with them that may affect their performance. The H-PSFs of this class are presented below.
• System design: It is described as achieving high quality and optimal efficiency in terms of components, modules, interfaces, and data to meet specific predetermined requirements of the system.
• Human-machine interface (HMI): It addresses how information is communicated among operators and equipment and assessed based on the clarity and validity of the information obtained by the equipment and its performance.
• Equipment: It includes everything associated with the equipment, such as performance, precision, shortage, and breakdown.
• Workplace: It includes everything associated with the equipment, such as performance, precision, shortage, and breakdown.
• Trust in equipment: It is described the extent to which operators trust the information output by particular equipment. Trust is affected by factors such as the duration of application, history of failure, and equipment reliability.
• Communication systems: It involves facilities consisting of physical units and equipment for the propagation of information among the staff.
• Similarity: It includes cases where errors occur due to the similarity between names, symptoms, etc.
7. Environmental factors include any factor outside the healthcare organization and over which there can be no control, such as weather conditions and third parties. The H-PSFs of this class are presented here.
• Weather conditions: Describe the atmospheric conditions each day, expressed in temperature, wind, cloud, precipitation, etc.
• Third parties: It concerns cases where individuals outside the organization cause an incident.
• Urban design: It concerns urban street conditions in terms of traffic, fitness (particularly for streets ending in hospitals), traffic lights, speed bumps, etc., and may cause errors in some instances.
8. Factors associated with the patient include any factor particular to the healthcare field, not applicable to others, involving those concerning the patient, one for the patient and one for their companion. The H-PSFs of this class are presented here.
• Patient: It is considered if an incident arises where the patient himself/herself plays a role.
• Patient’s companion: It is considered if an incident arises where the patient’s companion or family plays a role.
2. Materials and Methods
A total of 318 complaints of medical mistakes from March 2020 to March 2021 at 17 hospitals in Iran were analyzed for the planned H-PSFs. With and without repeats, the number of H-PSFs activations was assessed. These 17 hospitals were chosen because they gave the Health Ministry detailed descriptions of mistakes and occurrences that occurred over the time described above, including all the variables and personnel involved, reasons, etc. In the mode with repetition, a given H-PSF might be considered more than once in a medical mistake or event report. In the approach without repetition, a given H-PSF might be evaluated just once in a medical mistake or event report, even if the error was repeated. Also, this article’s graphs and statistical analysis results were obtained using Minitab software.
3. Result
Table 1 presents 318 medical mistake findings.
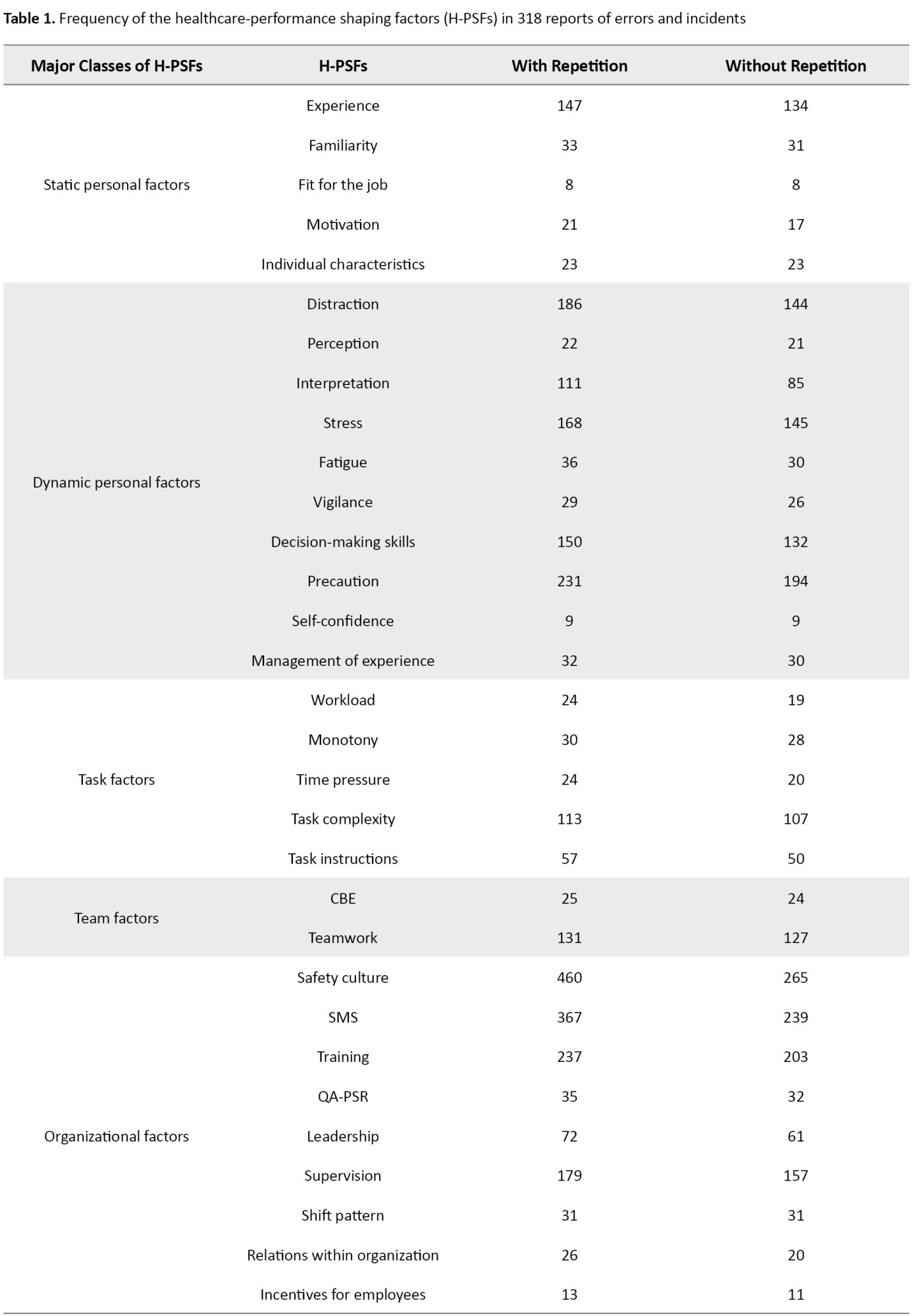
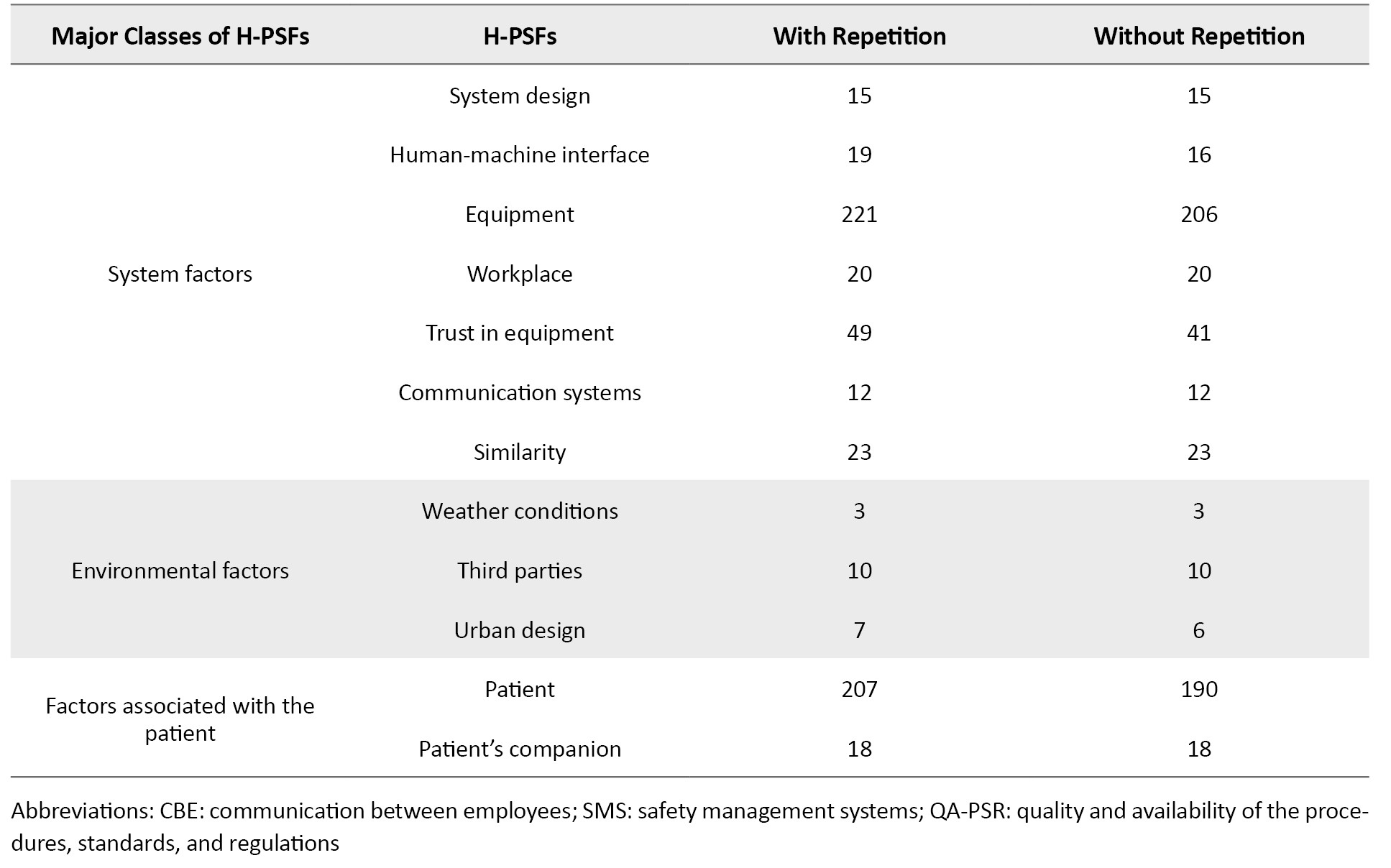
Figures 1 and 2 illustrate the H-PSF Pareto charts based on Table 1 for modes with and without repetition. Based on Figure 1, 14 H-PSFs led to 80% of mistakes or accidents. Figure 2 shows that 15 H-PSFs led to mistakes or occurrences. The Pareto charts show that focusing on a few H-PSFs may reduce healthcare mistakes and occurrences. The taxonomy of H-PSFs may help healthcare management reduce mistakes and occurrences.
With the help of H-PSFs classification, healthcare system managers can make better decisions in formulating general and comprehensive policies and policies to reduce errors and accidents.
To validate the proposed H-PSFs and their applications to health systems, we use the Chi-square goodness-of-fit test with the help of Minitab software. The null hypothesis and alternate hypothesis for this test are as follows:
H0: The results of the examination of the preliminary reports have good validity to be generalized to other healthcare systems.
H1: The results of the examination of the preliminary reports do not have good validity to be generalized to other healthcare systems. The type I error rate, α, was assumed to be 0.05.
For that purpose, 141 reports of medical errors that had occurred from March 21, 2021, to August 6, 2021, at 14 hospitals different from the primary 17 were examined as secondary reports, and the number of occurrences of each PSF in those reports was also extracted, where 1361 occurrences were identified in the way with repetition and 1190 in the mode without repetition. It should be noted that the reports were collected directly at the hospitals. The 14 hospitals were selected as they were different from the primary 17, for the results obtained from the goodness of fit test to be of greater validity.
In the mode with repetition, the Chi-square statistic was 40.8381. Since , there was no reason for rejection of the null hypothesis, which was therefore retained. In the mode without repetition, the value of the Chi-square statistic was 46.9218. Since , there was no reason for rejection of the null hypothesis, which was therefore retained. Thus, the findings in section 3 were validated by the results obtained from the goodness of fit test, and it can be said that the results of this article have enough validity to generalize the results to all healthcare systems.
4. Discussion
The emergence of medical errors and incidents is inevitable in healthcare. However, they affect people’s health as well as harm them financially. Therefore, it can significantly contribute to improving the conditions and minimizing these errors and incidents to analyze and investigate them and their causes. An appropriate approach to investigating errors and incidents in any area of expertise is to examine their causes, i.e. performance-shaping factors. For that purpose, a comprehensive, appropriate taxonomy was presented in this paper to explore the causes of errors and incidents in the healthcare field, i.e. introducing the shaping factors specific to the healthcare system, considering it as an integrated and coherent whole (H-PSF).
According to experts, 43 PSF were identified for the healthcare system. Using the medical error reports, the number of times that errors and mistakes were related to each of these 43 PSFs was calculated in two cases with and without repetition. To identify the most important PSFs, the Pareto principle has been used, and the results indicate that 14 H-PSFs in the non-repetitive mode and 15 H-PSFs in the repeated mode are responsible for the occurrence of errors.
5. Conclusion
Field managers can largely mitigate errors and incidents by considering these factors because the goodness of fit test was used to validate the proposed set of H-PSFs and examine its generalizability to all healthcare systems. The results demonstrated the great validity of the set to be generalized to similar systems.
Using the classification presented in this article, considering the healthcare system as an integrated whole to analyze human reliability is a suitable topic for future research.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and Supervision: Hossein Mahmoudi Sefidkouhi, Esmaeil Najafi, and Alireza Haji; Methodology: Hossein Mahmoudi Sefidkouhi; Investigation, Writing-original draft, and Writing-review & editing: All authors; Data collection: Hossein Mahmoudi Sefidkouhi; Data analysis: Hossein Mahmoudi Sefidkouhi and Abdollah Arasteh.
Conflict of interest
All authors declared no conflict of interest.
Acknowledgements
The authors appreciate all participants in the study.
References
- Abbaspour A, Saremi M, Alibabaei A, Moghanlu PS. Determining the optimal human reliability analysis (HRA) method in healthcare systems using Fuzzy ANP and Fuzzy TOPSIS. Journal of Patient Safety and Risk Management. 2020; 25(3):123-33. [DOI:10.1177/2516043519900431]
- Sujan MA, Embrey D, Huang H. On the application of human reliability analysis in healthcare: Opportunities and challenges. Reliability Engineering & System Safety. 2020; 194:106189. [DOI:10.1016/j.ress.2018.06.017]
- Loeppke R, Boldrighini J, Bowe J, Braun B, Eggins E, Eisenberg BS, et al. Interaction of health care worker health and safety and patient health and safety in the US health care system: Recommendations from the 2016 summit. Journal of Occupational and Environmental Medicine. 2017; 59(8):803-13. [DOI:10.1097/JOM.0000000000001100] [PMID]
- de Galizia A, Duval C, Serdet E, Weber P, Simon C, Iung B. Advanced investigation of HRA methods for probabilistic assessment of human barriers efficiency in complex systems for a given organisational and environmental context. Paper presented at: International Topical Meeting on Probabilistic Safety Assessment and Analysis, 26 April 2015; Sun Valley, United States. [Link]
- Tu J, Lou Y. A SLIM based methodology for human reliability analysis of lifting operations. Paper presented at: Proceedings 2013 International Conference on Mechatronic Sciences, Electric Engineering and Computer (MEC) 22 December 2013; Shenyang, China. [DOI:10.1109/MEC.2013.6885091]
- Kyriakidis M, Majumdar A, Grote G, Ochieng WY. Development and assessment of taxonomy for performance-shaping factors for railway operations. Transportation Research Record. 2012; 2289(1):145-53. [DOI:10.3141/2289-19]
- Kyriakidis M, Majumdar A, Ochieng WY. The human performance railway operational index-a novel approach to assess human performance for railway operations. Reliability Engineering & System Safety. 2018; 170:226-43. [DOI:10.1016/j.ress.2017.10.012]
- Smith P, Kyriakidis M, Majumdar A, Ochieng WY. Impact of European railway traffic management system on human performance in railway operations: European findings. Transportation Research Record. 2013; 2374(1):83-92. [DOI:10.3141/2374-10]
- Zhan Y, Tadikamalla PR, Craft JA, Lu J, Yuan J, Pei Z, et al. Human reliability study on the door operation from the view of Deep Machine Learning. Future Generation Computer Systems. 2019; 99:143-153. [DOI:10.1016/j.future.2018.11.055]
- Franciosi C, Di Pasquale V, Iannone R, Miranda S. A taxonomy of performance shaping factors for human reliability analysis in industrial maintenance. Journal of Industrial Engineering and Management. 2019; 12(1):115-32. [DOI:10.3926/jiem.2702]
- Park J, Boring RL, Ulrich TA, Lew R, Lee S, Park B, et al. A framework to collect human reliability analysis data for nuclear power plants using a simplified simulator and student operators. Reliability Engineering & System Safety. 2022; 221:108326. [DOI:10.1016/j.ress.2022.108326]
- Garg V, Vinod G, Prasad M, Chattopadhyay J, Smith C, Kant V. Human reliability analysis studies from simulator experiments using Bayesian inference. Reliability Engineering & System Safety. 2023; 229:108846. [DOI:10.1016/j.ress.2022.108846]
- Chauhan A, Golestani N, Yazdi M, Njue JCW, Abbassi R, Salehi F. A novel integrated methodology for human reliability assessment in hydrogen fuelling stations. International Journal of Hydrogen Energy. 2023; 84(34):12917-33. [DOI:10.1016/j.ijhydene.2022.12.181]
- Aalipour M, Ayele YZ, Barabadi A. Human reliability assessment (HRA) in maintenance of production process: A case study. International Journal of System Assurance Engineering and Management. 2016; 7(2):229-38. [DOI:10.1007/s13198-016-0453-z]
- Liu HC, Li Z, Zhang JQ, You XY. A large group decision making approach for dependence assessment in human reliability analysis. Reliability Engineering & System Safety. 2018; 176:135-44. [DOI:10.1016/j.ress.2018.04.008]
- Spurgin AJ. Human reliability assessment theory and practice. Boca Raton: CRC Press; 2009. [DOI:10.1201/9781420068528]
- Abedi G, Abedini E, Malakzadeh R, Araghian Mojarad F. Medical errors management before and after implementation of accreditation in hospital. Iranian Journal of Health Sciences. 2014; 2(4):59-66. [DOI:10.18869/acadpub.jhs.2.4.59]
- Buckle P, Clarkson PJ, Coleman R, Bound J, Ward J, Brown J. Systems mapping workshops and their role in understanding medication errors in healthcare. Applied Ergonomics. 2010; 41(5):645-56. [DOI:10.1016/j.apergo.2009.12.013] [PMID]
- Taib IA, McIntosh AS, Caponecchia C, Baysari MT. A review of medical error taxonomies: A human factors perspective. Safety Science. 2011; 49(5):607-15. [DOI:10.1016/j.ssci.2010.12.014]
- Bethune R, Francis N. Techniques aren't everything: Why conscientious well-trained surgeons make mistakes? Techniques in Coloproctology. 2015; 19(9):503-4. [DOI:10.1007/s10151-015-1352-z] [PMID]
- Kapur N, Parand A, Soukup T, Reader T, Sevdalis N. Aviation and healthcare: A comparative review with implications for patient safety. JRSM Open. 2015; 7(1):2054270415616548.[DOI:10.1177/2054270415616548] [PMID] [PMCID]
- Foster JD, Miskovic D, Allison AS, Conti JA, Ockrim J, Cooper EJ, et al. Application of objective clinical human reliability analysis (OCHRA) in assessment of technical performance in laparoscopic rectal cancer surgery. Techniques in Coloproctology. 2016; 20(6):361-7. [DOI:10.1007/s10151-016-1444-4] [PMID]
- Chana N, Porat T, Whittlesea C, Delaney B. Improving specialist drug prescribing in primary care using task and error analysis: An observational study. The British Journal of General Practice. 2017; 67(656):e157-67.[DOI:10.3399/bjgp17X689389] [PMID] [PMCID]
- Faiella G, Parand A, Franklin BD, Chana P, Cesarelli M, Stanton NA, et al. Expanding healthcare failure mode and effect analysis: A composite proactive risk analysis approach. Reliability Engineering & System Safety. 2018; 169:117-26. [DOI:10.1016/j.ress.2017.08.003]
- Levashenko V, Rabcan J, Zaitseva E. Reliability evaluation of the factors that influenced COVID-19 patients’ condition. Applied Sciences. 2021; 11(6):2589. [DOI:10.3390/app11062589]
- Khunti K, Griffiths A, Majeed A, Nagpaul C, Rao M. Assessing risk for healthcare workers during the covid-19 pandemic. BMJ. 2021; 372:n602. [DOI:10.1136/bmj.n602] [PMID]
Type of Study: Original Article |
Subject:
Health care Management
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |