Volume 12, Issue 4 (Autumn 2024)
Iran J Health Sci 2024, 12(4): 263-272 |
Back to browse issues page
Ethics code: IR.HSU.REC.1398.021
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gharaeinejad R, Haghighi A H, Askari R, Shahrabadi H. Effects of Skipping Rope Training and Running on Cardiovascular Risk Indicators in Overweight and Obese Girls. Iran J Health Sci 2024; 12 (4) :263-272
URL: http://jhs.mazums.ac.ir/article-1-970-en.html
URL: http://jhs.mazums.ac.ir/article-1-970-en.html
Department of Exercise Physiology, Faculty of Sport Sciences, Hakim Sabzevari University, Sabzevar, Iran. , ah.haghighi@hsu.ac.ir
Full-Text [PDF 880 kb]
(765 Downloads)
| Abstract (HTML) (2677 Views)
Full-Text: (2041 Views)
Introduction
All countries in the world experience overweight and obesity in their adolescent population [1]. The overweight/obesity prevalence in Iran is estimated at 35.09%, of which 56.55% is for people over 18 years old and 21.11% is for people under 18 years old [2]. Overweight and obesity result from a chronic imbalance between energy intake and energy expenditure [3]. In adolescents, obesity is associated with cardiovascular diseases (CVDs), type 2 diabetes, dyslipidemia, non-alcoholic fatty liver disease, obstructive sleep apnea, polycystic ovary syndrome, and psychiatric problems [4]. Identifying cardiovascular risk indicators associated with adolescence overweight/obesity is vital to design preventive interventions for cardiovascular diseases [5].
Maximum oxygen uptake (VO2max) is an important and widely used indicator of an individual’s aerobic capacity, which is closely related to body weight and body composition. It improves with the reduction of fat mass and the increase of lean mass [6]. There is also a close relationship between the BMI and the risk of CVDs; for every 5-unit increase in BMI, the risk of CVDs increases by 29% [7]. The amount of VO2max relative to body weight decreases slightly in girls during puberty (i.e. during adolescence) [8]. The increase in BMI in this period is due to the increase in fat mass and bone mineral density. The increase in fat mass is probably due to the release of the estrogen hormone. Therefore, VO2max may decrease more in obese girls [9].
Studies have also shown that lipid profile is an important risk indicator of CVDs. The association of high cholesterol with increased risk of CVDs is mainly related to the low-density lipoprotein (LDL) level. On the other hand, high-density lipoprotein (HDL) level is inversely related to mortality from coronary heart disease [10]. Apolipoprotein A1 (apoA1) is the main protein component of HDL, and it plays a key role in reverse cholesterol transport, the regulation of inflammatory response, and the antioxidant process. In contrast, apolipoprotein B (apoB) is the major protein component of LDL, which represents atherogenic particles. Therefore, it is believed that the increase in the concentration of apoB and the decrease in apoA1 have a strong relationship with CVDs and metabolic syndrome triglycerides (TG) [11].
Regular exercise is an effective method for reducing cardiovascular and metabolic diseases, especially in inactive adolescents [12]. It creates a feeling of satisfaction more than drug and treatment regimens that have side effects [13]. Physical activity can probably reduce cardiovascular risk indicators and mortality through the reduction of inflammatory, body fat, and obesity indicators [14]. The American College of Sports Medicine (ACSM) recommends that, in order to have an optimal effect and durability, it is better to exercise based on interval training [15]. In this regard, studies have shown that 8 weeks of skipping rope training (SRT) increases VO2max and reduces TG and total cholesterol (TC) levels, body fat percentage, and BMI in overweight/obese boys [16], and also increases apoA1 and reduce apoB in overweight/obese girls [17]. There are also studies that reported the effect of running training (RT) on cardiovascular risk indicators in obese people. Song et al. [18] showed that 8 weeks of RT reduced body weight, BMI, body fat percentage, waist circumference, hip circumference, TC level, and LDL level, and increased the HDL level in obese girls. Meng et al. [19] showed that 12 weeks of RT reduced body fat percentage and BMI and increased VO2peak and HDL in obese adolescent boys.
Since inactivity is one of the main causes of obesity [14] and physical activity is considered as an essential component in any training program to reduce or control body weight and treat obesity [16], it is important to know the role of cardiovascular indicators in obese people as well as effective training programs for obesity treatment. Performing SRT in interval mode is more fun and exciting than RT [20], and it may be a suitable alternative to RT because, according to the results of previous studies, overweight/obese people can benefit from it for the health of the cardiovascular system [16, 17]. Considering the low participation of obese people in other exercise programs [21], it may positively affect their participation. Also by reviewing literature, we did not find any research that compares the effect of these two training methods (SRT and RT) on cardiovascular risk indicators in overweight and obese girls. It is necessary to find the best training program according to the condition of obese people in order to improve their cardiovascular indicators. Accordingly, this research aims to compare the effects of SRT and RT on some cardiovascular risk indicators in overweight and obese girls.
Materials and Methods
Study design and participants
This is a quasi-experimental study with a pre-test/post-test design conducted in 2020. The study population consists of overweight and obese girls from Neyshabur city, north-east of Iran. For this purpose, 56 overweight and obese girls referred to health and educational centers (e.g. schools and universities) in Neyshabur City were assessed for eligibility. The sample size was determined at 23 for repeated measures analysis of variance using G*Power software, version 3.1.9.4 by considering the significance level of 0.05, test power of 0.8, and effect size of 0.6. However, considering the possibility of sample dropout, the sample size was increased to 30.
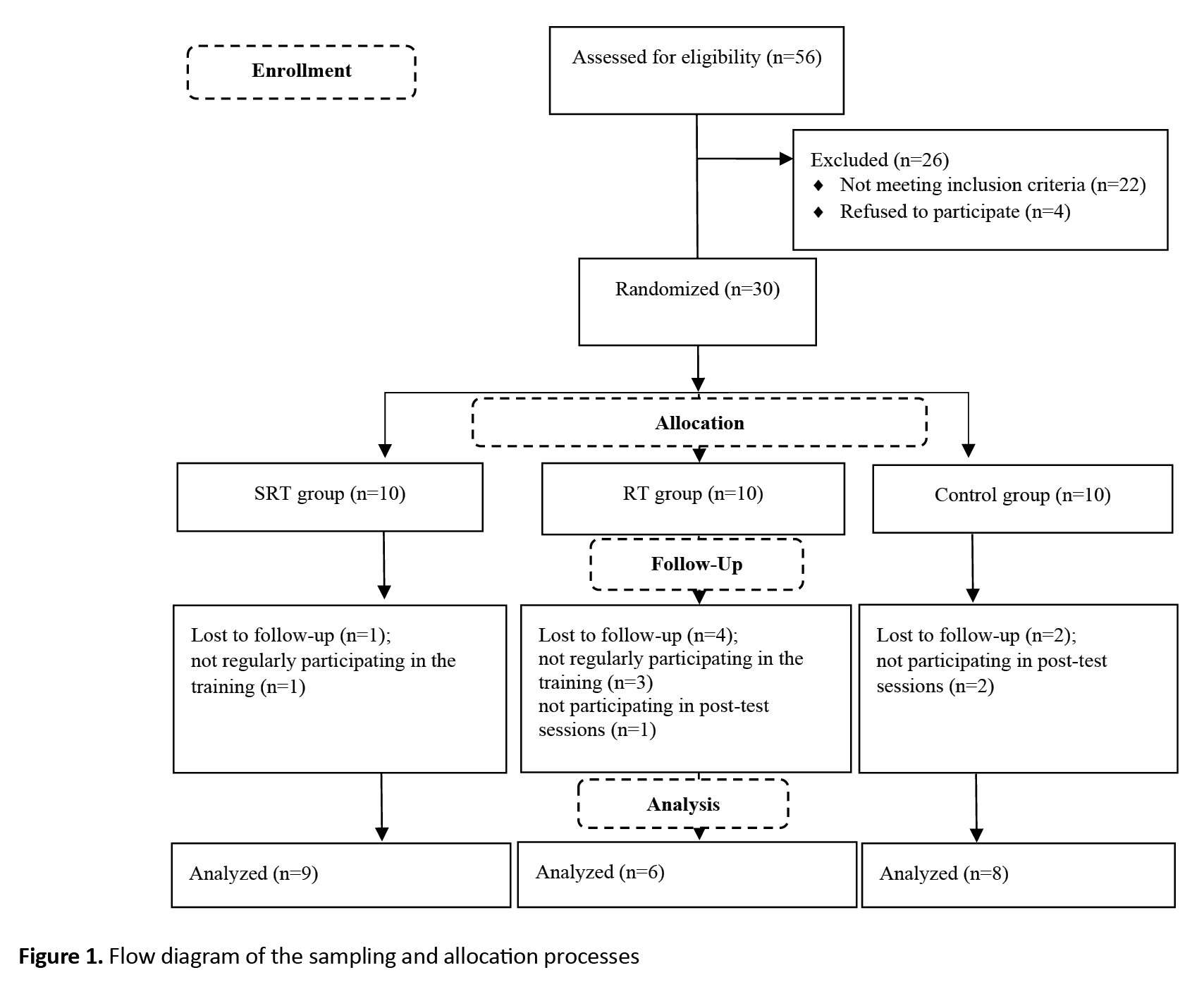
Inclusion criteria were age 15-20 years, BMI percentile ≥85 (BMI >23.5 kg/m2 for girls aged 15 and >25 kg/m2 for girls aged 20) [22], not taking drugs (e.g. medications for CVDs, nerve pain, diabetes), no smoking, and no regular participation in any training program in the last 6 months. Exclusion criteria were incidence of heart disease, absence from more than three training sessions, absence in post-test sessions, and unwillingness to complete the training program. After explaining the study objectives and methods, a written consent was obtained from all participants in the study. Then, they were randomly allocated to SRT (n=10), RT (n=10), and control (n=10) groups using the lottery method. During the training period, 7 participants (two from the control group, one from the SRT group, and four from the RT group) were excluded due to reasons such as not regularly participating in the training and post-test sessions. Finally, data analysis was done on the remaining 23 girls (Figure1).
Measurements
One week before the start of the study and random allocation, the participants were invited to attend Enghelab Sports Complex in Neyshabur city to measure their anthropometric indices, body composition, and aerobic capacity (VO2max). A general physician examined them prior to testing and intervention procedures. The participants were familiarized with the tests, and then measurements were taken by two assessors.
Blood sampling
Blood sampling was done after 12-14 hours of fasting and before and after training to measure the biochemical variables. The participants were asked not to do any strenuous physical activity for two days before blood sampling. The sampling was done at 8-10 AM by taking 5 mL of blood from the vein of right hand at sitting and resting position. A quantitative detection kit for lipid profile indicators in serum with a sensitivity of 1 mg/dL was prepared from Pars Azmoun Co, Iran. The immunoturbidimetry method and a special kit manufactured by Biorex Fars Co, Iran, were used to evaluate the level of apolipoproteins.
Anthropometric indices and body composition
Waist-to-hip ratio was calculated by dividing the waist circumference by the hip circumference. The body height was measured using a tape (NTT 9650, Nova, Iran) with bare feet and in a standing straight position. BMI was used as an index to determine obesity or body composition. For this purpose, the body weight was measured using a digital scale (EB9460, Camry, China) with bare feet. Then, the BMI was calculated by using the Equation 1:
1. BMI=Weight (kg)/Height (m2)
Subcutaneous fat was measured using a caliper (MK-60, Yagami, Japan) and Jackson and Pollack’s three-site skinfold formula (triceps, thigh, and suprailiac skinfolds) on the right side of the body [23].
VO2max
Cooper’s 12-min run test was used to determine VO2max. In one study, the validity of this test for female university students was reported to be strong (r=0.88, P<0.001) [24]. In the present study, the intraclass correlation coefficient (ICC) for this test was obtained 0.93 (95% CI, 0.8%, 0.98%). To perform the test, the participants ran for 12 minutes with maximum effort. Then, the distance traveled by each participant was recorded, and the VO2max was calculated using the Equation 2 [25]:
2. VO2max (mL/kg/min)=(Distance traveled in meters-504.9)/44.73
Exercise protocol
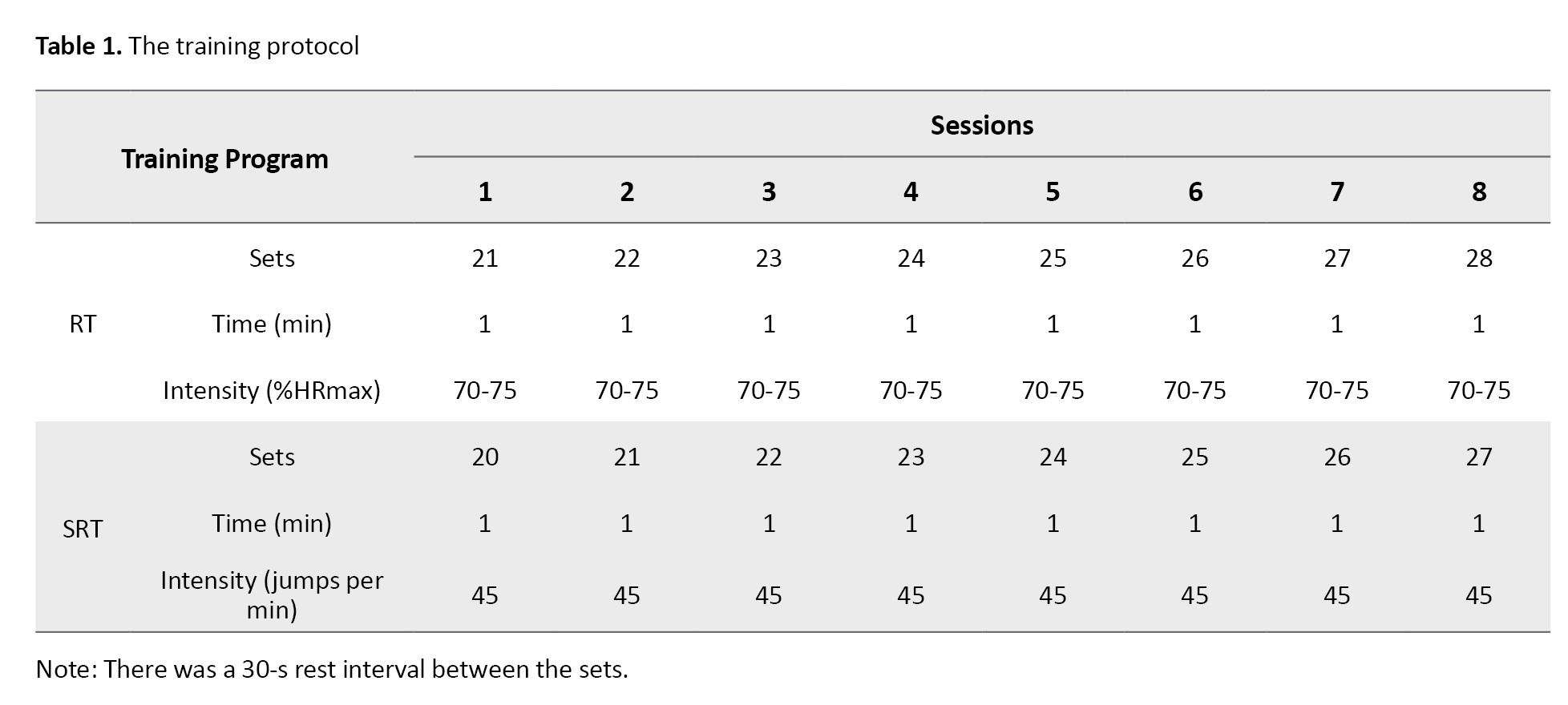
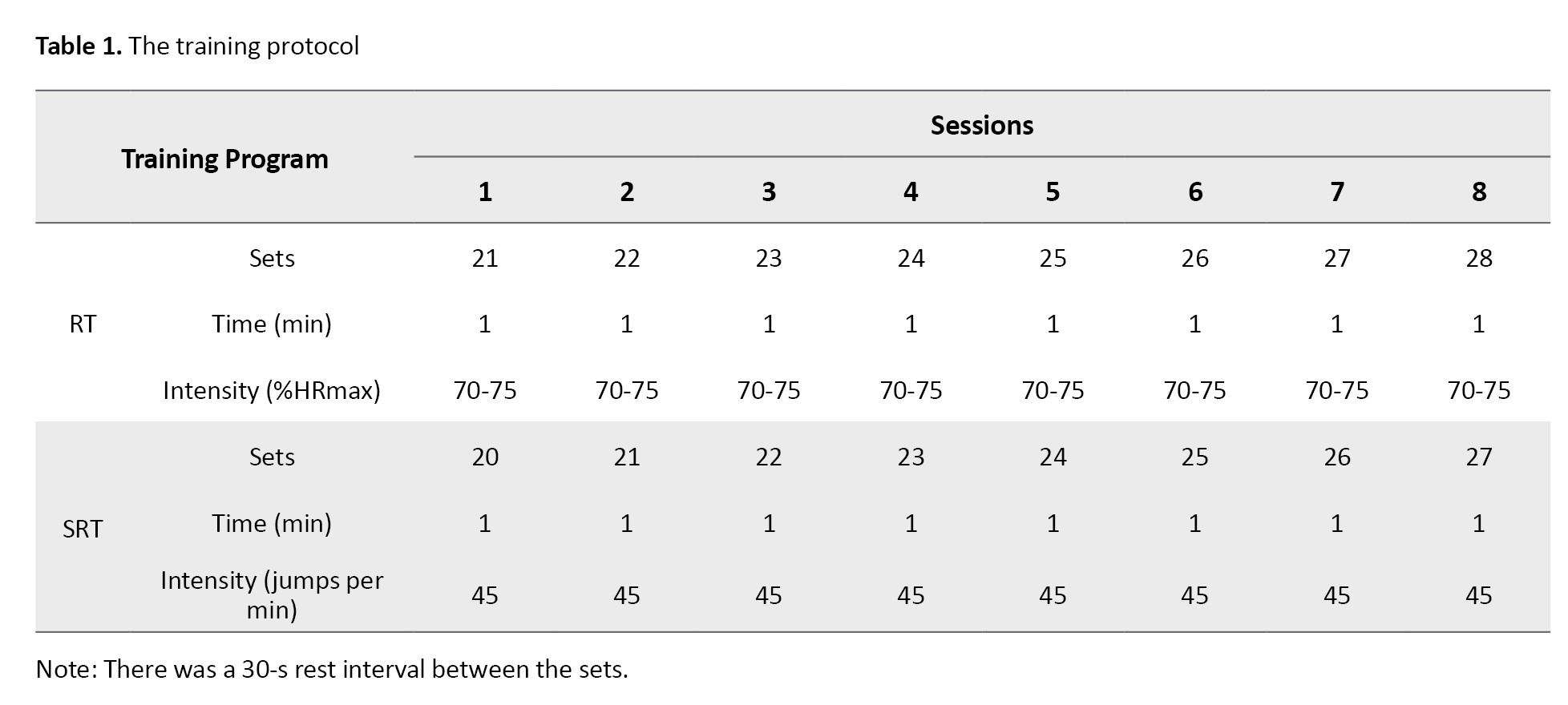
The girls in the intervention groups participated in SRT or RT programs for 8 weeks, three sessions per week, each for 45-60 minutes. In addition to the main exercises (Table 1), there was a 10-min warm-up session using body movements and stretching and a 5-min cool-down session using soft running and stretching movements.
The training programs were designed based on the participants’ characteristics, recommendations of sports coaches, and previous studies [26]. The training program was implemented under the supervision of two trainers. The maximum heart rate (HRmax) was calculated using the Equation 3:
3. HRmax=220-Age
The intensity of RT was controlled using a heart rate monitor (Polar H10, Finland), and the intensity of SRT was controlled based on the number of jumps per minute. The participants in the control group did not perform any exercise during this period, and their daily activities were the same as before.
Statistical analysis
Levene’s test was used to evaluate the homogeneity of variances, and the Shapiro-Wilk test was used to test the normality of data distribution. Due to the normality of distribution and the homogeneity of variances, repeated measures analysis of variance (ANOVA) was used for the comparison of physiological and biochemical variables, followed by Bonferroni’s post hoc test for pairwise comparison. All statistical analyses were performed in SPSS software, version 23, and the significance level was set at P<0.05.
Results
The percentage of compliance with training was calculated by the ratio of attendance sessions to the total number of required sessions, which was reported as 90.67±3.27 and 91.5±3.34 for the RT and SRT groups. The demographic characteristics of the participants are given in Table 2.
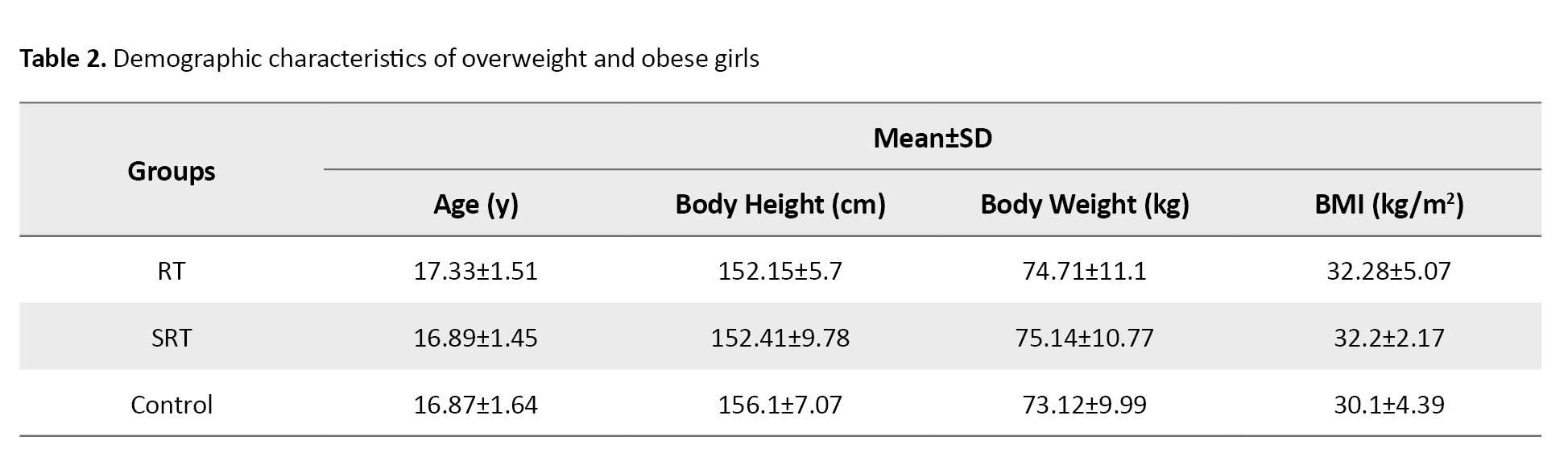
There was no significant difference among the groups in age (P=0.827), body height (P=0.563), body weight (P=0.920), and BMI (P=0.472) in the pre-test phase.
Descriptive statistics for the anthropometric and body composition indices and VO2max are presented in Table 3.
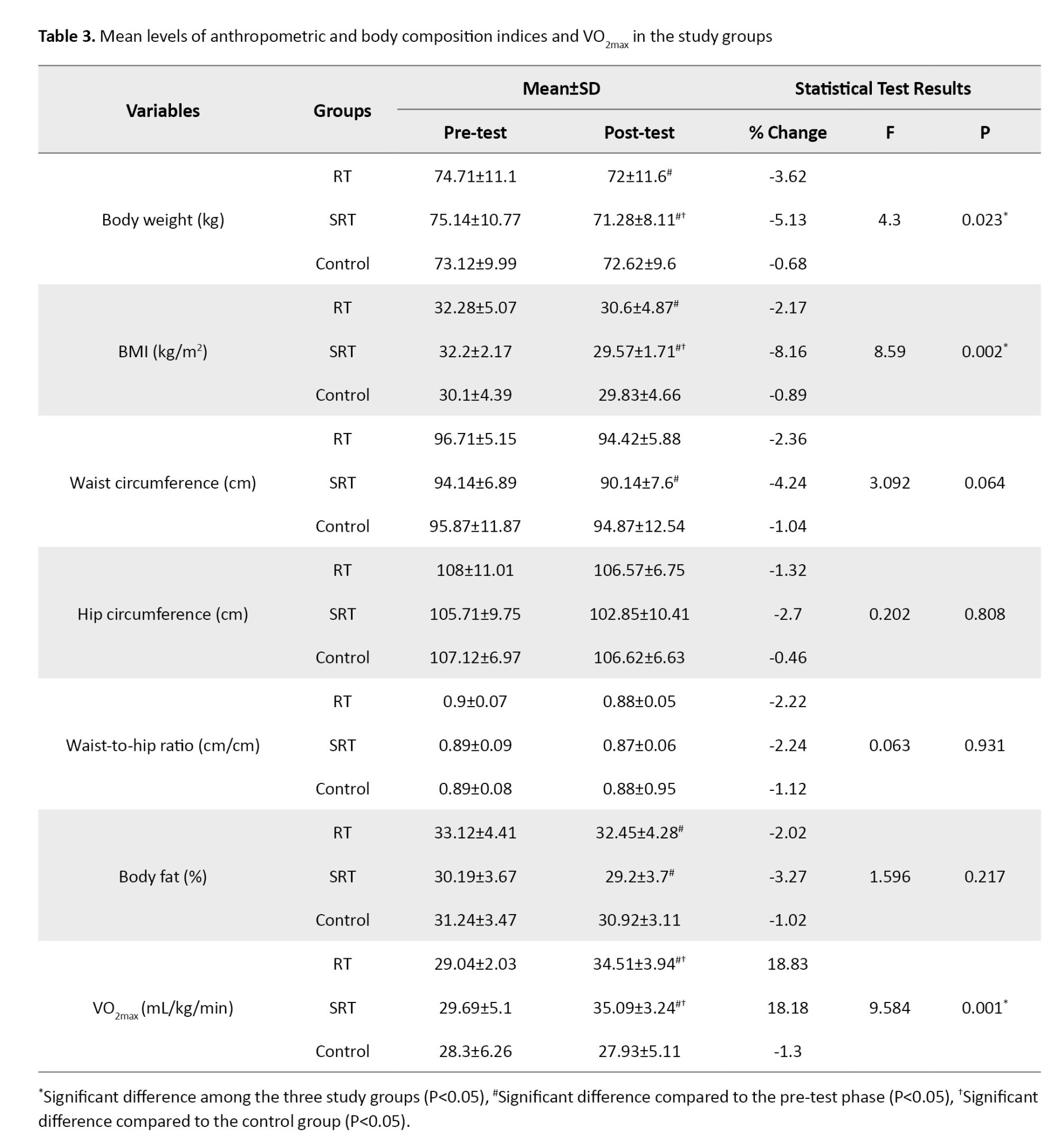
After 8 weeks of training, there was a significant decrease in body weight in the RT (P=0.009) and SRT (P=0.024) groups, a significant decrease in BMI in the RT (P=0.040) and SRT (P=0.009) groups, a significant decrease in waist circumference in the SRT group (P=0.005), a significant decrease in body fat percentage in the RT (P=0.008) and SRT (P=0.001) groups, and a significant increase in VO2max the RT (P=0.002) and SRT (P=0.001) groups (Table 3).
The results of repeated measures ANOVA (Table 3) showed a significant difference in body weight (P=0.023; pη2=0.303), BMI (P=0.002; pη2=0.462) and VO2max (P=0.001; pη2=0.489) among the three groups, but no significant difference was observed in the indicators of waist circumference (P=0.064), hip circumference (P=0.808), ratio of waist to hip circumference (P=0.931) and body fat percentage (P=0.217). Bonferroni’s post hoc test results (Table 3) showed that the body weight and BMI in the SRT group were significantly reduced compared to the control group (P=0.031) and the VO2max increased significantly in the SRT and RT groups compared to the control group (P=0.001).
Descriptive statistics for lipid profile, apoA1, and apoB are presented in Table 4.
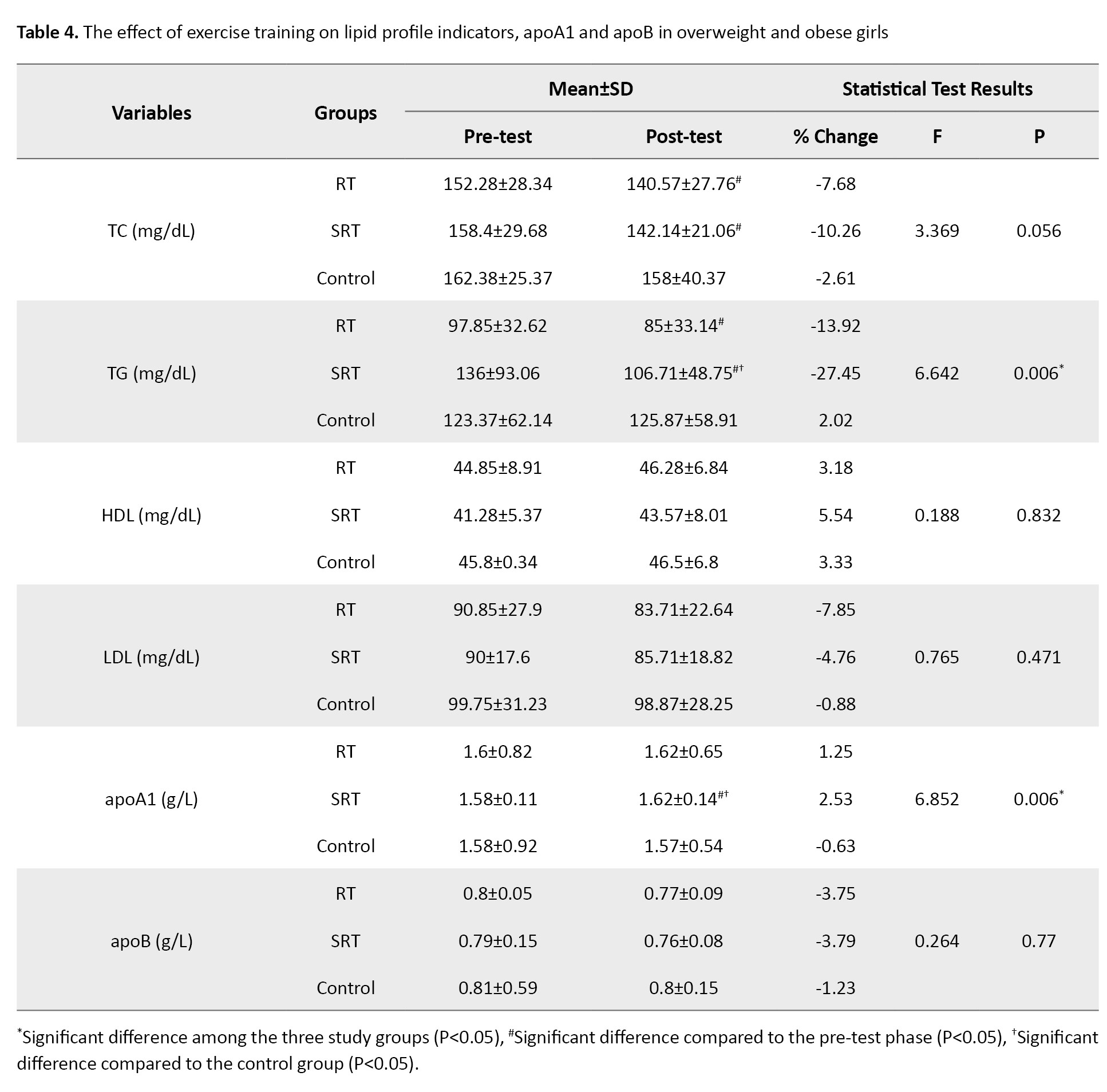
After 8 weeks of training, there was a significant decrease in TC in the RT (P=0.007) and SRT (P=0.020) groups, a significant decrease in TG in the RT (P=0.010) and SRT (P=0.030) groups, and a significant increase in apoA1 only in the SRT group (P=0.004) (Table 4).
The results of repeated measures ANOVA in Table 4 showed a significant difference in TG (P=0.006; pη2=0.399) and apoA1 (P=0.006; pη2=0.407) among the three groups; no significant difference was observed in the indicators of TC (P=0.056), HDL (P=0.832), LDL (P=0.471) and apoB (P=0.770). Bonferroni’s post hoc test results showed that the level of TG significantly decreased (P=0.003), and the level of apoA1 significantly increased (P=0.005) in the SRT group compared to the control group (Table 4).
Discussion
The present study was conducted with the aim of investigating the effect of two types of training programs (SRT and RT) on some cardiovascular risk indicators in overweight/obese girls. We found a significant improvement in body weight, BMI, VO2max, TG and apoA1 levels in the SRT group after training, while only the VO2max improved significantly in the RT group. There was no significant improvement in waist circumference, hip circumference, waist-to-hip ratio, body fat percentage, TC, HDL, LDL, or apoB levels after 8 weeks of training. Moreover, there was no significant difference between the two groups of SRT and RT in any indicators.
Ghorbanian and Mamaghani [17] showed that SRT did not improve body weight, body fat percentage, and BMI in overweight girls. Nazari et al. [27] stated that 8 weeks of SRT reduced body weight, BMI, and body fat percentage in obese male adolescents. Ghorbanian et al. [16] observed that 8 weeks of SRT reduced body fat percentage and BMI in overweight and obese male adolescents. The intensity of SRT was 40-110 and 60-90 jumps per min in the studies by Nazari et al. [27] and Ghorbanian et al. [16], respectively, but the intensity of SRT was lower (45 jumps per min) in our study. Kim et al. [13] showed that 12 weeks of SRT reduced body fat percentage and waist circumference in obese female adolescents. In our study, the rate of reduction in these two indicators in the SRT group was lower than in Kim et al.’s study [13], which may be due to the longer duration of the training period.
Karami et al. [28] stated that 8 weeks of regular training reduced body weight, BMI, and waist circumference in obese male adolescents. Meng et al. [19] also showed that 12 weeks of high-intensity interval training (HIIT) reduced body fat percentage and BMI in obese male adolescents. Racil et al. [29] showed that 12 weeks of moderate-intensity interval training (MIIT) reduced body weight and body fat percentage, but not waist circumference. Although these indicators decreased in our study, the intensity and duration of the training were probably not enough to bring the changes to a significant level. In this regard, Abassi et al. [30] showed that HIIT, compared to MIIT, caused more improvement in body composition and physical performance in obese and overweight adolescent girls. They also reported that, despite the improvement of these indicators, the MIIT group enjoyed more than the HIIT group during exercise. A study even emphasized that obese people with poor mood status and low self-efficacy should use MIIT [31].
Despite the lack of difference in the mentioned indicators between the SRT and RT groups, a significant decrease was observed in body weight and BMI. In the present study, the duration of each training session was almost the same in both training groups, and the training intensity was moderate. The reason for the decrease in body weight and BMI in the SRT group is probably due to the higher energy expenditure in this group, compared to RT, because the training skill level of the SRT group was lower than that of the RT group. Other studies also have stated that body composition improvement can be caused by the increased lipolysis activity in the fat tissue [32].
The results of the present study showed that VO2max improved in both training groups, but no significant difference was observed in this index between the two groups. This result is consistent with the results of Ghorbanian et al. [16], Ghorbanian and Mamaghani [17], Nazari et al. [27], Karami et al. [28], and Meng et al. [19]. Ingul et al. [33] showed that 12 weeks of RT with moderate intensity did not improve VO2max in obese girls. In their study, the intensity of exercise was 60-70% HRmax, which is lower than in our study. The exercise method was also different; in their study, it was a continuous type, while it was interval training in our study. The improvement of VO2max can be due to muscular and cardiovascular adaptations, including increased capillary density, increased number of mitochondria and mitochondrial enzymes related to the aerobic system, increased cardiac output, and decreased peripheral vascular resistance [34, 35].
The results of the present study showed that, after training, the TG and apoA1 levels improved significantly in the SRT group but not in the RT group. Ghorbanian et al. [16] stated that SRT for 8 weeks, 4 days per week (40 min per day) reduced the TG and TC levels in overweight and obese adolescent boys. Ghorbanian and Mamaghani [17] also stated that SRT for 8 weeks, 4 days a week (45 min per day) increased apoA1 and decreased apoB in overweight and obese girls. They also showed that, due to SRT, the amount of TG decreased and HDL increased significantly, but there was no improvement in TC and LDL. Song et al. [18] showed that 8 weeks of HIIT reduced TC and LDL and increased HDL in obese girls. Ahmadi et al. [36] showed that 8 weeks of RT increased HDL in obese girls, while the TC, TG, and LDL levels remained unchanged. Probably, the low sample size and less energy expenditure in the RT group compared to the SRT group were the reasons for the lack of change in lipid profile indicators, apoA1 and apoB.
Several possible mechanisms that cause an increase in apoA1 due to training include an increase in HDL, lipoprotein lipase (LPL), and lecithin cholesterol acyltransferase, and a decrease in hepatic triglyceride lipase [17]. The increase of the LPL activity causes the release of fatty acids from the triglycerides and generally increases the catabolism of triglycerides and the lipoproteins rich in triglycerides, and facilitates the removal of triglycerides from the bloodstream [37].
Conclusion
The two SRT and RT methods are not superior to each other in improving cardiovascular risk indicators; however, it seems that the SRT improves some health-related components of physical fitness and lipid profile. However, more research is needed to draw a definite conclusion.
Study limitations and recommendations
One of the limitations of the present study was the small sample size. The lack of significant change in most of the measured indicators is probably due to the small sample size. To solve this problem, further studies with a larger sample size are recommended. The non-control of the nutritional status of the participants was another limitation that may affect the results as a confounding factor. Therefore, it is recommended that this variable be controlled in future studies. Moreover, the 8-weeks duration of training might be a short period to show the signs of improvement in overweight and obese girls. Therefore, future studies should consider longer periods of training to achieve better goals. Non-blinding of the participants, personnel, and assessors was another limitation of the current study.
Ethical Considerations
Compliance with ethical guidelines
The procedures in this study were in accordance with the principles of the Declaration of Helsinki. The study was approved by the Ethics Committee of Hakim Sabzevari University, Sabzevar, Iran (Code: IR.HSU.REC.1398.021).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and supervision: Amir Hossein Haghighi and Roya Askari; Data collection, analysis, and literature review: Roya Gharaeinejad; Review and editing: Hadi Shahrabadi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all the participants who participated in this study for their cooperation.
References
All countries in the world experience overweight and obesity in their adolescent population [1]. The overweight/obesity prevalence in Iran is estimated at 35.09%, of which 56.55% is for people over 18 years old and 21.11% is for people under 18 years old [2]. Overweight and obesity result from a chronic imbalance between energy intake and energy expenditure [3]. In adolescents, obesity is associated with cardiovascular diseases (CVDs), type 2 diabetes, dyslipidemia, non-alcoholic fatty liver disease, obstructive sleep apnea, polycystic ovary syndrome, and psychiatric problems [4]. Identifying cardiovascular risk indicators associated with adolescence overweight/obesity is vital to design preventive interventions for cardiovascular diseases [5].
Maximum oxygen uptake (VO2max) is an important and widely used indicator of an individual’s aerobic capacity, which is closely related to body weight and body composition. It improves with the reduction of fat mass and the increase of lean mass [6]. There is also a close relationship between the BMI and the risk of CVDs; for every 5-unit increase in BMI, the risk of CVDs increases by 29% [7]. The amount of VO2max relative to body weight decreases slightly in girls during puberty (i.e. during adolescence) [8]. The increase in BMI in this period is due to the increase in fat mass and bone mineral density. The increase in fat mass is probably due to the release of the estrogen hormone. Therefore, VO2max may decrease more in obese girls [9].
Studies have also shown that lipid profile is an important risk indicator of CVDs. The association of high cholesterol with increased risk of CVDs is mainly related to the low-density lipoprotein (LDL) level. On the other hand, high-density lipoprotein (HDL) level is inversely related to mortality from coronary heart disease [10]. Apolipoprotein A1 (apoA1) is the main protein component of HDL, and it plays a key role in reverse cholesterol transport, the regulation of inflammatory response, and the antioxidant process. In contrast, apolipoprotein B (apoB) is the major protein component of LDL, which represents atherogenic particles. Therefore, it is believed that the increase in the concentration of apoB and the decrease in apoA1 have a strong relationship with CVDs and metabolic syndrome triglycerides (TG) [11].
Regular exercise is an effective method for reducing cardiovascular and metabolic diseases, especially in inactive adolescents [12]. It creates a feeling of satisfaction more than drug and treatment regimens that have side effects [13]. Physical activity can probably reduce cardiovascular risk indicators and mortality through the reduction of inflammatory, body fat, and obesity indicators [14]. The American College of Sports Medicine (ACSM) recommends that, in order to have an optimal effect and durability, it is better to exercise based on interval training [15]. In this regard, studies have shown that 8 weeks of skipping rope training (SRT) increases VO2max and reduces TG and total cholesterol (TC) levels, body fat percentage, and BMI in overweight/obese boys [16], and also increases apoA1 and reduce apoB in overweight/obese girls [17]. There are also studies that reported the effect of running training (RT) on cardiovascular risk indicators in obese people. Song et al. [18] showed that 8 weeks of RT reduced body weight, BMI, body fat percentage, waist circumference, hip circumference, TC level, and LDL level, and increased the HDL level in obese girls. Meng et al. [19] showed that 12 weeks of RT reduced body fat percentage and BMI and increased VO2peak and HDL in obese adolescent boys.
Since inactivity is one of the main causes of obesity [14] and physical activity is considered as an essential component in any training program to reduce or control body weight and treat obesity [16], it is important to know the role of cardiovascular indicators in obese people as well as effective training programs for obesity treatment. Performing SRT in interval mode is more fun and exciting than RT [20], and it may be a suitable alternative to RT because, according to the results of previous studies, overweight/obese people can benefit from it for the health of the cardiovascular system [16, 17]. Considering the low participation of obese people in other exercise programs [21], it may positively affect their participation. Also by reviewing literature, we did not find any research that compares the effect of these two training methods (SRT and RT) on cardiovascular risk indicators in overweight and obese girls. It is necessary to find the best training program according to the condition of obese people in order to improve their cardiovascular indicators. Accordingly, this research aims to compare the effects of SRT and RT on some cardiovascular risk indicators in overweight and obese girls.
Materials and Methods
Study design and participants
This is a quasi-experimental study with a pre-test/post-test design conducted in 2020. The study population consists of overweight and obese girls from Neyshabur city, north-east of Iran. For this purpose, 56 overweight and obese girls referred to health and educational centers (e.g. schools and universities) in Neyshabur City were assessed for eligibility. The sample size was determined at 23 for repeated measures analysis of variance using G*Power software, version 3.1.9.4 by considering the significance level of 0.05, test power of 0.8, and effect size of 0.6. However, considering the possibility of sample dropout, the sample size was increased to 30.
Inclusion criteria were age 15-20 years, BMI percentile ≥85 (BMI >23.5 kg/m2 for girls aged 15 and >25 kg/m2 for girls aged 20) [22], not taking drugs (e.g. medications for CVDs, nerve pain, diabetes), no smoking, and no regular participation in any training program in the last 6 months. Exclusion criteria were incidence of heart disease, absence from more than three training sessions, absence in post-test sessions, and unwillingness to complete the training program. After explaining the study objectives and methods, a written consent was obtained from all participants in the study. Then, they were randomly allocated to SRT (n=10), RT (n=10), and control (n=10) groups using the lottery method. During the training period, 7 participants (two from the control group, one from the SRT group, and four from the RT group) were excluded due to reasons such as not regularly participating in the training and post-test sessions. Finally, data analysis was done on the remaining 23 girls (Figure1).
Measurements
One week before the start of the study and random allocation, the participants were invited to attend Enghelab Sports Complex in Neyshabur city to measure their anthropometric indices, body composition, and aerobic capacity (VO2max). A general physician examined them prior to testing and intervention procedures. The participants were familiarized with the tests, and then measurements were taken by two assessors.
Blood sampling
Blood sampling was done after 12-14 hours of fasting and before and after training to measure the biochemical variables. The participants were asked not to do any strenuous physical activity for two days before blood sampling. The sampling was done at 8-10 AM by taking 5 mL of blood from the vein of right hand at sitting and resting position. A quantitative detection kit for lipid profile indicators in serum with a sensitivity of 1 mg/dL was prepared from Pars Azmoun Co, Iran. The immunoturbidimetry method and a special kit manufactured by Biorex Fars Co, Iran, were used to evaluate the level of apolipoproteins.
Anthropometric indices and body composition
Waist-to-hip ratio was calculated by dividing the waist circumference by the hip circumference. The body height was measured using a tape (NTT 9650, Nova, Iran) with bare feet and in a standing straight position. BMI was used as an index to determine obesity or body composition. For this purpose, the body weight was measured using a digital scale (EB9460, Camry, China) with bare feet. Then, the BMI was calculated by using the Equation 1:
1. BMI=Weight (kg)/Height (m2)
Subcutaneous fat was measured using a caliper (MK-60, Yagami, Japan) and Jackson and Pollack’s three-site skinfold formula (triceps, thigh, and suprailiac skinfolds) on the right side of the body [23].
VO2max
Cooper’s 12-min run test was used to determine VO2max. In one study, the validity of this test for female university students was reported to be strong (r=0.88, P<0.001) [24]. In the present study, the intraclass correlation coefficient (ICC) for this test was obtained 0.93 (95% CI, 0.8%, 0.98%). To perform the test, the participants ran for 12 minutes with maximum effort. Then, the distance traveled by each participant was recorded, and the VO2max was calculated using the Equation 2 [25]:
2. VO2max (mL/kg/min)=(Distance traveled in meters-504.9)/44.73
Exercise protocol
The girls in the intervention groups participated in SRT or RT programs for 8 weeks, three sessions per week, each for 45-60 minutes. In addition to the main exercises (Table 1), there was a 10-min warm-up session using body movements and stretching and a 5-min cool-down session using soft running and stretching movements.
The training programs were designed based on the participants’ characteristics, recommendations of sports coaches, and previous studies [26]. The training program was implemented under the supervision of two trainers. The maximum heart rate (HRmax) was calculated using the Equation 3:
3. HRmax=220-Age
The intensity of RT was controlled using a heart rate monitor (Polar H10, Finland), and the intensity of SRT was controlled based on the number of jumps per minute. The participants in the control group did not perform any exercise during this period, and their daily activities were the same as before.
Statistical analysis
Levene’s test was used to evaluate the homogeneity of variances, and the Shapiro-Wilk test was used to test the normality of data distribution. Due to the normality of distribution and the homogeneity of variances, repeated measures analysis of variance (ANOVA) was used for the comparison of physiological and biochemical variables, followed by Bonferroni’s post hoc test for pairwise comparison. All statistical analyses were performed in SPSS software, version 23, and the significance level was set at P<0.05.
Results
The percentage of compliance with training was calculated by the ratio of attendance sessions to the total number of required sessions, which was reported as 90.67±3.27 and 91.5±3.34 for the RT and SRT groups. The demographic characteristics of the participants are given in Table 2.
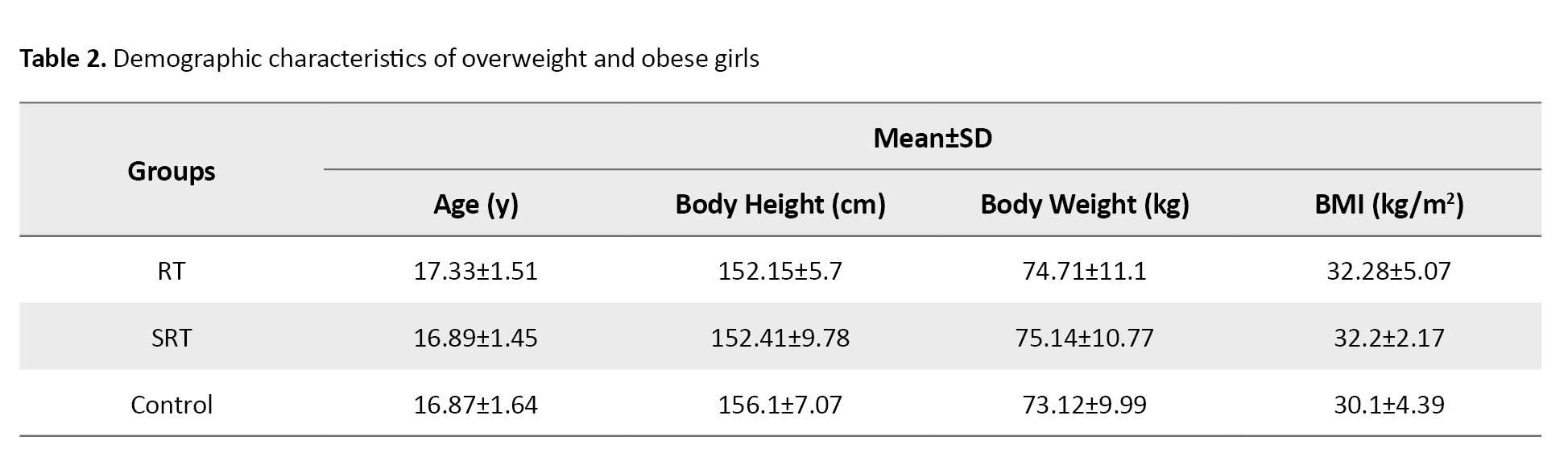
There was no significant difference among the groups in age (P=0.827), body height (P=0.563), body weight (P=0.920), and BMI (P=0.472) in the pre-test phase.
Descriptive statistics for the anthropometric and body composition indices and VO2max are presented in Table 3.
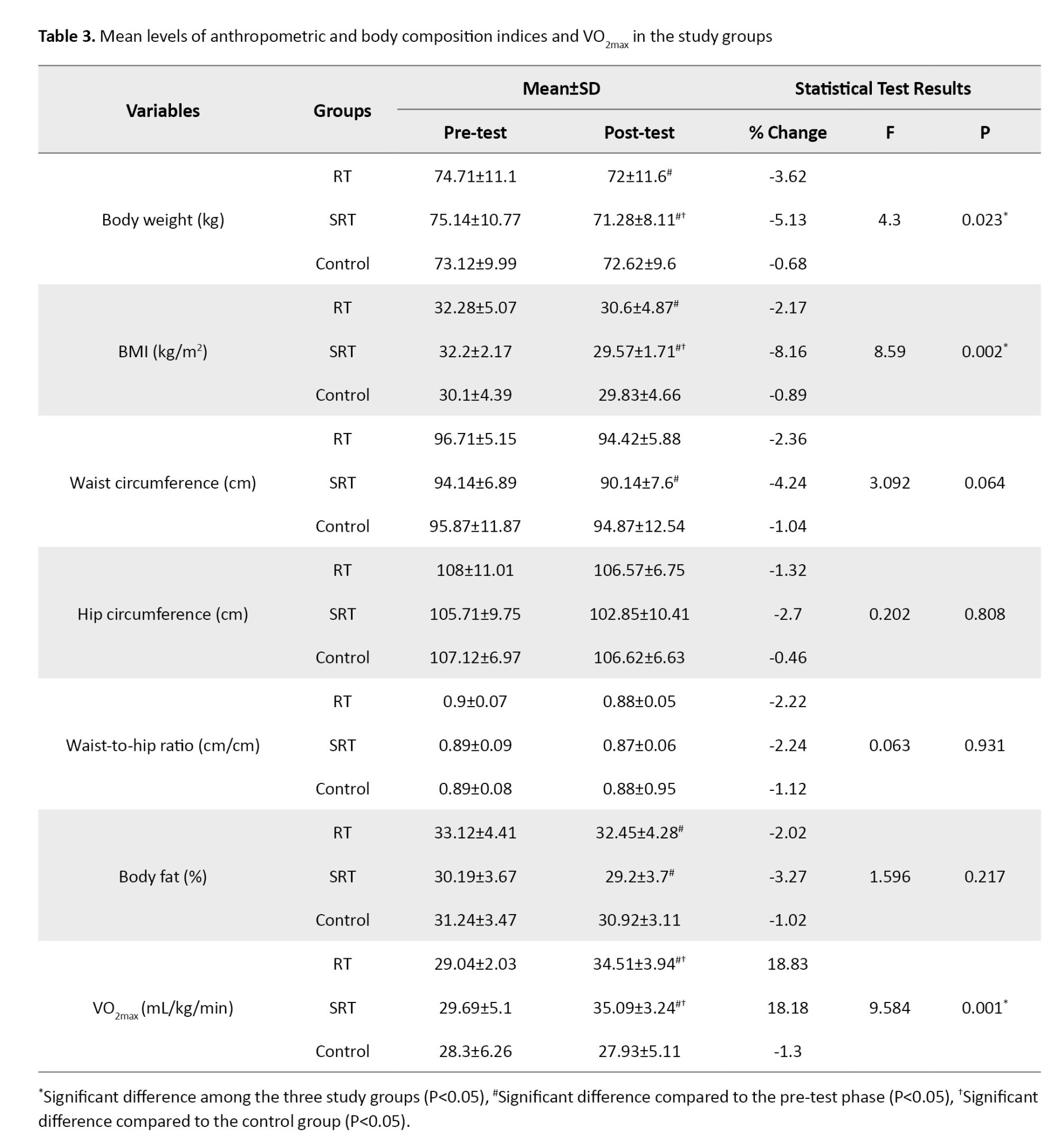
After 8 weeks of training, there was a significant decrease in body weight in the RT (P=0.009) and SRT (P=0.024) groups, a significant decrease in BMI in the RT (P=0.040) and SRT (P=0.009) groups, a significant decrease in waist circumference in the SRT group (P=0.005), a significant decrease in body fat percentage in the RT (P=0.008) and SRT (P=0.001) groups, and a significant increase in VO2max the RT (P=0.002) and SRT (P=0.001) groups (Table 3).
The results of repeated measures ANOVA (Table 3) showed a significant difference in body weight (P=0.023; pη2=0.303), BMI (P=0.002; pη2=0.462) and VO2max (P=0.001; pη2=0.489) among the three groups, but no significant difference was observed in the indicators of waist circumference (P=0.064), hip circumference (P=0.808), ratio of waist to hip circumference (P=0.931) and body fat percentage (P=0.217). Bonferroni’s post hoc test results (Table 3) showed that the body weight and BMI in the SRT group were significantly reduced compared to the control group (P=0.031) and the VO2max increased significantly in the SRT and RT groups compared to the control group (P=0.001).
Descriptive statistics for lipid profile, apoA1, and apoB are presented in Table 4.
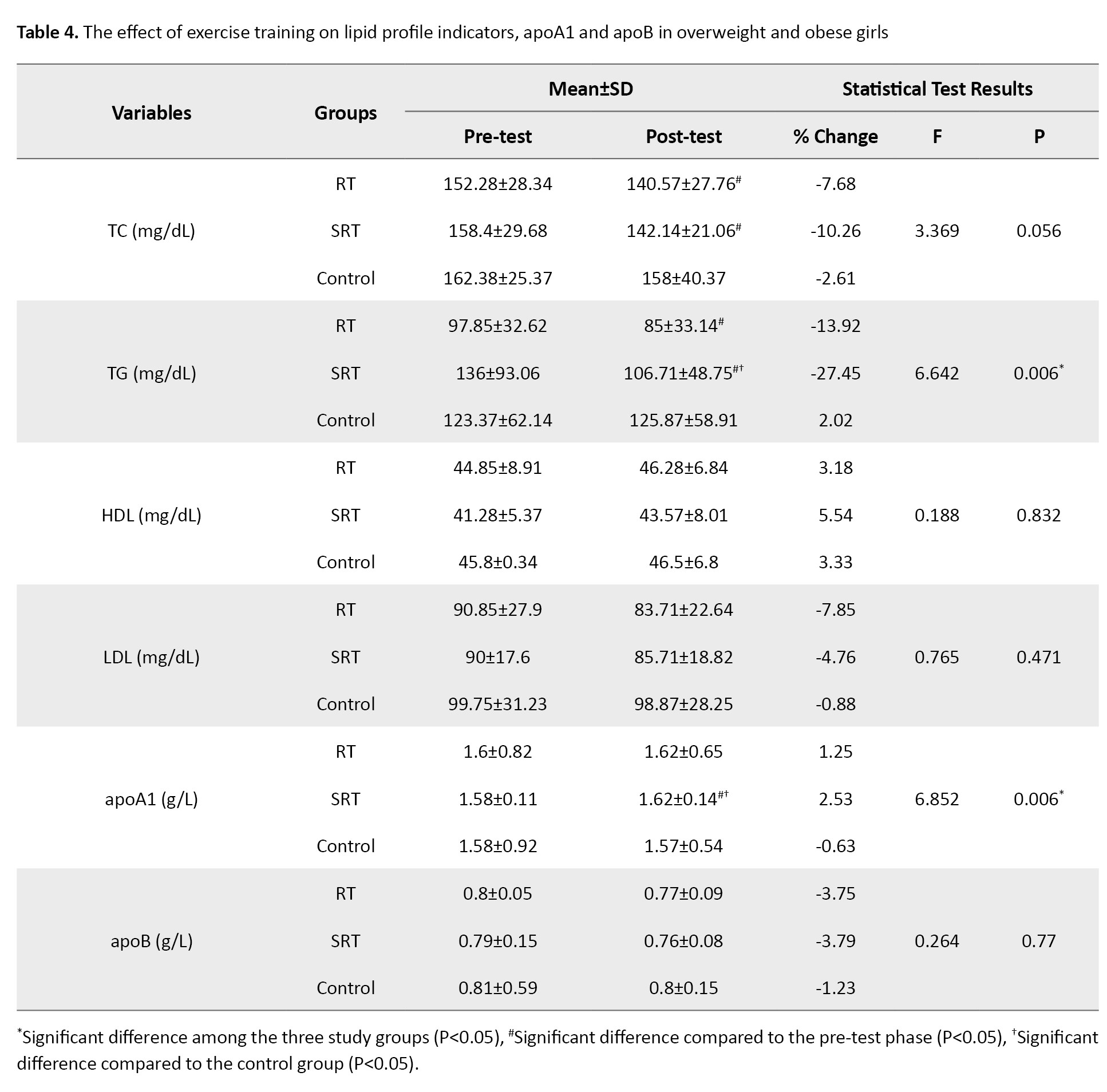
After 8 weeks of training, there was a significant decrease in TC in the RT (P=0.007) and SRT (P=0.020) groups, a significant decrease in TG in the RT (P=0.010) and SRT (P=0.030) groups, and a significant increase in apoA1 only in the SRT group (P=0.004) (Table 4).
The results of repeated measures ANOVA in Table 4 showed a significant difference in TG (P=0.006; pη2=0.399) and apoA1 (P=0.006; pη2=0.407) among the three groups; no significant difference was observed in the indicators of TC (P=0.056), HDL (P=0.832), LDL (P=0.471) and apoB (P=0.770). Bonferroni’s post hoc test results showed that the level of TG significantly decreased (P=0.003), and the level of apoA1 significantly increased (P=0.005) in the SRT group compared to the control group (Table 4).
Discussion
The present study was conducted with the aim of investigating the effect of two types of training programs (SRT and RT) on some cardiovascular risk indicators in overweight/obese girls. We found a significant improvement in body weight, BMI, VO2max, TG and apoA1 levels in the SRT group after training, while only the VO2max improved significantly in the RT group. There was no significant improvement in waist circumference, hip circumference, waist-to-hip ratio, body fat percentage, TC, HDL, LDL, or apoB levels after 8 weeks of training. Moreover, there was no significant difference between the two groups of SRT and RT in any indicators.
Ghorbanian and Mamaghani [17] showed that SRT did not improve body weight, body fat percentage, and BMI in overweight girls. Nazari et al. [27] stated that 8 weeks of SRT reduced body weight, BMI, and body fat percentage in obese male adolescents. Ghorbanian et al. [16] observed that 8 weeks of SRT reduced body fat percentage and BMI in overweight and obese male adolescents. The intensity of SRT was 40-110 and 60-90 jumps per min in the studies by Nazari et al. [27] and Ghorbanian et al. [16], respectively, but the intensity of SRT was lower (45 jumps per min) in our study. Kim et al. [13] showed that 12 weeks of SRT reduced body fat percentage and waist circumference in obese female adolescents. In our study, the rate of reduction in these two indicators in the SRT group was lower than in Kim et al.’s study [13], which may be due to the longer duration of the training period.
Karami et al. [28] stated that 8 weeks of regular training reduced body weight, BMI, and waist circumference in obese male adolescents. Meng et al. [19] also showed that 12 weeks of high-intensity interval training (HIIT) reduced body fat percentage and BMI in obese male adolescents. Racil et al. [29] showed that 12 weeks of moderate-intensity interval training (MIIT) reduced body weight and body fat percentage, but not waist circumference. Although these indicators decreased in our study, the intensity and duration of the training were probably not enough to bring the changes to a significant level. In this regard, Abassi et al. [30] showed that HIIT, compared to MIIT, caused more improvement in body composition and physical performance in obese and overweight adolescent girls. They also reported that, despite the improvement of these indicators, the MIIT group enjoyed more than the HIIT group during exercise. A study even emphasized that obese people with poor mood status and low self-efficacy should use MIIT [31].
Despite the lack of difference in the mentioned indicators between the SRT and RT groups, a significant decrease was observed in body weight and BMI. In the present study, the duration of each training session was almost the same in both training groups, and the training intensity was moderate. The reason for the decrease in body weight and BMI in the SRT group is probably due to the higher energy expenditure in this group, compared to RT, because the training skill level of the SRT group was lower than that of the RT group. Other studies also have stated that body composition improvement can be caused by the increased lipolysis activity in the fat tissue [32].
The results of the present study showed that VO2max improved in both training groups, but no significant difference was observed in this index between the two groups. This result is consistent with the results of Ghorbanian et al. [16], Ghorbanian and Mamaghani [17], Nazari et al. [27], Karami et al. [28], and Meng et al. [19]. Ingul et al. [33] showed that 12 weeks of RT with moderate intensity did not improve VO2max in obese girls. In their study, the intensity of exercise was 60-70% HRmax, which is lower than in our study. The exercise method was also different; in their study, it was a continuous type, while it was interval training in our study. The improvement of VO2max can be due to muscular and cardiovascular adaptations, including increased capillary density, increased number of mitochondria and mitochondrial enzymes related to the aerobic system, increased cardiac output, and decreased peripheral vascular resistance [34, 35].
The results of the present study showed that, after training, the TG and apoA1 levels improved significantly in the SRT group but not in the RT group. Ghorbanian et al. [16] stated that SRT for 8 weeks, 4 days per week (40 min per day) reduced the TG and TC levels in overweight and obese adolescent boys. Ghorbanian and Mamaghani [17] also stated that SRT for 8 weeks, 4 days a week (45 min per day) increased apoA1 and decreased apoB in overweight and obese girls. They also showed that, due to SRT, the amount of TG decreased and HDL increased significantly, but there was no improvement in TC and LDL. Song et al. [18] showed that 8 weeks of HIIT reduced TC and LDL and increased HDL in obese girls. Ahmadi et al. [36] showed that 8 weeks of RT increased HDL in obese girls, while the TC, TG, and LDL levels remained unchanged. Probably, the low sample size and less energy expenditure in the RT group compared to the SRT group were the reasons for the lack of change in lipid profile indicators, apoA1 and apoB.
Several possible mechanisms that cause an increase in apoA1 due to training include an increase in HDL, lipoprotein lipase (LPL), and lecithin cholesterol acyltransferase, and a decrease in hepatic triglyceride lipase [17]. The increase of the LPL activity causes the release of fatty acids from the triglycerides and generally increases the catabolism of triglycerides and the lipoproteins rich in triglycerides, and facilitates the removal of triglycerides from the bloodstream [37].
Conclusion
The two SRT and RT methods are not superior to each other in improving cardiovascular risk indicators; however, it seems that the SRT improves some health-related components of physical fitness and lipid profile. However, more research is needed to draw a definite conclusion.
Study limitations and recommendations
One of the limitations of the present study was the small sample size. The lack of significant change in most of the measured indicators is probably due to the small sample size. To solve this problem, further studies with a larger sample size are recommended. The non-control of the nutritional status of the participants was another limitation that may affect the results as a confounding factor. Therefore, it is recommended that this variable be controlled in future studies. Moreover, the 8-weeks duration of training might be a short period to show the signs of improvement in overweight and obese girls. Therefore, future studies should consider longer periods of training to achieve better goals. Non-blinding of the participants, personnel, and assessors was another limitation of the current study.
Ethical Considerations
Compliance with ethical guidelines
The procedures in this study were in accordance with the principles of the Declaration of Helsinki. The study was approved by the Ethics Committee of Hakim Sabzevari University, Sabzevar, Iran (Code: IR.HSU.REC.1398.021).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and supervision: Amir Hossein Haghighi and Roya Askari; Data collection, analysis, and literature review: Roya Gharaeinejad; Review and editing: Hadi Shahrabadi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all the participants who participated in this study for their cooperation.
References
- Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clinical Obesity. 2020; 10(6):e12416. [DOI:10.1111/cob.12416] [PMID]
- Abiri B, Ahmadi AR, Amini S, Akbari M, Hosseinpanah F, Madinehzad SA, et al. Prevalence of overweight and obesity among Iranian population: A systematic review and meta-analysis. Journal of Health, Population, and Nutrition. 2023; 42(1):70. [DOI:10.1186/s41043-023-00419-w] [PMID]
- Heindel JJ, Lustig RH, Howard S, Corkey BE. Obesogens: A unifying theory for the global rise in obesity. International Journal of Obesity. 2024; 48(4):449-60. [DOI:10.1038/s41366-024-01460-3] [PMID]
- Chung YL, Rhie YJ. Severe obesity in children and adolescents: Metabolic effects, assessment, and treatment. Journal of Obesity & Metabolic Syndrome. 2021; 30(4):326-35. [DOI:10.7570/jomes21063] [PMID]
- Choukem SP, Tochie JN, Sibetcheu AT, Nansseu JR, Hamilton-Shield JP. Overweight/obesity and associated cardiovascular risk factors in sub-Saharan African children and adolescents: A scoping review. International Journal of Pediatric Endocrinology. 2020; 2020:6. [DOI:10.1186/s13633-020-0076-7] [PMID]
- Zhou N. Assessment of aerobic exercise capacity in obesity, which expression of oxygen uptake is the best? Sports Medicine and Health Science. 2021; 3(3):138-47. [DOI:10.1016/j.smhs.2021.01.001] [PMID]
- Iyen B, Weng S, Vinogradova Y, Akyea RK, Qureshi N, Kai J. Long-term body mass index changes in overweight and obese adults and the risk of heart failure, cardiovascular disease and mortality: A cohort study of over 260,000 adults in the UK. BMC Public Health. 2021; 21(1):576. [DOI:10.1186/s12889-021-10606-1] [PMID]
- Landgraff HW, Riiser A, Lihagen M, Skei M, Leirstein S, Hallén J. Longitudinal changes in maximal oxygen uptake in adolescent girls and boys with different training backgrounds. Scandinavian Journal of Medicine & Science in Sports. 2021; 31 (Suppl 1):65-72. [DOI:10.1111/sms.13765] [PMID]
- Kondapalli A, Devpura G, Manohar S, Perakam S. Cardio respiratory fitness among normal, overweight and obese adolescent girls of hyderabad. International Journal of Health Sciences & Research. 2019; 9(3):65-70. [Link]
- Soppert J, Lehrke M, Marx N, Jankowski J, Noels H. Lipoproteins and lipids in cardiovascular disease: From mechanistic insights to therapeutic targeting. Advanced Drug Delivery Reviews. 2020; 159:4-33. [DOI:10.1016/j.addr.2020.07.019] [PMID]
- Chen F, Wu T, Bai C, Guo S, Huang W, Pan Y, et al. Serum apolipoprotein B/apolipoprotein A1 ratio in relation to intervertebral disk herniation: A cross-sectional frequency-matched case-control study. Lipids in Health and Disease. 2021; 20(1):79. [DOI:10.1186/s12944-021-01502-z] [PMID]
- Men J, Zou S, Ma J, Xiang C, Li S, Wang J. Effects of high-intensity interval training on physical morphology, cardiorespiratory fitness and metabolic risk factors of cardiovascular disease in children and adolescents: A systematic review and meta-analysis. PLoS One. 2023; 18(5):e0271845. [DOI:10.1371/journal.pone.0271845] [PMID]
- Kim J, Son WM, Headid Iii RJ, Pekas EJ, Noble JM, Park SY. The effects of a 12-week jump rope exercise program on body composition, insulin sensitivity, and academic self-efficacy in obese adolescent girls. Journal of Pediatric Endocrinology and Metabolism. 2020; 33(1):129-37. [DOI:10.1515/jpem-2019-0327] [PMID]
- Visco V, Izzo C, Bonadies D, Di Feo F, Caliendo G, Loria F, et al. Interventions to address cardiovascular risk in obese patients: Many hands make light work. Journal of Cardiovascular Development and Disease. 2023; 10(8):327. [PMID]
- Kilpatrick MW, Jung ME, Little JP. High-intensity interval training: A review of physiological and psychological responses. ACSM’s Health & Fitness Journal. 2014; 18(5):11-16. [DOI:10.1249/FIT.0000000000000067]
- Ghorbanian B, Ravassi A, Kordi MR, Hedayati M. The effects of rope training on lymphocyte ABCA1 expression, plasma ApoA-I and HDL-c in boy adolescents. International Journal of Endocrinology and Metabolism. 2013; 11(2):76-81. [DOI:10.5812/ijem.8178] [PMID]
- Ghorbanian B, Mamaghani H. [Effect of eight weeks of rope training along with portu-laca oleracea supplementation on serum levels of ox-LDL, Apo-A1, and Apo-B in overweight girls (Persian)]. Research in Medicine. 2021; 45 (1):15-22. [Link]
- Song X, Cui X, Su W, Shang X, Tao M, Wang J, et al. Comparative effects of high-intensity interval training and moderate-intensity continuous training on weight and metabolic health in college students with obesity. Scientific Reports. 2024; 14(1):16558. [DOI:10.1038/s41598-024-67331-z] [PMID]
- Meng C, Yucheng T, Shu L, Yu Z. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: A randomized controlled trial. BMC Pediatrics. 2022; 22(1):112. [DOI:10.1186/s12887-021-03079-z] [PMID]
- Chen CC, Lin SY. The impact of rope jumping exercise on physical fitness of visually impaired students. Research in Developmental Disabilities. 2011; 32(1):25-9. [DOI:10.1016/j.ridd.2010.08.010] [PMID]
- Zhang BG, Qian XF. Weight self-stigma and engagement among obese students in a physical education class. Frontiers in Psychology. 2022; 13:1035827. [DOI:10.3389/fpsyg.2022.1035827] [PMID]
- World Health Organization. Growth Reference 5-19 Years. Geneva: World Health Organization; 2020. [Link]
- Haghighi AH, Hosseini SB, Askari R, Shahrabadi H, Ramirez-Campillo R. Effects of plyometric compared to high-intensity interval training on youth female basketball player’s athletic performance. Sport Sciences for Health. 2023; 20(1):211-20. [DOI:10.1007/s11332-023-01096-2]
- Bandyopadhyay A. Validity of Cooper’s 12-min run test for estimation of maximum oxygen uptake in female university students. Indian Journal of Physiology and Pharmacology. 2014; 58(2):184-6. [PMID]
- Konieczna A, Radziminski L, Paszulewicz J, Lopez-Sanchez GF, Dragos P, Jstrzebski Z. Physical capacity and body composition in 13-16 year old soccer players during three-year training cycle. Baltic Journal of Health and Physical Activity. 2019; 11(4):47-57. [DOI:10.29359/BJHPA.11.4.06]
- Azmand F, Haghighi AH, Askari R, Shahrabadi H. The effect of concurrent training on some cardiovascular risk factors, serum estradiol and physical fitness indicators in overweight women with type 2 diabetes. Iranian Journal of Health Sciences. 2024; 12(1):59-68. [DOI:10.32598/ijhs.12.1.1000.1]
- Nazari S, TaheriChadorneshin H, Marefati H, AbtahiEivary S. The effect of rope jump training on serum levels of lipocalin-2, anthropometric parameters, and aerobic power in obese adolescent boys. Journal of Basic Research in Medical Sciences. 2020; 7(3):7-18. [Link]
- Karami H, Dehnou VV, Nazari A, Gahreman D. Regular training has a greater effect on aerobic capacity, fasting blood glucose and blood lipids in obese adolescent males compared to irregular training. Journal of Exercise Science & Fitness. 2021; 19(2):98-103. [DOI:10.1016/j.jesf.2020.11.003] [PMID]
- Racil G, Coquart JB, Elmontassar W, Haddad M, Goebel R, Chaouachi A, et al. Greater effects of high- compared with moderate-intensity interval training on cardio-metabolic variables, blood leptin concentration and ratings of perceived exertion in obese adolescent females. Biology of Sport. 2016; 33(2):145-52. [DOI:10.5604/20831862.1198633] [PMID]
- Abassi W, Ouerghi N, Feki M, Jebabli N, Andrade MS, Bouassida A, et al. Effects of moderate-vs. high-intensity interval training on physical fitness, enjoyment, and affective valence in overweight/obese female adolescents: A pre-/post-test study. European Review for Medical and Pharmacological Sciences. 2023; 27(9):3809-22. [PMID]
- De Feo P. Is high-intensity exercise better than moderate-intensity exercise for weight loss? Nutrition, Metabolism and Cardiovascular Diseases. 2013; 23(11):1037-42. [DOI:10.1016/j.numecd.2013.06.002] [PMID]
- Rodrigues AC, Prímola-Gomes TN, Peluzio MCG, Hermsdorff HHM, Natali AJ. Aerobic exercise and lipolysis: A review of the β-adrenergic signaling pathways in adipose tissue. Science & Sports. 2021; 36(1):16-26. [DOI:10.1016/j.scispo.2020.04.006]
- Ingul CB, Dias KA, Tjonna AE, Follestad T, Hosseini MS, Timilsina AS, et al. Effect of high intensity interval training on cardiac function in children with obesity: A randomised controlled trial. Progress in Cardiovascular Diseases. 2018; 61(2):214-21. [DOI:10.1016/j.pcad.2018.01.012] [PMID]
- Santisteban KJ, Lovering AT, Halliwill JR, Minson CT. Sex differences in VO2max and the impact on endurance-exercise performance. International Journal of Environmental Research and Public Health. 2022; 19(9):4946. [DOI:10.3390/ijerph19094946] [PMID]
- Lee J, Zhang XL. Physiological determinants of VO2max and the methods to evaluate it: A critical review. Science & Sports. 2021; 36(4):259-71. [DOI:10.1016/j.scispo.2020.11.006]
- Ahmadi M, Abbassi Daloii A, Shadmehri S, Agghaei Bahmanbeglu N. [Compare the effect of eight weeks aerobic and resistance training on oxidant, antioxidant status and lipid profile in obese girls (Persian)]. Sport and Exercise Physiology. 2018; 11(1):139-52. [Link]
- Kimura T, Tsunekawa K, Nagasawa T, Aoki T, Miyashita K, Yoshida A. et al. Circulating levels of lipoprotein lipase and glycosylphosphatidylinositol-anchored high-density lipoprotein binding protein 1: new markers for cardiovascular diseases among noncommunicable diseases: A brief narrative review. Journal of Laboratory and Precision Medicine. 2023; 8. [DOI:10.21037/jlpm-23-12]
Type of Study: Original Article |
Subject:
Health
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |