Volume 13, Issue 2 (Spring 2025)
Iran J Health Sci 2025, 13(2): 123-132 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Babaei S, Moosazadeh M, Kheradmand M, Hosseini A, Bagheri-Nesami M. Association Between Menopause and Metabolic Syndrome in the Registration Phase Data of Tabari Cohort Population. Iran J Health Sci 2025; 13 (2) :123-132
URL: http://jhs.mazums.ac.ir/article-1-998-en.html
URL: http://jhs.mazums.ac.ir/article-1-998-en.html
Seyed-Robabe Babaei 

 , Mahmood Moosazadeh
, Mahmood Moosazadeh 

 , Motahareh Kheradmand
, Motahareh Kheradmand 

 , Amirsaeed Hosseini
, Amirsaeed Hosseini 

 , Masoumeh Bagheri-Nesami *
, Masoumeh Bagheri-Nesami * 




 , Mahmood Moosazadeh
, Mahmood Moosazadeh 

 , Motahareh Kheradmand
, Motahareh Kheradmand 

 , Amirsaeed Hosseini
, Amirsaeed Hosseini 

 , Masoumeh Bagheri-Nesami *
, Masoumeh Bagheri-Nesami * 


Traditional and Complementary Medicine Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran. & World Federation of Acupuncture-Moxibustion Societies (WFAS), Beijing, China. , anna3043@gmail.com
Full-Text [PDF 786 kb]
(105 Downloads)
| Abstract (HTML) (287 Views)
Full-Text: (1 Views)
Introduction
Metabolic syndrome (also called syndrome X) is an insulin resistance syndrome. It involves a set of disorders in glucose metabolism, dyslipidemia, hypertension and central obesity that can predict the progression of cardiovascular diseases (CVD) and type 2 diabetes in the future [1, 2]. The international diabetes federation (IDF) and the adult treatment panel III (ATP III) guidelines have provided different definitions for the components of metabolic syndrome [3-5]. Numerous studies have suggested that metabolic syndrome is associated with an increased risk of coronary heart disease and heart attack [6] and an increase in deaths from CVDs by 3 to 5 times [7, 8]. The prevalence of metabolic syndrome is increasing worldwide. A systematic and meta-analysis study reported 36.9% and 34.6% prevalence rates for metabolic syndrome in Iran based on the ATP III and IDF criteria, respectively [9]. The prevalence of metabolic syndrome can be affected by various factors such as age, gender, family history, stress, inactivity, hormonal factors, malnutrition and the socioeconomic status of a community. These factors and their prevalence rates vary in different geographical areas [10]. One of the factors affecting the prevalence of metabolic syndrome is menopause. Menopause refers to the complete cessation of ovarian function, which occurs spontaneously (natural menopause) or iatrogenic (secondary menopause) [11]. The average age of women at menopause is 51 years, and only 4% of women experience natural menopause before the age of 40 [12]. Hot flashes, night sweats, vaginal atrophy, osteoporosis, psychiatric disorders, sexual dysfunction, skin lesions, CVD, cancer, metabolic disorders and obesity are the most obvious symptoms that occur in the menopausal age and continue until old age. These factors can adversely affect the quality of life of women [13]. A study conducted on Moroccan women showed that metabolic syndrome and abdominal obesity are more common in post-menopausal women than pre-menopausal women, and menopausal women with metabolic syndrome had at least three risk factors for this syndrome [14]. Studies conducted in the USA have found that the incidence of metabolic syndrome is higher in post-menopausal women than in pre-menopausal women [2]. Menopause induces lipid metabolism impairment and altered fatty acid synthesis, promoting insulin resistance, abdominal obesity and dyslipidemia, thereby increasing cancer risk [15, 16]. Concurrently, estrogen deficiency independently elevates hypertension susceptibility in postmenopausal women [17].
Given the high prevalence of metabolic syndrome, obesity, CVD and diabetes in recent years in the world, and also since no study has addressed metabolic syndrome and its relationship with menopause among women living in Mazandaran Province, Iran, the present study sought to examine the relationship between metabolic syndrome and menopause in the Tabari cohort population. The insights from this study can be used by health education experts and planners of the Ministry of Health, Treatment and Medical Education to develop future interventions and policies.
Material and Methods
The current study is a cross-sectional study conducted within the framework of the Tabari cohort study (TCS), and the data collected in the first phase of the study was used. TCS is a part of the national cohort study entitled prospective epidemiological research studies in Iran (Persian), the details of which are mentioned in other studies of the Tabari cohort [18-20]. The TCS recruited participants from June 2015 to November 2017 using a census-based sampling method. In urban regions, two health care volunteers identified eligible individuals, while health care workers facilitated enrollment in mountainous areas. Urban recruitment started from the right side of the cohort center. Recruitment in mountainous regions was conducted through household registries maintained at local health houses. From an initial pool of 12191 eligible urban residents, 7012 were included in the Tabari cohort. Similarly, among 4417 eligible individuals in mountainous areas, 3243 were enrolled. The first phase of TCS comprised 10255 participants aged 35–70 years (7012 urban and 3243 mountainous populations) from Sari City, Mazandaran Province, Iran.
Data were collected using a structured questionnaire standardized by the PERSIAN cohort team. Moreover, fasting blood samples (12-hour fast) were taken from all participants for laboratory tests. Fasting blood sugar, cholesterol level, triglyceride and high-density lipoprotein (HDL) cholesterol levels were measured using BT 1500 (Biotechnic, Italy). The blood pressure of all participants in the TCS was measured twice with an interval of 10 minutes using a Riester dial sphygmomanometer. Measurement of anthropometric indicators was done by trained personnel based on standard protocol [21].
The exclusion criteria of this study were cancer and kidney transplants. The sampling was performed using the census method; in the first phase of the Tabari cohort, 6106 women aged 35-70 were enrolled. Women who self-reported menopause and one year had passed since their last period were considered menopausal. According to the ATP III criteria, women who had at least three of the following were considered to have metabolic syndrome:
1) Waist circumference size more than 88 cm; 2) Triglyceride equal to or more than 150 mg/dL or drug use; 3) HDL cholesterol less than 50 mg/dL; 4) Hypertension, defined as a systolic blood pressure of 130 mm Hg or higher and a diastolic blood pressure of 85 mm Hg or higher, or receiving medication and 5) Hyperglycemia, characterized by a fasting blood sugar level of 100 mg/dL or higher or receiving medication [3, 5].
The demographic and medical information investigated in this study included age, sex, occupation, marital status, educational status, socioeconomic status, place of living, underlying disease, body mass index (BMI), metabolic syndrome indicators, menopause age, and its cause. Descriptive statistics such as Mean±SD and frequency were used to describe the variables. The chi-square test and logistic regression were used to determine the relationship between the two qualitative variables. The data were entered into SPSS software, version 21 for analysis. P≤0.05 was also considered significant.
Results
In the current study, 6106 women aged 35-70 were enrolled, of which 2591 were post-menopausal. Among post-menopausal women, 2033 participants (78.5%) had metabolic syndrome and 558 (21.5%) did not. The results of the chi-square test indicated no significant association between metabolic syndrome and factors such as the presence of menopause (P=0.181), age at menopause (P=0.058), natural menopause (P=0.27), unnatural menopause (P=0.69) and the type of menopause (natural versus unnatural) (P=0.181).
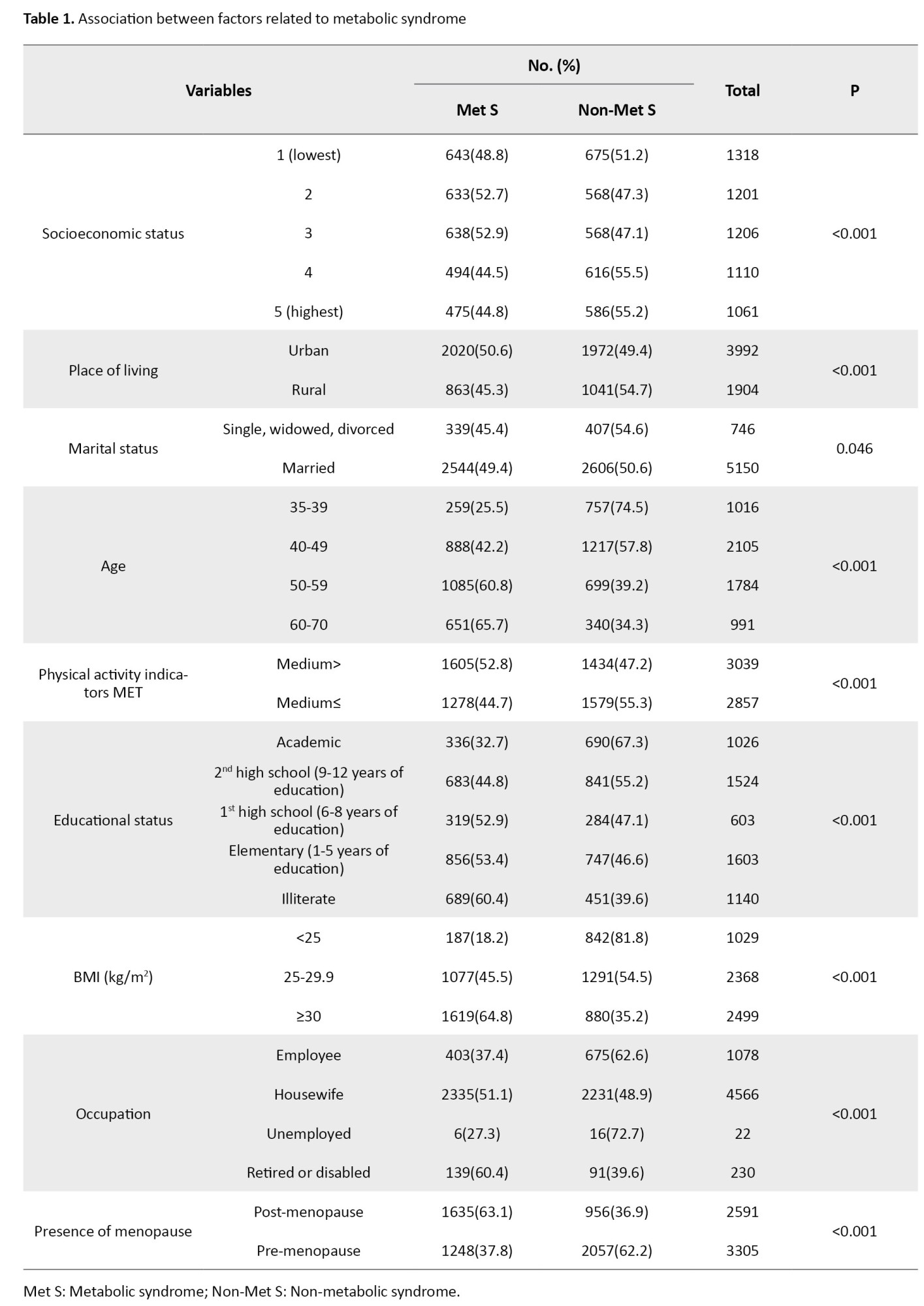
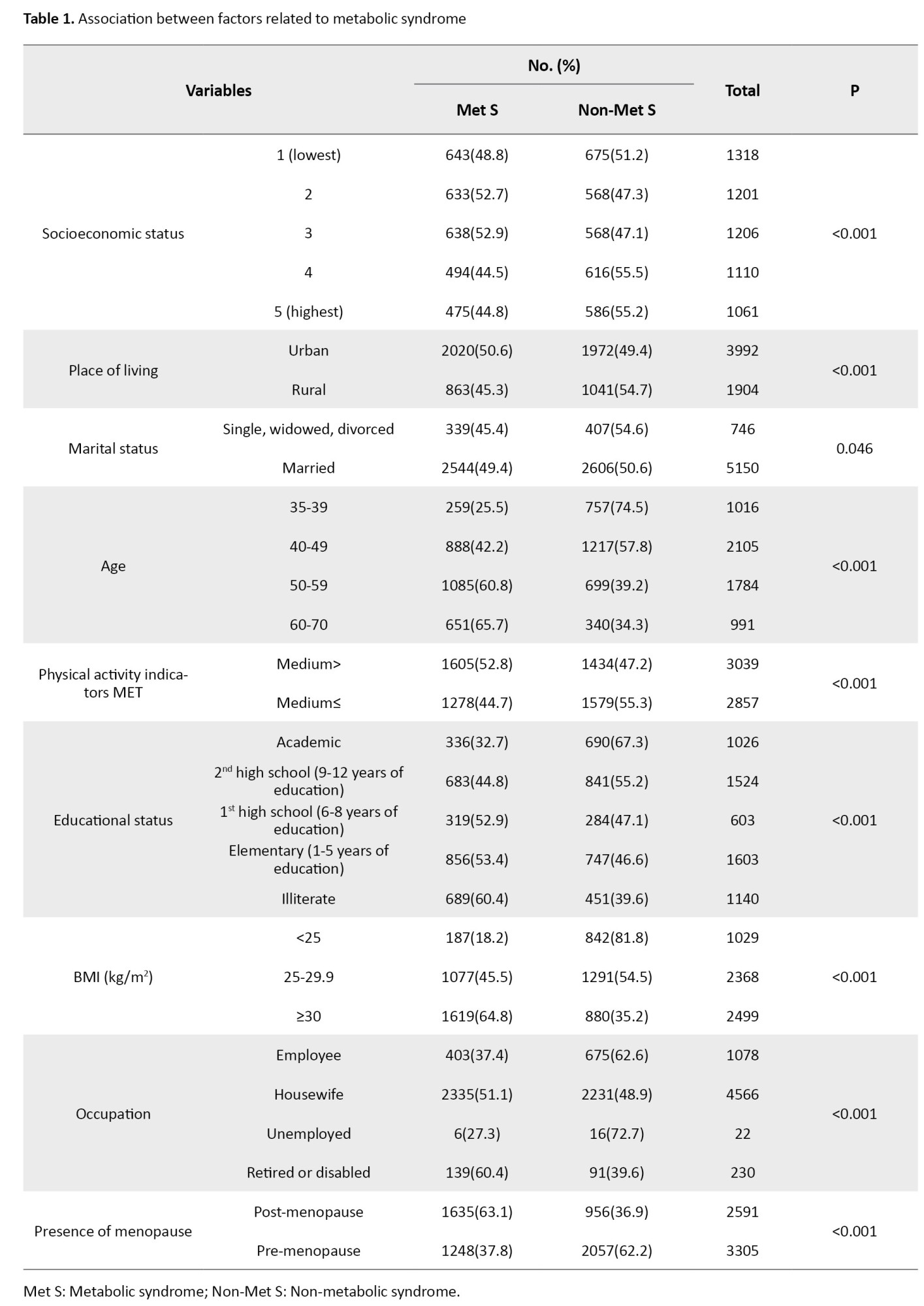
The association between metabolic syndrome and confounding variables (correlated) was examined using the chi-squared statistical test. Table 1 presents findings from the chi-square analysis indicating significant relationships between metabolic syndrome and several factors, including socioeconomic status (P<0.001), place of living (P<0.001), marital status (P=0.040), age (P<0.001), indicators of physical activity (metabolic equivalents [MET]) (P<0.001), educational status (P<0.001), BMI (P<0.001), occupational status (P<0.001) and presence of menopause (P<0.001).
To mitigate the influence of confounding variables, those variables that demonstrated a significant association with metabolic syndrome were incorporated into the logistic regression model, with a threshold P<0.2.
Therefore, the logistic regression model was designed with variables of presence or absence of menopause, age of post-menopause (quantitatively and qualitatively), natural menopause versus secondary menopause, as well as removing confounding variables, such as educational status, age (due to correlation with age of menopause), place of living, BMI, indicators of physical activity MET, socioeconomic status, and marriage.
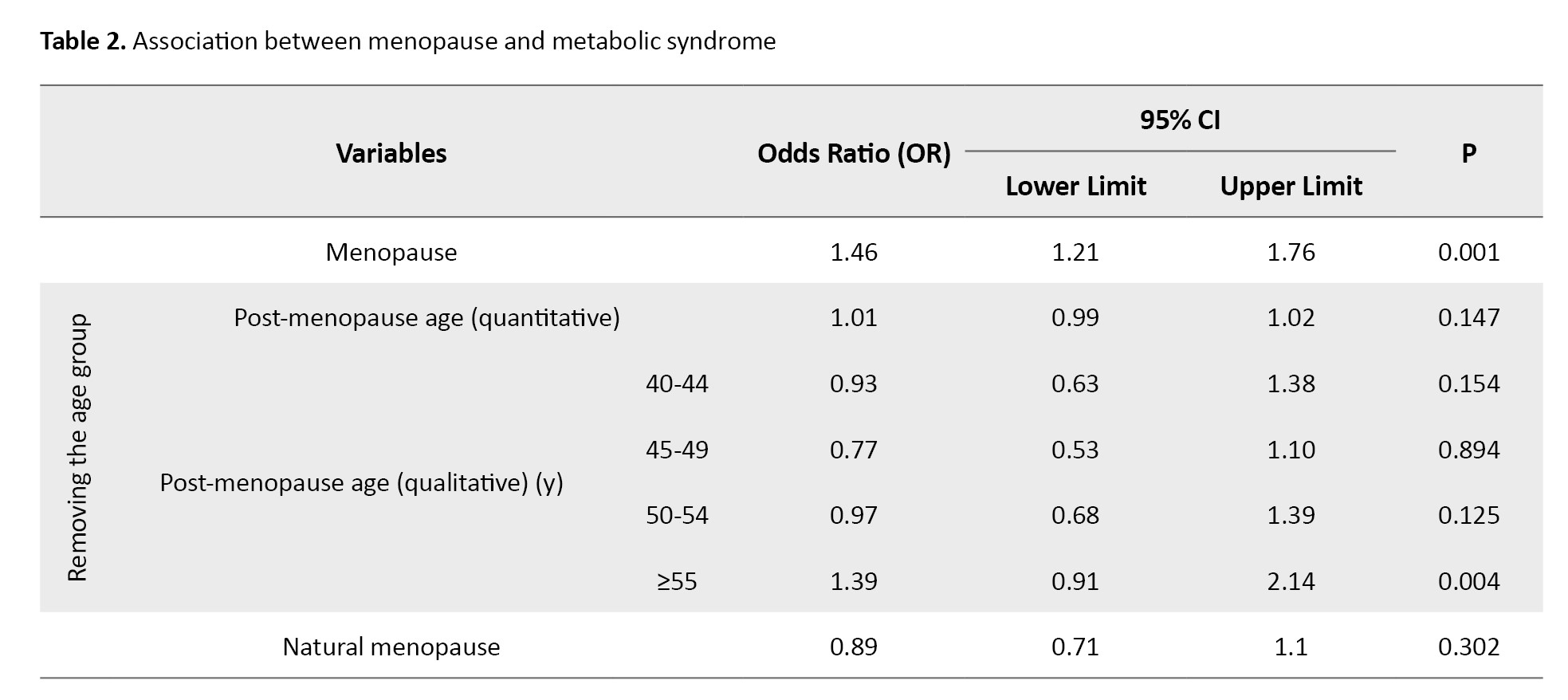
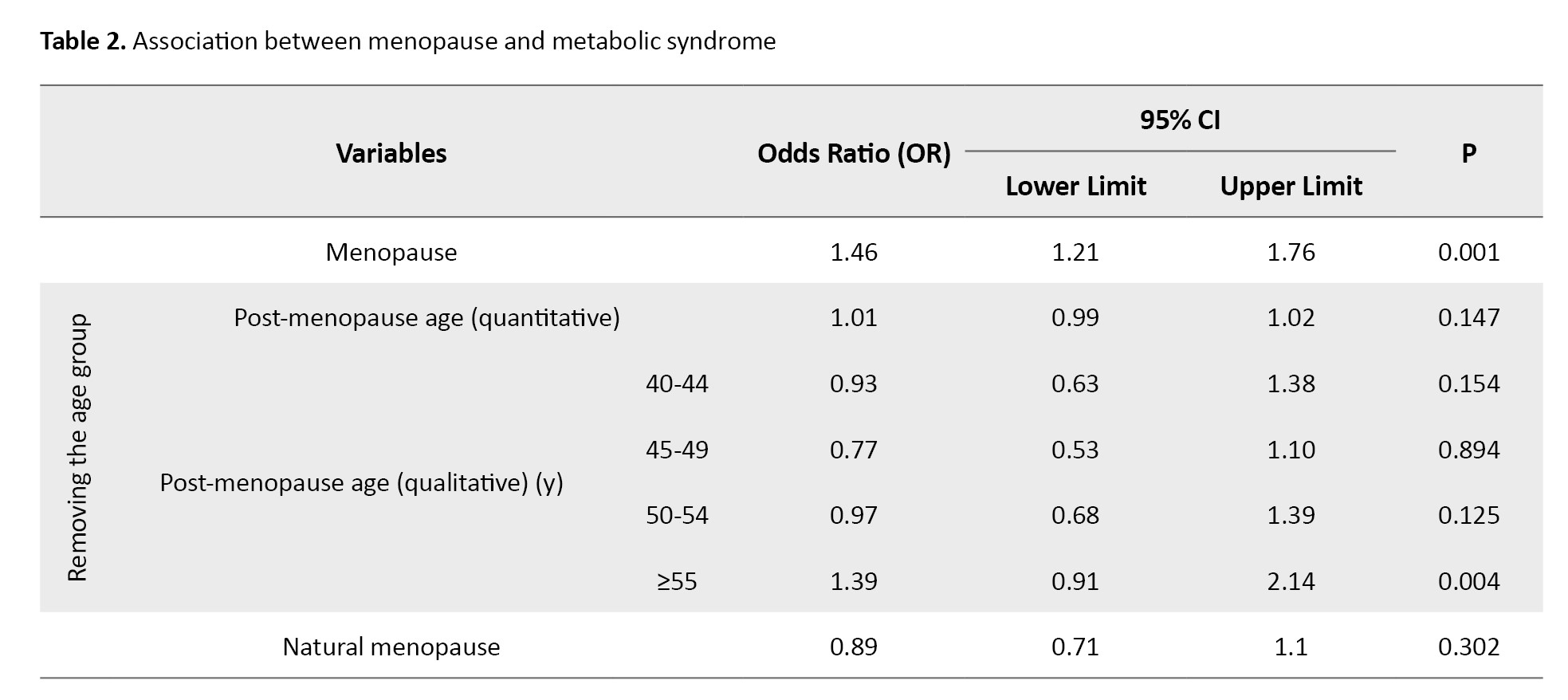
After removing confounding variables, the logistic regression model revealed a significant relationship between the presence of menopause and post-menopausal age equal to and greater than 55 years (qualitatively) and metabolic syndrome. Post-menopausal women were 1.46 times more at risk of metabolic syndrome than pre-menopausal women (P=0.001). Women aged 55 years and older had 1.39 times more chance of developing metabolic syndrome than women younger than 40 years (P=0.004). There was no significant relationship between post-menopausal age in quantitative form (P=0.147), post-menopausal age in qualitative form, the age range of 40-54 years (P>0.05), and natural menopause (P=0.302) with metabolic syndrome. The results relating to the logistic regression model are presented in Table 2.
Discussion
The present study investigated the association between menopause and metabolic syndrome based on the data from the enrollment phase of the TCS. The results showed that 78.5% of 2591 post-menopausal women (2033 women) had metabolic syndrome. The prevalence of metabolic syndrome was 65.13% in Brazilian cohort studies (with a population of 99 post-menopausal women) [22], 32.6% in Canada (with a population of 1035 post-menopausal women) [23], 25.4% in South Korea (with a population of 464 post-menopausal women) [24], 30% in Taiwan (with a population of 11484 post-menopausal women), 74.18% in non-cohort studies in Morocco (with a population of 213 post-menopausal women) [25] and 42% in India (with a population of 100 post-menopausal women) [2]. Different geographical locations and the non-uniformity of the studied population can account for the inconsistent findings reported in previous studies. Since low education and educational inequality in developing countries have increased the rate of metabolic syndrome [26], these countries should mainly focus on planning health policies to improve education and information about metabolic syndrome in post-menopausal women.
The data in the present study revealed a significant association between the presence of menopause and metabolic syndrome. Post-menopausal women were 1.46 times more at risk of metabolic syndrome compared to pre-menopausal women. Consistent with the data in the present study, a cohort study on 17460 Taiwanese women (11484 post-menopausal women and 5976 pre-menopausal women) also showed that the prevalence rates of metabolic syndrome in post-menopausal and pre-menopausal women were 30% versus 14%, respectively. Post-menopausal women had the chance of developing metabolic syndrome 1.17 times more than pre-menopausal women [27]. Furthermore, a cohort study in South Korea on 5275 women in the age range of 42-53 years (464 post-menopausal women and 1038 pre-menopausal women) showed that the metabolic syndrome indicators (blood pressure and diabetes) were 25.4% and 16.6% in post-menopausal and pre-menopausal women. Post-menopausal women had 3.90 times more chance of suffering from metabolic syndrome (blood pressure) than pre-menopausal women [24]. In addition, a systematic and meta-analysis review of 112 studies with a population of 95115 people (in the age range of 20 to 78 years) conducted globally from 2004 to 2017 reported the prevalence of metabolic syndrome in post-menopausal women to be 37.17%.
The results also indicate that the chance of developing metabolic syndrome in post-menopausal women is 3.54 times higher than in pre-menopausal women [28]. Since the studies reviewed above and the present study have addressed large sample sizes, their results have acceptable credibility. The rate of metabolic syndrome in post-menopausal women in the present study was higher than the rate reported in other studies. The focus on industrial growth in developing countries has neglected correct lifestyle education for post-menopausal women. The high prevalence of metabolic syndrome among adults aged 65-69, especially among women living in cities and older adults in Iran, is a matter of concern [29]. It seems that menopause plays a significant role in the development of metabolic syndrome. Although technology is currently a suitable tool for achieving lifestyle changes, it is ineffective compared to personal education [30]. As a result, changes should be made in the educational methods to improve their efficiency.
The findings from the present study showed that post-menopausal age equal to and greater than 55 years is significantly (qualitatively) associated with metabolic syndrome. Women aged 55 years and older had 1.39 times more chances of developing metabolic syndrome than women younger than 40 years. In line with the findings of the present study, another study in Iran (Shiraz Cohort Center) on 924 women over 40 years old (434 post-menopausal women and 490 pre-menopausal women) also shows the prevalence rates of metabolic syndrome as 51.2% and 30% in post-menopausal and pre-menopausal women. The findings also indicate that the risk of developing metabolic syndrome in post-menopausal women over 60 years is 4.8 times higher than in women under 40 years [31]. A study on 701 Indian women aged 35 to 66 (224 post-menopausal women and 274 pre-menopausal women) shows that the prevalence rates of metabolic syndrome are 55% and 45% in post-menopausal and pre-menopausal women, respectively. Moreover, women aged 56 years and older have 4.09 times more chances of developing metabolic syndrome than women aged less than 40 years [32]. A study in Brazil on 958 women (681 post-menopausal women and 277 pre-menopausal women) reports the prevalence rates of metabolic syndrome in post-menopausal and pre-menopausal women as 22.2% and 9.4%, respectively.
The results also reveal that with the increasing age of menopausal women, the incidence of metabolic syndrome increases, so that women aged 56-65 years have a 5.94 times higher chance of developing metabolic syndrome than women under 40 years [33]. In line with the findings from the present study, other studies have also suggested that the incidence of metabolic syndrome increases as the age of post-menopause increases [22, 25]. Since metabolic syndrome increases with inappropriate diet [34], inactivity [35], lack of physical activity [36] and sleep disorders [37], it seems that post-menopausal women are more exposed to the mentioned problems (inappropriate diet, inactivity, lack of physical activity and sleep disorders) due to increasing age. As a result, the risk of metabolic syndrome increases. Contrary to the present study, a study in Tehran City, Iran, on 639 women (418 post-menopausal women and 221 pre-menopausal women) in the age range of 40 to 60 years shows no statistically significant difference in terms of the prevalence of metabolic syndrome and age in the two groups of women and the prevalence rates of metabolic syndrome are 87.7% and 87.5% in post-menopausal and pre-menopausal women [38]. Another study in Iran on 140 post-menopausal women in Shiraz (2009) shows no significant relationship between age and metabolic syndrome indicators (except for fasting blood sugar) [39]. A study in South Korea on 892 post-menopausal women (in 2005) also shows no statistically significant relationship between the age of post-menopause and metabolic syndrome [40]. Since the reviewed studies were conducted 10-24 years ago, it can be concluded that, in addition to menopause, the passage of time would affect the prevalence of metabolic syndrome. The growing use of technology can affect people’s lifestyles and cause less mobility in people in different age groups, especially older adults. Thus, technological growth can be a reason for the increase in metabolic syndrome. A cohort study in Canada on 12611 women (10035 post-menopausal and 2576 pre-menopausal) aged 45-85 years shows that although the prevalence rates of metabolic syndrome are 36.2% and 20.5% in post-menopausal and pre-menopausal women, respectively, menopause was associated with an increased risk of metabolic syndrome independent of age [23]. It seems that in addition to the variations in the prevalence of metabolic syndrome in different geographical regions [10], public education and health in the prevention of diseases and metabolic syndrome is higher in developed countries than in developing countries.
A systematic and meta-analysis study conducted in 29 African countries on 156464 persons from 2004 to 2022 reported a higher occurrence of metabolic syndrome in women (36.9%) compared to men (26.7%) [41]. Furthermore, the prevalence of metabolic syndrome is significantly higher in women than in men over the age of 50 [42]. Even though pre-menopausal women may be protected against CVD, post-menopause increases the risk of CVD in them with the possibility of hormonal changes [43]. Physical changes during menopause, such as decreased insulin function, increased triglycerides [44, 45], estrogen deficiency, a relative increase in androgen levels and an increase in fat deposition in the abdominal area [45, 46], can be associated with some systemic metabolic disorders, exposing the person to the risk of CVD [46, 47]. Numerous studies have suggested that the range of metabolic syndrome indicators changes during menopause beyond the normal range [48, 49]. Thus, to reduce the incidence of metabolic syndrome and CVD in post-menopausal women, some health-promoting protocols and lifestyle modifications should be considered for this group of women.
Conclusion
In this study, 78.5% of post-menopausal women have metabolic syndrome. The data also show that the presence of menopause and increased age in women during post-menopause are significantly associated with metabolic syndrome. Hence, as a preventive healthcare solution, the necessary training should be provided to menopausal women. Although it is difficult to control all the risk factors of metabolic syndrome, the occurrence of metabolic syndrome can be prevented during menopause through lifestyle changes and periodic monitoring of women. Engaging in daily physical activity, losing weight, and quitting smoking are changes that can help lower blood pressure and balance blood sugar and fat levels. These changes can contribute to reducing the risk of metabolic syndrome.
Study limitations and suggestions
One of the strengths of the present study is using cohort phase data, which increased the accuracy of the data and findings. Participants were selected from only one region in Iran that was not representative of the entire population of the country, and the present study was a cross-sectional design, which has its limitations. Therefore, future studies with longitudinal design and larger sample sizes with follow-up methods are recommended.
Ethical Considerations
Compliance with ethical guidelines
This study was registered with the Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran (IR.MAZUMS. REC.1395.2524).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Study design and data collection: Seyed-Robabe Babaei; Statistical analysis: Mahmood Moosazadeh; Data collection: Motahareh Kheradmand and Amirsaeed Hosseini; Conceptualization, review and editing: Masoumeh Bagheri-Nesami; Reading and approval of the first and final drafts of the article: all authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Vice-Chancellor for Research and Technology of Mazandaran University of Medical Sciences and the Persian Cohort and Tabari Cohort members for their collaborations in conducting the research project.
Reference
Metabolic syndrome (also called syndrome X) is an insulin resistance syndrome. It involves a set of disorders in glucose metabolism, dyslipidemia, hypertension and central obesity that can predict the progression of cardiovascular diseases (CVD) and type 2 diabetes in the future [1, 2]. The international diabetes federation (IDF) and the adult treatment panel III (ATP III) guidelines have provided different definitions for the components of metabolic syndrome [3-5]. Numerous studies have suggested that metabolic syndrome is associated with an increased risk of coronary heart disease and heart attack [6] and an increase in deaths from CVDs by 3 to 5 times [7, 8]. The prevalence of metabolic syndrome is increasing worldwide. A systematic and meta-analysis study reported 36.9% and 34.6% prevalence rates for metabolic syndrome in Iran based on the ATP III and IDF criteria, respectively [9]. The prevalence of metabolic syndrome can be affected by various factors such as age, gender, family history, stress, inactivity, hormonal factors, malnutrition and the socioeconomic status of a community. These factors and their prevalence rates vary in different geographical areas [10]. One of the factors affecting the prevalence of metabolic syndrome is menopause. Menopause refers to the complete cessation of ovarian function, which occurs spontaneously (natural menopause) or iatrogenic (secondary menopause) [11]. The average age of women at menopause is 51 years, and only 4% of women experience natural menopause before the age of 40 [12]. Hot flashes, night sweats, vaginal atrophy, osteoporosis, psychiatric disorders, sexual dysfunction, skin lesions, CVD, cancer, metabolic disorders and obesity are the most obvious symptoms that occur in the menopausal age and continue until old age. These factors can adversely affect the quality of life of women [13]. A study conducted on Moroccan women showed that metabolic syndrome and abdominal obesity are more common in post-menopausal women than pre-menopausal women, and menopausal women with metabolic syndrome had at least three risk factors for this syndrome [14]. Studies conducted in the USA have found that the incidence of metabolic syndrome is higher in post-menopausal women than in pre-menopausal women [2]. Menopause induces lipid metabolism impairment and altered fatty acid synthesis, promoting insulin resistance, abdominal obesity and dyslipidemia, thereby increasing cancer risk [15, 16]. Concurrently, estrogen deficiency independently elevates hypertension susceptibility in postmenopausal women [17].
Given the high prevalence of metabolic syndrome, obesity, CVD and diabetes in recent years in the world, and also since no study has addressed metabolic syndrome and its relationship with menopause among women living in Mazandaran Province, Iran, the present study sought to examine the relationship between metabolic syndrome and menopause in the Tabari cohort population. The insights from this study can be used by health education experts and planners of the Ministry of Health, Treatment and Medical Education to develop future interventions and policies.
Material and Methods
The current study is a cross-sectional study conducted within the framework of the Tabari cohort study (TCS), and the data collected in the first phase of the study was used. TCS is a part of the national cohort study entitled prospective epidemiological research studies in Iran (Persian), the details of which are mentioned in other studies of the Tabari cohort [18-20]. The TCS recruited participants from June 2015 to November 2017 using a census-based sampling method. In urban regions, two health care volunteers identified eligible individuals, while health care workers facilitated enrollment in mountainous areas. Urban recruitment started from the right side of the cohort center. Recruitment in mountainous regions was conducted through household registries maintained at local health houses. From an initial pool of 12191 eligible urban residents, 7012 were included in the Tabari cohort. Similarly, among 4417 eligible individuals in mountainous areas, 3243 were enrolled. The first phase of TCS comprised 10255 participants aged 35–70 years (7012 urban and 3243 mountainous populations) from Sari City, Mazandaran Province, Iran.
Data were collected using a structured questionnaire standardized by the PERSIAN cohort team. Moreover, fasting blood samples (12-hour fast) were taken from all participants for laboratory tests. Fasting blood sugar, cholesterol level, triglyceride and high-density lipoprotein (HDL) cholesterol levels were measured using BT 1500 (Biotechnic, Italy). The blood pressure of all participants in the TCS was measured twice with an interval of 10 minutes using a Riester dial sphygmomanometer. Measurement of anthropometric indicators was done by trained personnel based on standard protocol [21].
The exclusion criteria of this study were cancer and kidney transplants. The sampling was performed using the census method; in the first phase of the Tabari cohort, 6106 women aged 35-70 were enrolled. Women who self-reported menopause and one year had passed since their last period were considered menopausal. According to the ATP III criteria, women who had at least three of the following were considered to have metabolic syndrome:
1) Waist circumference size more than 88 cm; 2) Triglyceride equal to or more than 150 mg/dL or drug use; 3) HDL cholesterol less than 50 mg/dL; 4) Hypertension, defined as a systolic blood pressure of 130 mm Hg or higher and a diastolic blood pressure of 85 mm Hg or higher, or receiving medication and 5) Hyperglycemia, characterized by a fasting blood sugar level of 100 mg/dL or higher or receiving medication [3, 5].
The demographic and medical information investigated in this study included age, sex, occupation, marital status, educational status, socioeconomic status, place of living, underlying disease, body mass index (BMI), metabolic syndrome indicators, menopause age, and its cause. Descriptive statistics such as Mean±SD and frequency were used to describe the variables. The chi-square test and logistic regression were used to determine the relationship between the two qualitative variables. The data were entered into SPSS software, version 21 for analysis. P≤0.05 was also considered significant.
Results
In the current study, 6106 women aged 35-70 were enrolled, of which 2591 were post-menopausal. Among post-menopausal women, 2033 participants (78.5%) had metabolic syndrome and 558 (21.5%) did not. The results of the chi-square test indicated no significant association between metabolic syndrome and factors such as the presence of menopause (P=0.181), age at menopause (P=0.058), natural menopause (P=0.27), unnatural menopause (P=0.69) and the type of menopause (natural versus unnatural) (P=0.181).
The association between metabolic syndrome and confounding variables (correlated) was examined using the chi-squared statistical test. Table 1 presents findings from the chi-square analysis indicating significant relationships between metabolic syndrome and several factors, including socioeconomic status (P<0.001), place of living (P<0.001), marital status (P=0.040), age (P<0.001), indicators of physical activity (metabolic equivalents [MET]) (P<0.001), educational status (P<0.001), BMI (P<0.001), occupational status (P<0.001) and presence of menopause (P<0.001).
To mitigate the influence of confounding variables, those variables that demonstrated a significant association with metabolic syndrome were incorporated into the logistic regression model, with a threshold P<0.2.
Therefore, the logistic regression model was designed with variables of presence or absence of menopause, age of post-menopause (quantitatively and qualitatively), natural menopause versus secondary menopause, as well as removing confounding variables, such as educational status, age (due to correlation with age of menopause), place of living, BMI, indicators of physical activity MET, socioeconomic status, and marriage.
After removing confounding variables, the logistic regression model revealed a significant relationship between the presence of menopause and post-menopausal age equal to and greater than 55 years (qualitatively) and metabolic syndrome. Post-menopausal women were 1.46 times more at risk of metabolic syndrome than pre-menopausal women (P=0.001). Women aged 55 years and older had 1.39 times more chance of developing metabolic syndrome than women younger than 40 years (P=0.004). There was no significant relationship between post-menopausal age in quantitative form (P=0.147), post-menopausal age in qualitative form, the age range of 40-54 years (P>0.05), and natural menopause (P=0.302) with metabolic syndrome. The results relating to the logistic regression model are presented in Table 2.
Discussion
The present study investigated the association between menopause and metabolic syndrome based on the data from the enrollment phase of the TCS. The results showed that 78.5% of 2591 post-menopausal women (2033 women) had metabolic syndrome. The prevalence of metabolic syndrome was 65.13% in Brazilian cohort studies (with a population of 99 post-menopausal women) [22], 32.6% in Canada (with a population of 1035 post-menopausal women) [23], 25.4% in South Korea (with a population of 464 post-menopausal women) [24], 30% in Taiwan (with a population of 11484 post-menopausal women), 74.18% in non-cohort studies in Morocco (with a population of 213 post-menopausal women) [25] and 42% in India (with a population of 100 post-menopausal women) [2]. Different geographical locations and the non-uniformity of the studied population can account for the inconsistent findings reported in previous studies. Since low education and educational inequality in developing countries have increased the rate of metabolic syndrome [26], these countries should mainly focus on planning health policies to improve education and information about metabolic syndrome in post-menopausal women.
The data in the present study revealed a significant association between the presence of menopause and metabolic syndrome. Post-menopausal women were 1.46 times more at risk of metabolic syndrome compared to pre-menopausal women. Consistent with the data in the present study, a cohort study on 17460 Taiwanese women (11484 post-menopausal women and 5976 pre-menopausal women) also showed that the prevalence rates of metabolic syndrome in post-menopausal and pre-menopausal women were 30% versus 14%, respectively. Post-menopausal women had the chance of developing metabolic syndrome 1.17 times more than pre-menopausal women [27]. Furthermore, a cohort study in South Korea on 5275 women in the age range of 42-53 years (464 post-menopausal women and 1038 pre-menopausal women) showed that the metabolic syndrome indicators (blood pressure and diabetes) were 25.4% and 16.6% in post-menopausal and pre-menopausal women. Post-menopausal women had 3.90 times more chance of suffering from metabolic syndrome (blood pressure) than pre-menopausal women [24]. In addition, a systematic and meta-analysis review of 112 studies with a population of 95115 people (in the age range of 20 to 78 years) conducted globally from 2004 to 2017 reported the prevalence of metabolic syndrome in post-menopausal women to be 37.17%.
The results also indicate that the chance of developing metabolic syndrome in post-menopausal women is 3.54 times higher than in pre-menopausal women [28]. Since the studies reviewed above and the present study have addressed large sample sizes, their results have acceptable credibility. The rate of metabolic syndrome in post-menopausal women in the present study was higher than the rate reported in other studies. The focus on industrial growth in developing countries has neglected correct lifestyle education for post-menopausal women. The high prevalence of metabolic syndrome among adults aged 65-69, especially among women living in cities and older adults in Iran, is a matter of concern [29]. It seems that menopause plays a significant role in the development of metabolic syndrome. Although technology is currently a suitable tool for achieving lifestyle changes, it is ineffective compared to personal education [30]. As a result, changes should be made in the educational methods to improve their efficiency.
The findings from the present study showed that post-menopausal age equal to and greater than 55 years is significantly (qualitatively) associated with metabolic syndrome. Women aged 55 years and older had 1.39 times more chances of developing metabolic syndrome than women younger than 40 years. In line with the findings of the present study, another study in Iran (Shiraz Cohort Center) on 924 women over 40 years old (434 post-menopausal women and 490 pre-menopausal women) also shows the prevalence rates of metabolic syndrome as 51.2% and 30% in post-menopausal and pre-menopausal women. The findings also indicate that the risk of developing metabolic syndrome in post-menopausal women over 60 years is 4.8 times higher than in women under 40 years [31]. A study on 701 Indian women aged 35 to 66 (224 post-menopausal women and 274 pre-menopausal women) shows that the prevalence rates of metabolic syndrome are 55% and 45% in post-menopausal and pre-menopausal women, respectively. Moreover, women aged 56 years and older have 4.09 times more chances of developing metabolic syndrome than women aged less than 40 years [32]. A study in Brazil on 958 women (681 post-menopausal women and 277 pre-menopausal women) reports the prevalence rates of metabolic syndrome in post-menopausal and pre-menopausal women as 22.2% and 9.4%, respectively.
The results also reveal that with the increasing age of menopausal women, the incidence of metabolic syndrome increases, so that women aged 56-65 years have a 5.94 times higher chance of developing metabolic syndrome than women under 40 years [33]. In line with the findings from the present study, other studies have also suggested that the incidence of metabolic syndrome increases as the age of post-menopause increases [22, 25]. Since metabolic syndrome increases with inappropriate diet [34], inactivity [35], lack of physical activity [36] and sleep disorders [37], it seems that post-menopausal women are more exposed to the mentioned problems (inappropriate diet, inactivity, lack of physical activity and sleep disorders) due to increasing age. As a result, the risk of metabolic syndrome increases. Contrary to the present study, a study in Tehran City, Iran, on 639 women (418 post-menopausal women and 221 pre-menopausal women) in the age range of 40 to 60 years shows no statistically significant difference in terms of the prevalence of metabolic syndrome and age in the two groups of women and the prevalence rates of metabolic syndrome are 87.7% and 87.5% in post-menopausal and pre-menopausal women [38]. Another study in Iran on 140 post-menopausal women in Shiraz (2009) shows no significant relationship between age and metabolic syndrome indicators (except for fasting blood sugar) [39]. A study in South Korea on 892 post-menopausal women (in 2005) also shows no statistically significant relationship between the age of post-menopause and metabolic syndrome [40]. Since the reviewed studies were conducted 10-24 years ago, it can be concluded that, in addition to menopause, the passage of time would affect the prevalence of metabolic syndrome. The growing use of technology can affect people’s lifestyles and cause less mobility in people in different age groups, especially older adults. Thus, technological growth can be a reason for the increase in metabolic syndrome. A cohort study in Canada on 12611 women (10035 post-menopausal and 2576 pre-menopausal) aged 45-85 years shows that although the prevalence rates of metabolic syndrome are 36.2% and 20.5% in post-menopausal and pre-menopausal women, respectively, menopause was associated with an increased risk of metabolic syndrome independent of age [23]. It seems that in addition to the variations in the prevalence of metabolic syndrome in different geographical regions [10], public education and health in the prevention of diseases and metabolic syndrome is higher in developed countries than in developing countries.
A systematic and meta-analysis study conducted in 29 African countries on 156464 persons from 2004 to 2022 reported a higher occurrence of metabolic syndrome in women (36.9%) compared to men (26.7%) [41]. Furthermore, the prevalence of metabolic syndrome is significantly higher in women than in men over the age of 50 [42]. Even though pre-menopausal women may be protected against CVD, post-menopause increases the risk of CVD in them with the possibility of hormonal changes [43]. Physical changes during menopause, such as decreased insulin function, increased triglycerides [44, 45], estrogen deficiency, a relative increase in androgen levels and an increase in fat deposition in the abdominal area [45, 46], can be associated with some systemic metabolic disorders, exposing the person to the risk of CVD [46, 47]. Numerous studies have suggested that the range of metabolic syndrome indicators changes during menopause beyond the normal range [48, 49]. Thus, to reduce the incidence of metabolic syndrome and CVD in post-menopausal women, some health-promoting protocols and lifestyle modifications should be considered for this group of women.
Conclusion
In this study, 78.5% of post-menopausal women have metabolic syndrome. The data also show that the presence of menopause and increased age in women during post-menopause are significantly associated with metabolic syndrome. Hence, as a preventive healthcare solution, the necessary training should be provided to menopausal women. Although it is difficult to control all the risk factors of metabolic syndrome, the occurrence of metabolic syndrome can be prevented during menopause through lifestyle changes and periodic monitoring of women. Engaging in daily physical activity, losing weight, and quitting smoking are changes that can help lower blood pressure and balance blood sugar and fat levels. These changes can contribute to reducing the risk of metabolic syndrome.
Study limitations and suggestions
One of the strengths of the present study is using cohort phase data, which increased the accuracy of the data and findings. Participants were selected from only one region in Iran that was not representative of the entire population of the country, and the present study was a cross-sectional design, which has its limitations. Therefore, future studies with longitudinal design and larger sample sizes with follow-up methods are recommended.
Ethical Considerations
Compliance with ethical guidelines
This study was registered with the Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran (IR.MAZUMS. REC.1395.2524).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Study design and data collection: Seyed-Robabe Babaei; Statistical analysis: Mahmood Moosazadeh; Data collection: Motahareh Kheradmand and Amirsaeed Hosseini; Conceptualization, review and editing: Masoumeh Bagheri-Nesami; Reading and approval of the first and final drafts of the article: all authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Vice-Chancellor for Research and Technology of Mazandaran University of Medical Sciences and the Persian Cohort and Tabari Cohort members for their collaborations in conducting the research project.
Reference
- Napoleone JM, Boudreau RM, Lange-Maia BS, El Khoudary SR, Ylitalo KR, Kriska AM, et al. Metabolic Syndrome Trajectories and Objective Physical Performance in Mid-to-Early Late Life: The Study of Women's Health Across the Nation (SWAN). The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2022; 77(2):e39-47. [DOI:10.1093/gerona/glab188] [PMID]
- Mehndiratta N, Sharma S, Sharma RK, Grover S. A prospective study on the incidence of metabolic syndrome in premenopausal and postmenopausal women. Journal of Mid-Life Health. 2020; 11(1):17-21. [DOI:10.4103/jmh.JMH_57_19] [PMID]
- Alberti KG, Zimmet P, Shaw J; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome-a new worldwide definition. The Lancet. 2005; 366(9491):1059-62. [DOI:10.1016/S0140-6736(05)67402-8] [PMID]
- Hajian-Tilaki K, Heidari B, Firouzjahi A, Bagherzadeh M, Hajian-Tilaki A, Halalkhor S. Prevalence of metabolic syndrome and the association with socio-demographic characteristics and physical activity in urban population of Iranian adults: A population-based study. Diabetes & Metabolic Syndrome. 2014; 8(3):170-6. [DOI:10.1016/j.dsx.2014.04.012] [PMID]
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005; 112(17):2735-52. [DOI:10.1161/CIRCULATIONAHA.105.169404] [PMID]
- Dun Y, Thomas RJ, Smith JR, Medina-Inojosa JR, Squires RW, Bonikowske AR, et al. High-intensity interval training improves metabolic syndrome and body composition in outpatient cardiac rehabilitation patients with myocardial infarction. Cardiovascular Diabetology. 2019; 18(1):140. [DOI:10.1186/s12933-019-0907-0] [PMID]
- Markopoulou P, Papanikolaou E, Analytis A, Zoumakis E, Siahanidou T. Preterm Birth as a Risk Factor for Metabolic Syndrome and Cardiovascular Disease in Adult Life: A Systematic Review and Meta-Analysis.The Journal of Pediatrics. 2019; 210:69-80.e5. [DOI:10.1016/j.jpeds.2019.02.041] [PMID]
- Fernández-Armenteros JM, Gómez-Arbonés X, Buti-Soler M, Betriu-Bars A, Sanmartin-Novell V, et al. Psoriasis, metabolic syndrome and cardiovascular risk factors. A population-based study. Journal of the European Academy of Dermatology and Venereology. 2019; 33(1):128-35. [DOI:10.1111/jdv.15159] [PMID]
- Naghipour M, Joukar F, Nikbakht HA, Hassanipour S, Asgharnezhad M, Arab-Zozani M, et al. High prevalence of metabolic syndrome and its related demographic factors in North of Iran: Results from the Persian Guilan cohort study. International Journal of Endocrinology. 2021; 2021:8862456. [DOI:10.1155/2021/8862456] [PMID]
- Gouveia HJCB, Urquiza-Martínez MV, Manhães-de-Castro R, Costa-de-Santana BJR, Villarreal JP, Mercado-Camargo R, et al. Effects of the Treatment with Flavonoids on Metabolic Syndrome Components in Humans: A systematic review focusing on mechanisms of action. International Journal of Molecular Sciences. 2022; 23(15):8344. [DOI:10.3390/ijms23158344] [PMID]
- Davis SR, Baber RJ. Treating menopause-MHT and beyond. Nature Reviews Endocrinology. 2022; 18(8):490-502. [DOI:10.1038/s41574-022-00685-4] [PMID]
- Sayahi M, Zakerkish M, Haghighizadeh MH, Ziagham S. [Relationship between menopausal symptoms, age, body mass index and metabolic syndrome in postmenopausal women in a number of health centers in Ahvaz in2013 (Persian)]. Journal of Arak University of Medical Sciences. 2015; 17(10):50-7. [Link]
- Stachowiak G, Pertyński T, Pertyńska-Marczewska M. Metabolic disorders in menopause. Przeglad Menopauzalny = Menopause review. 2015; 14(1):59-64. [DOI:10.5114/pm.2015.50000] [PMID]
- El Brini O, Akhouayri O, Benazzouz B. Metabolic Syndrome and Menopause are correlated in Moroccan women population. E3S Web of Conferences; 2021; 319(01058):1-6. [DOI:10.1051/e3sconf/202131901058]
- Ko SH, Kim HS. Menopause-associated lipid metabolic disorders and foods beneficial for postmenopausal women. Nutrients. 2020; 12(1):202. [DOI:10.3390/nu12010202] [PMID]
- Cao Z, Zheng X, Yang H, Li S, Xu F, Yang X, Wang Y. Association of obesity status and metabolic syndrome with site-specific cancers: A population-based cohort study. British Journal of Cancer. 2020; 123(8):1336-44. [DOI:10.1038/s41416-020-1012-6] [PMID]
- Morimoto S, Ichihara A. Late age at menopause positively associated with obesity-mediated hypertension. Hypertension Research. 2023; 46(5):1163-4. [DOI:10.1038/s41440-023-01237-7] [PMID]
- Kheradmand M, Moosazadeh M, Saeedi M, Poustchi H, Eghtesad S, Esmaeili R, et al. Tabari cohort profile and preliminary results in urban areas and mountainous regions of Mazandaran, Iran. Archives of Iranian Medicine. 2019; 22(6):279-85. [PMID]
- Eghtesad S, Mohammadi Z, Shayanrad A, Faramarzi E, Joukar F, Hamzeh B, et al. The PERSIAN cohort: Providing the evidence needed for healthcare reform. Archives of Iranian Medicine. 2017; 20(11):691-5. [PMID]
- Poustchi H, Eghtesad S, Kamangar F, Etemadi A, Keshtkar AA, Hekmatdoost A, et al. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): Rationale, objectives, and design. American Journal of Epidemiology. 2018; 187(4):647-55. [DOI:10.1093/aje/kwx314] [PMID]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Surveys (NHANES): Anthropometry procedure manual. California CreateSpace Independent Publishing Platform; 2014.
- Correia ES, Godinho-Mota JCM, Schincaglia RM, Martins KA, Martins JS, Vilella PR, et al. Metabolic Syndrome in postmenopausal women: Prevalence, sensibility, and specificity of adiposity indices. Clinical Nutrition Open Science. 2022; 41:106-14. [DOI:10.1016/j.nutos.2022.01.001]
- Christakis MK, Hasan H, De Souza LR, Shirreff L. The effect of menopause on metabolic syndrome: Cross-sectional results from the Canadian Longitudinal Study on Aging. Menopause. 2020; 27(9):999-1009. [DOI:10.1097/GME.0000000000001575] [PMID]
- Oh GC, Kang KS, Park CS, Sung HK, Ha KH, Kim HC, et al. Metabolic syndrome, not menopause, is a risk factor for hypertension in peri-menopausal women. Clinical Hypertension. 2018; 24:14. [DOI:10.1186/s40885-018-0099-z] [PMID]
- Harraqui K, Oudghiri DE, Hannoun Z, Naceiri Mrabti H, Aboulghras S, M. Assaggaf H, et al. Frequency of metabolic syndrome and study of anthropometric, clinical and biological characteristics in peri-and postmenopausal Women in the City of Ksar El Kebir (Northern Morocco). International Journal of Environmental Research and Public Health. 2022; 19(10):6109. [DOI:10.3390/ijerph19106109] [PMID]
- Gronner MF, Bosi PL, Carvalho AM, Casale G, Contrera D, Pereira MA, et al. Prevalence of metabolic syndrome and its association with educational inequalities among Brazilian adults: A population-based study. Brazilian Journal of Medical and Biological Research. 2011; 44(7):713-9. [DOI:10.1590/s0100-879x2011007500087] [PMID]
- Ou YJ, Lee JI, Huang SP, Chen SC, Geng JH, Su CH. Association between menopause, postmenopausal hormone therapy and metabolic syndrome. Journal of Clinical Medicine. 2023; 12(13):4435. [DOI:10.3390/jcm12134435] [PMID]
- Hallajzadeh J, Khoramdad M, Izadi N, Karamzad N, Almasi-Hashiani A, Ayubi E, et al. Metabolic syndrome and its components in premenopausal and postmenopausal women: A comprehensive systematic review and meta-analysis on observational studies. Menopause. 2018; 25(10):1155-64. [DOI:10.1097/GME.0000000000001136] [PMID]
- Tabatabaei-Malazy O, Saeedi Moghaddam S, Rezaei N, Sheidaei A, Hajipour MJ, Mahmoudi N, et al. A nationwide study of metabolic syndrome prevalence in Iran; a comparative analysis of six definitions. Plos One. 2021; 16(3):e0241926. [DOI:10.1371/journal.pone.0241926] [PMID]
- Bassi N, Karagodin I, Wang S, Vassallo P, Priyanath A, Massaro E, et al. Lifestyle modification for metabolic syndrome: A systematic review. The American Journal of Medicine. 2014; 127(12):1242.e1-10. [DOI:10.1016/j.amjmed.2014.06.035] [PMID]
- Maharlouei N, Bellissimo N, Ahmadi SM, Lankarani KB. Prevalence of metabolic syndrome in pre-and postmenopausal Iranian women. Climacteric. 2013; 16(5):561-7. [DOI:10.3109/13697137.2012.727504] [PMID]
- Pandey S, Srinivas M, Agashe S, Joshi J, Galvankar P, Prakasam C, et al. Menopause and metabolic syndrome: A study of 498 urban women from western India. Journal of Mid-Life Health. 2010; 1(2):63-9. [DOI:10.4103/0976-7800.76214] [PMID]
- Marchi R, Dell'Agnolo CM, Lopes TCR, Gravena AAF, Demitto MO, Brischiliari SCR, et al. Prevalence of metabolic syndrome in pre-and postmenopausal women. Archives of Endocrinology and Metabolism. 2017; 61(2):160-6. [DOI:10.1590/2359-3997000000253] [PMID]
- Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care. 2010; 33(11):2477-83. [DOI:10.2337/dc10-1079] [PMID]
- Wu J, Zhang H, Yang L, Shao J, Chen D, Cui N, et al. Sedentary time and the risk of metabolic syndrome: A systematic review and dose-response meta-analysis. Obesity Reviews. 2022; 23(12):e13510. [DOI:10.1111/obr.13510] [PMID]
- Cleven L, Krell-Roesch J, Schmidt SCE, Dziuba A, Bös K, Jekauc D, et al. Longitudinal association between physical activity and the risk of incident metabolic syndrome in middle-aged adults in Germany. Scientific Reports. 2022; 12(1):19424. [DOI:10.1038/s41598-022-24052-5] [PMID]
- Smiley A, King D, Bidulescu A. The association between sleep duration and metabolic syndrome: The NHANES 2013/2014. Nutrients. 2019; 11(11):2582. [DOI:10.3390/nu11112582] [PMID]
- Nakhjavani M, Imani M, Larry M, Aghajani-Nargesi A, Morteza A, Esteghamati A. Metabolic syndrome in premenopausal and postmenopausal women with type 2 diabetes: Loss of protective effects of premenopausal status. Journal of Diabetes & Metabolic Disorders. 2014; 13(1):102. [DOI:10.1186/s40200-014-0102-5] [PMID]
- Ziaei S, Ziagham S, Sayahi M. [Relationship between menopausal age and metabolic syndrome in non-obese postmenopausal women (Persian)]. Journal of Arak University of Medical Sciences. 2013;16(5):41-8. [Link]
- Cho GJ, Park HT, Shin JH, Kim T, Hur JY, Kim YT, et al. The relationship between reproductive factors and metabolic syndrome in Korean postmenopausal women: Korea National Health and Nutrition Survey 2005. Menopause. 2009; 16(5):998-1003. [DOI:10.1097/gme.0b013e3181a03807] [PMID]
- Bowo-Ngandji A, Kenmoe S, Ebogo-Belobo JT, Kenfack-Momo R, Takuissu GR, Kengne-Ndé C, et al. Prevalence of the metabolic syndrome in African populations: A systematic review and meta-analysis. Plos One. 2023; 18(7):e0289155. [DOI:10.1371/journal.pone.0289155] [PMID]
- Kim HM, Kim DJ, Jung IH, Park C, Park J. Prevalence of the metabolic syndrome among Korean adults using the new International Diabetes Federation definition and the new abdominal obesity criteria for the Korean people. Diabetes Research and Clinical Practice. 2007; 77(1):99-106. [DOI:10.1016/j.diabres.2006.10.009] [PMID]
- Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. The Journal of the Association of Physicians of India. 2009; 5):163-70. [PMID]
- Barroso TA, Marins LB, Alves R, Gonçalves ACS, Barroso SG, Rocha GdS. Association of central obesity with the incidence of cardiovascular diseases and risk factors. International Journal of Cardiovascular Sciences. 2017; 30(05):416-24. [DOI:10.5935/2359-4802.20170073]
- Hong SC, Yoo SW, Cho GJ, Kim T, Hur JY, Park YK, et al. Correlation between estrogens and serum adipocytokines in premenopausal and postmenopausal women. Menopause. 2007; 14(5):835-40. [DOI:10.1097/gme.0b013e31802cddca] [PMID]
- Meirelles RM. [Menopause and metabolic syndrome (Portuguese)]. Arquivos Brasileiros de Endocrinologia e Metabologia. 2014; 58(2):91-6. [DOI:10.1590/0004-2730000002909] [PMID]
- Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabetic Medicine. 2006; 23(5):469-80. [DOI:10.1111/j.1464-5491.2006.01858.x] [PMID]
- Sahin GT, Salman S, Ayanoglu YT, Sarıtaş DG, Tuna G. Prevalence of metabolic syndrome and effect of hormone profile in postmenopausal patients. JAREM Journal of Academic Research in Medicine. 2016; 6(1):35-41. [DOI:10.5152/jarem.2016.910]
- Marjani A, Moghasemi S. The metabolic syndrome among postmenopausal women in Gorgan. International Journal of Endocrinology. 2012; 2012:953627. [DOI:10.1155/2012/953627] [PMID]
Type of Study: Original Article |
Subject:
Epidemiology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |