Volume 13, Issue 1 (Winter 2025)
Iran J Health Sci 2025, 13(1): 23-30 |
Back to browse issues page
Ethics code: XU REC Package No. NSG-2023001290
Clinical trials code: N/A
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Enguio R K, Espinosa Z, Fallarna A J, Galarrita F G, Guillermo J J, Gutoc J, et al . Factors Influencing Measles Vaccine Compliance: A Descriptive-correlational Study in Barangay C, Northern Mindanao. Iran J Health Sci 2025; 13 (1) :23-30
URL: http://jhs.mazums.ac.ir/article-1-999-en.html
URL: http://jhs.mazums.ac.ir/article-1-999-en.html
Rhy Kenji Enguio 
 , Zenju Espinosa
, Zenju Espinosa 
 , Ashley Jenn Fallarna
, Ashley Jenn Fallarna 
 , Ferdinand Gabriel Galarrita
, Ferdinand Gabriel Galarrita 
 , Justine Jean Guillermo
, Justine Jean Guillermo 
 , Jasimah Gutoc
, Jasimah Gutoc 
 , Rhea Mae Janolino
, Rhea Mae Janolino 
 , Aleks Jimenez
, Aleks Jimenez 
 , Kayle Mae Labasano
, Kayle Mae Labasano 
 , Jade Godwin Lagua
, Jade Godwin Lagua 
 , Ariel Lacdo-O
, Ariel Lacdo-O 
 , Edmund Zheen Regor Moreno
, Edmund Zheen Regor Moreno 
 , Paolo Araune *
, Paolo Araune * 

 , Ivy Go
, Ivy Go 


 , Zenju Espinosa
, Zenju Espinosa 
 , Ashley Jenn Fallarna
, Ashley Jenn Fallarna 
 , Ferdinand Gabriel Galarrita
, Ferdinand Gabriel Galarrita 
 , Justine Jean Guillermo
, Justine Jean Guillermo 
 , Jasimah Gutoc
, Jasimah Gutoc 
 , Rhea Mae Janolino
, Rhea Mae Janolino 
 , Aleks Jimenez
, Aleks Jimenez 
 , Kayle Mae Labasano
, Kayle Mae Labasano 
 , Jade Godwin Lagua
, Jade Godwin Lagua 
 , Ariel Lacdo-O
, Ariel Lacdo-O 
 , Edmund Zheen Regor Moreno
, Edmund Zheen Regor Moreno 
 , Paolo Araune *
, Paolo Araune * 

 , Ivy Go
, Ivy Go 

Department of Mathematics, Xavier University-Ateneo de Cagayan, Cagayan de Oro, Philippines. , paraune@xu.edu.ph
Full-Text [PDF 699 kb]
(287 Downloads)
| Abstract (HTML) (555 Views)
Full-Text: (276 Views)
Introduction
Measles, characterized as an acute viral respiratory illness, poses a significant threat due to its highly contagious nature. Despite the availability of a safe and effective vaccine, measles has remained a prominent cause of mortality among young children worldwide, as noted by the World Health Organization (WHO) [1].
In the first two months of 2022, the global tally of reported measles cases surged by 79% compared to the corresponding period in 2021, as reported by the United Nations Children's Fund (UNICEF) [2]. This escalation was an early indicator of deficiencies in global immunization coverage. To address this shortfall, efforts led by WHO, in collaboration with UNICEF and other organizations, persisted in implementing programs to promote adherence to and supplying vaccines such as measles, mumps, and rubella (MMR) to various regions worldwide [2].
The inclusion of the MMR vaccine in Republic Act No. 10152, commonly known as the mandatory infants and children health immunization act of 2011, underscores the significance of immunization programs influenced by the Expanded Program on Immunization (EPI) [2]. This legislation mandates primary immunization against vaccine-preventable diseases for all children under five years old. As a result of this mandated law, the country experienced unprecedented success in reducing measles cases and fatalities for nearly two decades.
However, Hotez et al. highlighted a resurgence in measles transmission in the Philippines, attributing vaccine hesitancy as the primary cause [3]. A study by Domai et al. [4] revealed that the most substantial measles outbreak in the Western Pacific region, as designated by the WHO, occurred in the Philippines. This outbreak coincided with a decline in first-dose measles-containing vaccine coverage to 75% in 2018, as reported by the same study [4].
Moreover, the Philippine News Agency (PNA) [5] reported that measles cases had reached 289 in Northern Mindanao, with 38 cases, including three deaths, coming from the city of Cagayan de Oro. According to Luis [5], the City Health Office disclosed that most measles cases were in the barangays of Carmen, Lapasan, Cugman, and Balulang. Although the non-communicable diseases department had not declared an outbreak, it continually urged parents to be informed about vaccines.
Besides the increasing cases, the COVID-19 pandemic disrupted the delivery of routine immunization services, especially during the enhanced community quarantine in the Philippines. According to the study by Kurukkal [6], the ongoing pandemic has disrupted the delivery of childhood vaccines by increasing parents’ anxiety about exposing their children to COVID-19, leading them to keep their children well away from clinics. Additionally, healthcare workers were also reassigned from routine immunizations to COVID-19 vaccinations.
With all the mentioned determinants affecting the delivery of routine immunization services, the researchers of the study further investigated the factors affecting vaccine compliance, specifically measles inoculation in a selected barangay in Northern Mindanao, Philippines, called barangay C (for anonymity). The said barangay was the fifth barangay in the city with the largest population and was one of the adopted communities of Xavier University-Ateneo de Cagayan. Furthermore, since no studies were investigating the factors affecting vaccine compliance in the said research locale, the researchers aimed to address this gap.
The independent variables, including age, decision-maker, and educational attainment, were hypothesized to have impacted the dependent variable, the respondents’ measles vaccine compliance level. This study determined the factors influencing measles vaccine compliance among respondents in a selected barangay of a particular city in northern Mindanao. Additionally, it aimed to ascertain if there was a significant difference in the level of measles vaccine compliance when grouped according to age, decision-maker of the family, and educational attainment.
Material and Methods
Study design
The study employed a non-experimental quantitative research design, precisely the descriptive-correlational approach. This design allows for the observation and collection of data on the natural relationships between factors influencing measles vaccination compliance among families. The descriptive-correlational approach facilitates the identification of associations between dependent and independent variables without manipulating the variables, and therefore, no causal inferences are made [7].
Sample, sample size, sampling technique
The study was conducted in barangay C, one of the university’s partnered barangays, with the highest population of families with children under 5. Barangay C was chosen to ensure adequate representation of families with young children, a critical factor for the research. According to the 2020 census, barangay C had a population of 35238, representing 4.84% of the region’s total population [8]. The final research setting was selected based on its high concentration of families with children under five years old.
The respondents were selected based on the following criteria: residents aged 18 to 59 years, residing in the selected zone for at least six months, with children under five years old who had not received the first or second dose of the measles vaccine, had received only one dose or had received both doses. Additionally, the primary decision-makers of these families, regardless of educational attainment, were included in the study.
The researchers used the Cochran formula for sample size calculation to determine the ideal sample size. Assuming a household population (N) of 200 with children aged 0-5 years old in the selected zone, a 95% confidence level (z=1.96), a margin of error (e) of 0.05, and a variability (p) of 0.5, the calculated sample size was 132 respondents (n). This sample size was deemed sufficient for statistical power and to minimize sampling error.
Simple random sampling was employed to select participants from the identified households. As described by Thomas [9], simple random sampling is a primary probability sampling method where each individual in the population has an equal chance of being selected. This technique ensured strong internal and external validity and minimized selection and sampling biases, increasing the reliability and generalizability of the study’s findings.
Data collection process
For the data-gathering procedure, the researchers sent a letter of intent to the City Health Officer to obtain permission to access data from the chosen barangay’s primary health center and conduct the study. Upon receiving approval from the city health officer, the researchers, under the supervision of the barangay health nurse, were granted access to the list of zones of the chosen barangay and its corresponding residents.
The instrument of data collection
The researchers utilized a researcher-made questionnaire to gather primary data on factors influencing measles vaccine compliance, which was divided into two sections. The first section collected demographic information in a checklist format, including age, decision-maker, and educational attainment. The second section assessed factors influencing vaccine compliance using a 4-point Likert scale, categorized into psychosocial factors and behavioral-specific cognitions. To ensure validity, the questionnaire was reviewed by health experts familiar with the relevant factors, and a pilot test was conducted with a small sample from a different barangay to refine the instrument. The Cronbach α for the overall questionnaire was 0.85, indicating good internal consistency, with values of 0.80 for psychosocial factors and 0.82 for behavioral-specific cognitions, demonstrating acceptable reliability. Informed consent forms were provided, and respondents were oriented in both English and Bisaya to ensure a clear understanding of the study.
Data analysis
The t-test and analysis of variance (ANOVA)/F-tests were utilized to achieve the study’s objective. The t-test examined the significance of mean differences among various age groups, considering their variance or distribution, thereby measuring the magnitude of these differences. Additionally, the researchers applied ANOVA to ascertain any significant disparities in mean profiles concerning the family’s decision-maker and educational attainment. Subsequently, F tests were conducted to assess the statistical equality of means.
Results
A total of 132 respondents, aged 18 to 59 years, participated in the study. Most participants were female (65%) and served as the primary decision-makers in their households (80%). Most respondents had children under five years old, with a significant proportion having received at least one dose of the measles vaccine, while others had completed the full vaccination schedule.
Table 1 presents the differences in measles vaccine compliance based on age.
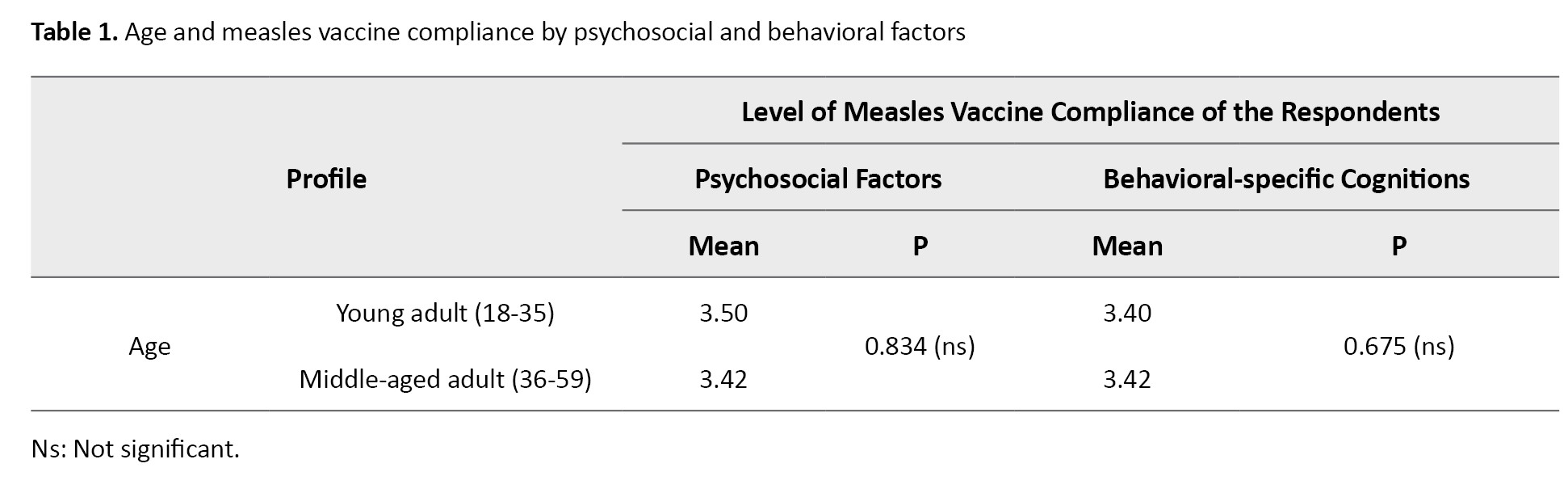
Younger adults (18-35 years) exhibited slightly higher compliance levels in psychosocial factors (mean=3.50) compared to middle-aged adults (36-59 years, mean=3.42). Conversely, middle adults showed slightly higher compliance regarding behavioral-specific cognitions (mean=3.42) than younger adults (mean=3.40). The t-test was performed to assess these differences, with P of 0.834 for psychosocial factors and 0.675 for behavioral-specific cognitions. Since both P exceeded the threshold of 0.05, the null hypothesis was accepted, suggesting no significant difference in measles vaccine compliance between younger and middle adults when grouped by age.
The underlying assumptions of the t-test, including the data’s normality and the variances’ homogeneity, were examined. The Shapiro-Wilk test was performed for normality, and the results showed no significant deviation from normality (P>0.05) for both psychosocial factors and behavioral-specific cognitions. The Levene’s test for equality of variances showed no significant differences in variances across the groups (P>0.05), supporting the validity of the t-test results.
Table 2 explores how the decision-maker in the household influences vaccine compliance.
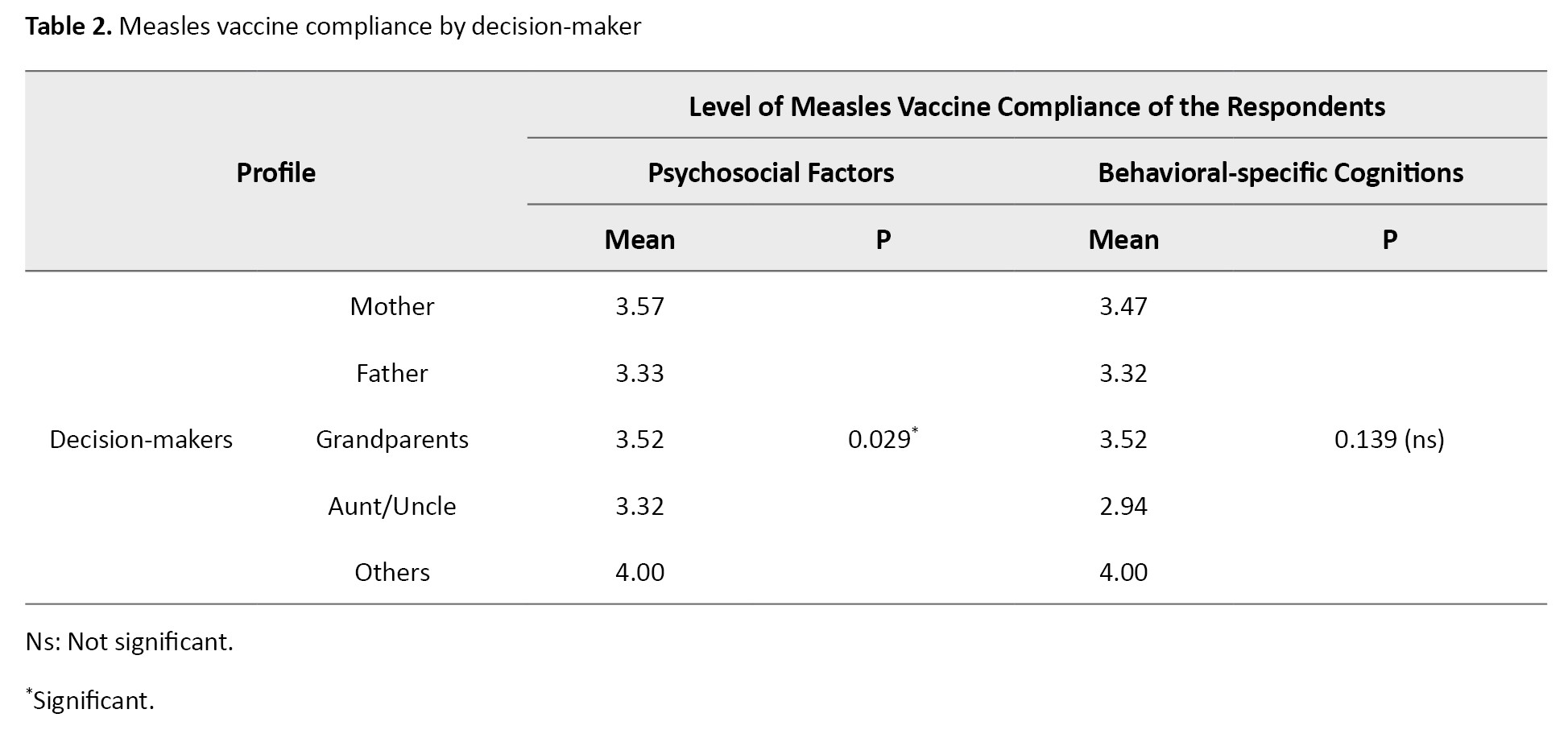
Mothers exhibited the highest compliance in psychosocial factors (mean=3.57) compared to other decision-makers. This condition highlights the significant role that psychological factors and social-cultural contexts may play in mothers’ decisions regarding vaccination. The ANOVA showed a significant P of 0.029 for psychosocial factors, indicating a statistically significant difference between decision-makers. However, the P for behavioral-specific cognitions (0.139) was above 0.05, indicating no significant difference in this domain.
The assumptions for the ANOVA test were also checked. The data met the normality assumption, with the Shapiro-Wilk test indicating no significant departure from normality (P>0.05) for both psychosocial factors and behavioral-specific cognitions. Homogeneity of variances was confirmed using Levene’s test (P=0.617 for psychosocial factors and P=0.838 for behavioral-specific cognitions), supporting the validity of the ANOVA results.
Table 3 examines measles vaccine compliance by respondents’ highest educational attainment.
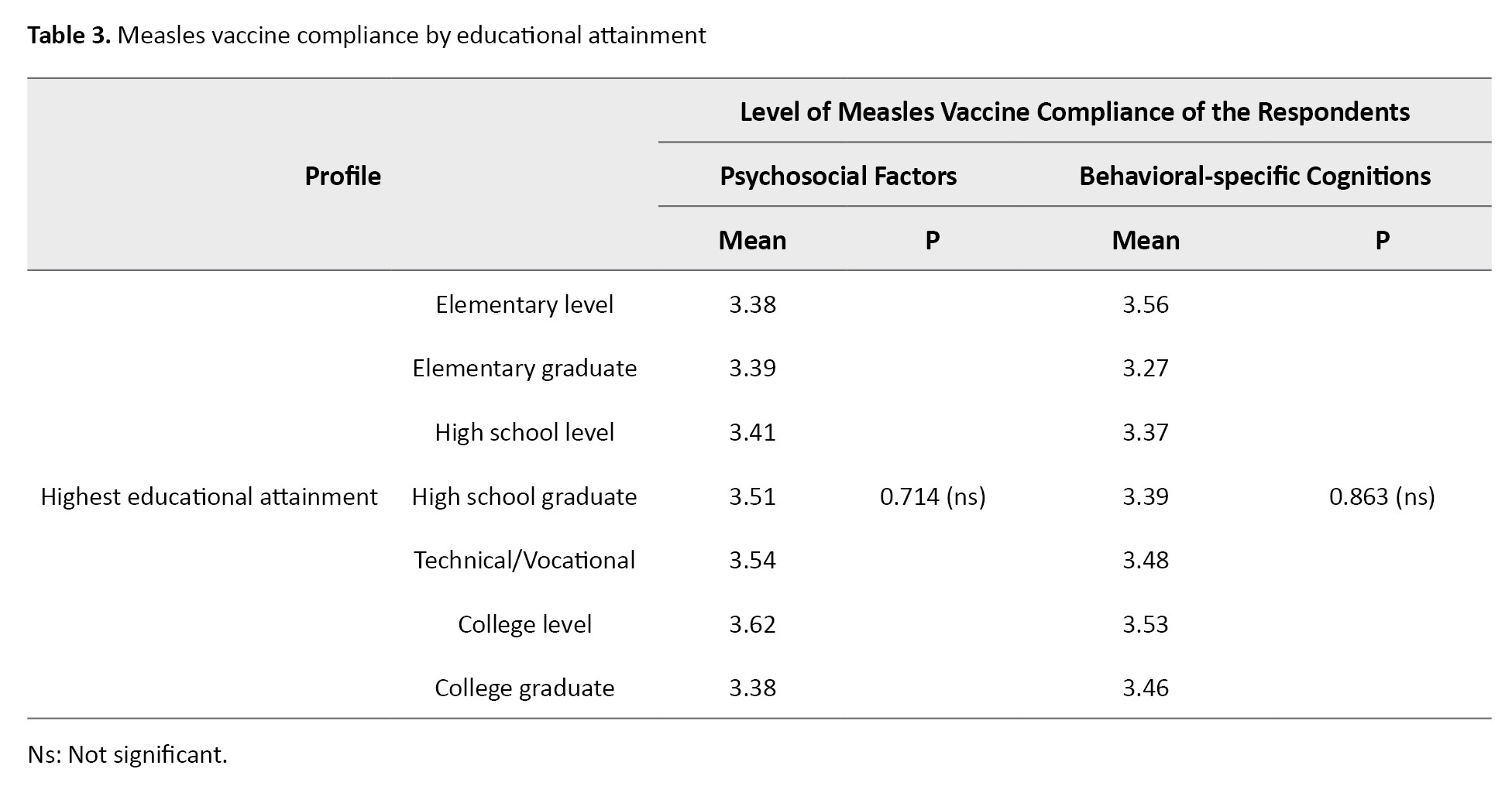
For psychosocial factors, individuals with some college education (mean=3.62) showed the highest compliance levels, suggesting that psychological and social contexts may be particularly influential at this education level. Interestingly, decision-makers with only elementary education (mean=3.56) had the highest compliance for behavioral-specific cognitions, possibly indicating that their perceptions, behavior, and motivation were influential in their vaccine compliance. ANOVA results for both psychosocial factors (P=0.714) and behavioral-specific cognitions (P=0.863) showed no significant differences across educational attainment groups, as both P exceeded 0.05.
As with Table 2, the assumptions for the ANOVA test were tested. Normality was confirmed through the Shapiro-Wilk test (P>0.05), and homogeneity of variance was validated with Levene’s test (P=0.746 for psychosocial factors and P=0.648 for behavioral-specific cognitions), ensuring that the assumptions of the test were met.
These findings suggest that factors such as the decision-maker’s role in the household and age may influence measles vaccine compliance, though differences in educational attainment did not significantly impact compliance levels. The lack of statistically significant differences in some areas calls for further exploration of additional variables that might affect vaccine uptake.
Discussion
A higher level of compliance concerning psychosocial factors was observed among younger adults, implying that self-motivation, perceived health status, definition of health, education, and cultural or religious beliefs greatly influence them. This result also indicated that younger adult respondents tended to rely more on their competence regarding measles vaccine adherence.
On the other hand, middle-aged individuals exhibited greater adherence to behavioral-specific cognitions, suggesting that factors such as perceived benefits of action, perceived barriers to action, perceived self-efficacy, activity-related effect, interpersonal influences, and situational influences significantly influenced their compliance with routine measles vaccination. This finding also implies that middle-aged respondents are more susceptible to the influence of their social circles when making decisions regarding measles vaccination compliance.
According to the study by Shati et al. [10], parents aged 20-30 believed that vaccination may not pose more risk to children than adults, leading to higher vaccine compliance among children with younger adult parents. However, Lampkin [11] stated that more than half of persons over 50 reported not knowing whom to believe regarding vaccine information. Additionally, Migriño et al. [12] supported the findings from this Table, which stated no significant associations between reasons for vaccine refusal and the respondents’ demographic data, such as their age.
The high level of compliance regarding psychosocial factors among the respondents, specifically the mothers, can be attributed to the nature of Filipino households. Filipino culture often strongly emphasizes the role of mothers as caregivers and nurturers. This cultural expectation further contributed to mothers’ heightened awareness and responsibility regarding their children’s health, including vaccine compliance. The pressure to fulfill societal expectations has increased vigilance and motivation among the respondents to ensure their children’s well-being, including adherence to vaccination schedules.
Moreover, Filipino mothers tended to have strong social support networks, including extended family members, friends, and fellow mothers in their communities. These networks play a significant role in shaping attitudes, beliefs, and behaviors related to vaccines. Social support provided validation, information sharing, and reinforcement of vaccine compliance practices. The influence of social networks on mothers’ compliance was pronounced due to their active engagement in the community or their close relationship with fellow mothers.
These findings are consistent with the results of a cross-sectional survey of parents in Italy by Della Polla et al. [13]. The study found that mothers were more likely to have positive attitudes toward HPV vaccination than fathers, which predicted their children’s vaccination status. Moreover, this study observed that parents’ attitudes toward the vaccine tended to be affected by their knowledge and awareness of the HPV vaccine, indicating the significant role of psychosocial factors in affecting adherence to vaccinations.
Another study supporting the importance of psychosocial factors is the review by Balgovind and Mohammadnezhad [14]. From the 44 studies they reviewed, factors affecting childhood immunization were identified and summarized into four themes: Parental knowledge, attitudes, and beliefs about vaccines. Furthermore, it shows that parents with limited knowledge about vaccines are less likely to be compliant or have a positive attitude toward vaccines, which is similar to the findings of this study, except that the respondents in this study displayed a more positive attitude, hence a higher level of compliance.
Regarding Nola Pender’s Health Promotion Model [15], the findings agree that a person’s psychological traits and sociocultural characteristics can significantly shape their health-promoting behaviors, which, in this study, involved compliance or adherence to vaccination recommendations. Mothers’ characteristics, such as their knowledge, beliefs, attitudes, and past experiences, influence their vaccine compliance. Their social environment and interactions with others also played a crucial role, as supported by Nola Pender’s propositions [16]. Psychosocial factors indeed played a role in the health-promoting behaviors of mothers.
Although the results indicated no significant difference in the respondents’ measles vaccine compliance level when grouped according to decision-makers regarding behavioral-specific cognitions, it showed that grandparents had the highest mean. This finding indicated that overall perceptions, behavior, and motivation were significant factors in the measles vaccine compliance of grandparents as decision-makers.
Similarly, in a study by Skitarelić et al. [16], wherein attitudes about childhood vaccinations between parents and grandparents were investigated and compared, it was observed that grandparents preferred children’s health benefits as a reason for vaccination by 9.19% more than parents. Furthermore, grandparents displayed less fear and suspicion toward vaccines than younger parents.
Upon examining the results, it was found that guardians who attended college but did not graduate exhibited higher compliance toward immunizing their children than those who graduated, particularly regarding psychosocial factors. Maybe these individuals spent much more time at home, whereas those who graduated pursued job opportunities, resulting in their time being occupied.
According to a study by Nguyen et al. [17], vaccine compliance hesitancy was higher among mothers who completed high school than those who attained a college education level. This trend was attributed to the higher educational exposure of college-aged individuals. College students typically have better access to information and possess enhanced health literacy, motivating them to make informed health decisions, particularly regarding their children’s health [18]. This finding is supported by the research of Thomas and Darling [18], which revealed a 43% increase in the likelihood of compliance with vaccination among college graduates, extending to their children as well. Furthermore, due to their lack of income sources and remote residency, these individuals heavily relied on the free medical assistance provided at the barangay health center, which prompted them to adhere rigorously to their children’s immunizations. Bryden et al. [19] concluded that remote areas with lower socioeconomic statuses in Australia demonstrated better vaccination compliance than significant cities. This outcome suggests that respondents in the chosen sitio exhibited higher levels of vaccination compliance, particularly among individuals who attended college but did not graduate, as income opportunities are limited.
Moreover, behavioral-specific cognitions display the highest mean among respondents who completed elementary education. A possible explanation for this is that parents with lower educational levels need more knowledge regarding health management, prompting them to rely on information provided by their barangay. A study conducted in India by Singh et al. [20] supported this claim by advocating for awareness and information dissemination among community leaders to improve vaccine compliance among individuals with lower levels of educational attainment.
It is important to acknowledge several limitations of this study. The sample size, while adequate, may not fully represent the broader population, especially considering factors like regional or socioeconomic disparities that could influence vaccine attitudes. Additionally, the cross-sectional nature of the research design limits the ability to infer causal relationships between psychosocial factors and vaccine compliance. The data collection method, a self-reported survey, could also introduce biases, such as social desirability bias, which might have influenced the accuracy of respondents’ answers regarding vaccine compliance. Future studies could benefit from larger, more diverse samples and longitudinal designs to better capture the dynamic relationship between psychosocial factors and vaccine adherence. Despite these limitations, the findings underscore the critical role of psychosocial and behavioral factors in shaping vaccination behaviors and highlight the need for targeted interventions to address these influences. It is also essential to consider how research design, sample size, and data collection methods may impact results, as these factors can affect the generalizability of the findings and our understanding of the psychosocial determinants of vaccine compliance.
Conclusion
The study findings reveal that the respondents’ profiles in barangay C contributed to their compliance with measles vaccination. Regarding age, it was found that younger adults were also decision-makers compared to middle-aged adults in the barangay. Meanwhile, concerning the decision-maker of the family and educational attainment, the majority happened to be mothers, and most respondents were high school graduates, respectively.
On the other hand, the study also found that more respondents strongly agreed to comply with the recommended age and number of doses of the measles vaccine for their children, influenced by both psychosocial factors and behavioral-specific cognitions. Additionally, among all the demographic profiles of the respondents, only the decision-maker in terms of psychosocial factors had a significant relationship with measles vaccine compliance, wherein mothers exhibited the highest level of adherence. This finding demonstrates that the psychosocial factors mentioned under Nola Pender’s Health Promotion Model influence mothers’ vaccine compliance through a complex interplay of individual beliefs, social interactions, and contextual factors. Thus, recognizing and addressing these factors through tailored health promotion interventions, targeted education campaigns, and supportive healthcare systems can increase vaccine compliance among mothers and promote public health.
Furthermore, our study findings should be included in improving platforms or campaigns that promote adherence to routine measles vaccination. In creating such programs, it is essential to emphasize awareness and vigilance regarding false information on social media and encourage family members to conduct further research about measles vaccination using reliable sources.
Overall, the research findings suggest that several factors must be considered when discussing measles vaccine compliance for children. These factors should be focused on promoting better health outcomes and preventing vaccine-preventable diseases from spreading. As future healthcare providers, we must emphasize the role of vaccinations, especially measles vaccination, in the community. This study would pave the way for a more compliant and healthier community in future generations.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Xavier University-Ateneo de Cagayan, Research Ethics Board, Cagayan de Oro, Philippines (Code: XU REC Package No. NSG-2024001281). Informed consent was obtained from all participants before their inclusion in the study.
Funding
The paper was extracted from the thesis of undergraduate students in the College of Nursing of Xavier University-Ateneo de Cagayan, Cagayan de Oro, Philippines.
Authors contributions
Conceptualization, data analysis, writing the manuscript: Rhy Kenji Enguio, Zenju Espinosa, Paolo Araune, and Ivy Go; Study design, data collection, review and editing: Ashley Jenn Fallarna, Ferdinand Gabriel Galarrita, Justine Jean Gullermo, Jasimah Gutoc, Rhea Mae Janolino, and Aleks Jimenez; Data interpretation and the literature review: Kayle Mae Labasano, Jade Godwin Lagua, Ariel Lacdo-O, and Edmund Zheen Regor Moreno; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all participants in this study for their time and cooperation.
References
Measles, characterized as an acute viral respiratory illness, poses a significant threat due to its highly contagious nature. Despite the availability of a safe and effective vaccine, measles has remained a prominent cause of mortality among young children worldwide, as noted by the World Health Organization (WHO) [1].
In the first two months of 2022, the global tally of reported measles cases surged by 79% compared to the corresponding period in 2021, as reported by the United Nations Children's Fund (UNICEF) [2]. This escalation was an early indicator of deficiencies in global immunization coverage. To address this shortfall, efforts led by WHO, in collaboration with UNICEF and other organizations, persisted in implementing programs to promote adherence to and supplying vaccines such as measles, mumps, and rubella (MMR) to various regions worldwide [2].
The inclusion of the MMR vaccine in Republic Act No. 10152, commonly known as the mandatory infants and children health immunization act of 2011, underscores the significance of immunization programs influenced by the Expanded Program on Immunization (EPI) [2]. This legislation mandates primary immunization against vaccine-preventable diseases for all children under five years old. As a result of this mandated law, the country experienced unprecedented success in reducing measles cases and fatalities for nearly two decades.
However, Hotez et al. highlighted a resurgence in measles transmission in the Philippines, attributing vaccine hesitancy as the primary cause [3]. A study by Domai et al. [4] revealed that the most substantial measles outbreak in the Western Pacific region, as designated by the WHO, occurred in the Philippines. This outbreak coincided with a decline in first-dose measles-containing vaccine coverage to 75% in 2018, as reported by the same study [4].
Moreover, the Philippine News Agency (PNA) [5] reported that measles cases had reached 289 in Northern Mindanao, with 38 cases, including three deaths, coming from the city of Cagayan de Oro. According to Luis [5], the City Health Office disclosed that most measles cases were in the barangays of Carmen, Lapasan, Cugman, and Balulang. Although the non-communicable diseases department had not declared an outbreak, it continually urged parents to be informed about vaccines.
Besides the increasing cases, the COVID-19 pandemic disrupted the delivery of routine immunization services, especially during the enhanced community quarantine in the Philippines. According to the study by Kurukkal [6], the ongoing pandemic has disrupted the delivery of childhood vaccines by increasing parents’ anxiety about exposing their children to COVID-19, leading them to keep their children well away from clinics. Additionally, healthcare workers were also reassigned from routine immunizations to COVID-19 vaccinations.
With all the mentioned determinants affecting the delivery of routine immunization services, the researchers of the study further investigated the factors affecting vaccine compliance, specifically measles inoculation in a selected barangay in Northern Mindanao, Philippines, called barangay C (for anonymity). The said barangay was the fifth barangay in the city with the largest population and was one of the adopted communities of Xavier University-Ateneo de Cagayan. Furthermore, since no studies were investigating the factors affecting vaccine compliance in the said research locale, the researchers aimed to address this gap.
The independent variables, including age, decision-maker, and educational attainment, were hypothesized to have impacted the dependent variable, the respondents’ measles vaccine compliance level. This study determined the factors influencing measles vaccine compliance among respondents in a selected barangay of a particular city in northern Mindanao. Additionally, it aimed to ascertain if there was a significant difference in the level of measles vaccine compliance when grouped according to age, decision-maker of the family, and educational attainment.
Material and Methods
Study design
The study employed a non-experimental quantitative research design, precisely the descriptive-correlational approach. This design allows for the observation and collection of data on the natural relationships between factors influencing measles vaccination compliance among families. The descriptive-correlational approach facilitates the identification of associations between dependent and independent variables without manipulating the variables, and therefore, no causal inferences are made [7].
Sample, sample size, sampling technique
The study was conducted in barangay C, one of the university’s partnered barangays, with the highest population of families with children under 5. Barangay C was chosen to ensure adequate representation of families with young children, a critical factor for the research. According to the 2020 census, barangay C had a population of 35238, representing 4.84% of the region’s total population [8]. The final research setting was selected based on its high concentration of families with children under five years old.
The respondents were selected based on the following criteria: residents aged 18 to 59 years, residing in the selected zone for at least six months, with children under five years old who had not received the first or second dose of the measles vaccine, had received only one dose or had received both doses. Additionally, the primary decision-makers of these families, regardless of educational attainment, were included in the study.
The researchers used the Cochran formula for sample size calculation to determine the ideal sample size. Assuming a household population (N) of 200 with children aged 0-5 years old in the selected zone, a 95% confidence level (z=1.96), a margin of error (e) of 0.05, and a variability (p) of 0.5, the calculated sample size was 132 respondents (n). This sample size was deemed sufficient for statistical power and to minimize sampling error.
Simple random sampling was employed to select participants from the identified households. As described by Thomas [9], simple random sampling is a primary probability sampling method where each individual in the population has an equal chance of being selected. This technique ensured strong internal and external validity and minimized selection and sampling biases, increasing the reliability and generalizability of the study’s findings.
Data collection process
For the data-gathering procedure, the researchers sent a letter of intent to the City Health Officer to obtain permission to access data from the chosen barangay’s primary health center and conduct the study. Upon receiving approval from the city health officer, the researchers, under the supervision of the barangay health nurse, were granted access to the list of zones of the chosen barangay and its corresponding residents.
The instrument of data collection
The researchers utilized a researcher-made questionnaire to gather primary data on factors influencing measles vaccine compliance, which was divided into two sections. The first section collected demographic information in a checklist format, including age, decision-maker, and educational attainment. The second section assessed factors influencing vaccine compliance using a 4-point Likert scale, categorized into psychosocial factors and behavioral-specific cognitions. To ensure validity, the questionnaire was reviewed by health experts familiar with the relevant factors, and a pilot test was conducted with a small sample from a different barangay to refine the instrument. The Cronbach α for the overall questionnaire was 0.85, indicating good internal consistency, with values of 0.80 for psychosocial factors and 0.82 for behavioral-specific cognitions, demonstrating acceptable reliability. Informed consent forms were provided, and respondents were oriented in both English and Bisaya to ensure a clear understanding of the study.
Data analysis
The t-test and analysis of variance (ANOVA)/F-tests were utilized to achieve the study’s objective. The t-test examined the significance of mean differences among various age groups, considering their variance or distribution, thereby measuring the magnitude of these differences. Additionally, the researchers applied ANOVA to ascertain any significant disparities in mean profiles concerning the family’s decision-maker and educational attainment. Subsequently, F tests were conducted to assess the statistical equality of means.
Results
A total of 132 respondents, aged 18 to 59 years, participated in the study. Most participants were female (65%) and served as the primary decision-makers in their households (80%). Most respondents had children under five years old, with a significant proportion having received at least one dose of the measles vaccine, while others had completed the full vaccination schedule.
Table 1 presents the differences in measles vaccine compliance based on age.
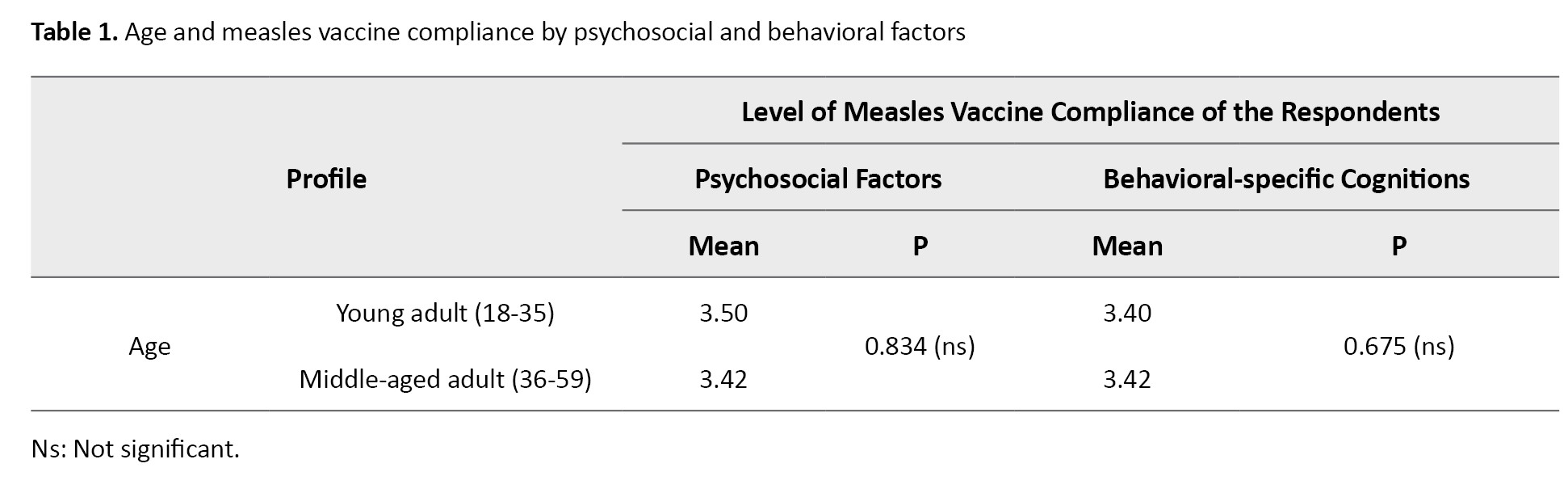
Younger adults (18-35 years) exhibited slightly higher compliance levels in psychosocial factors (mean=3.50) compared to middle-aged adults (36-59 years, mean=3.42). Conversely, middle adults showed slightly higher compliance regarding behavioral-specific cognitions (mean=3.42) than younger adults (mean=3.40). The t-test was performed to assess these differences, with P of 0.834 for psychosocial factors and 0.675 for behavioral-specific cognitions. Since both P exceeded the threshold of 0.05, the null hypothesis was accepted, suggesting no significant difference in measles vaccine compliance between younger and middle adults when grouped by age.
The underlying assumptions of the t-test, including the data’s normality and the variances’ homogeneity, were examined. The Shapiro-Wilk test was performed for normality, and the results showed no significant deviation from normality (P>0.05) for both psychosocial factors and behavioral-specific cognitions. The Levene’s test for equality of variances showed no significant differences in variances across the groups (P>0.05), supporting the validity of the t-test results.
Table 2 explores how the decision-maker in the household influences vaccine compliance.
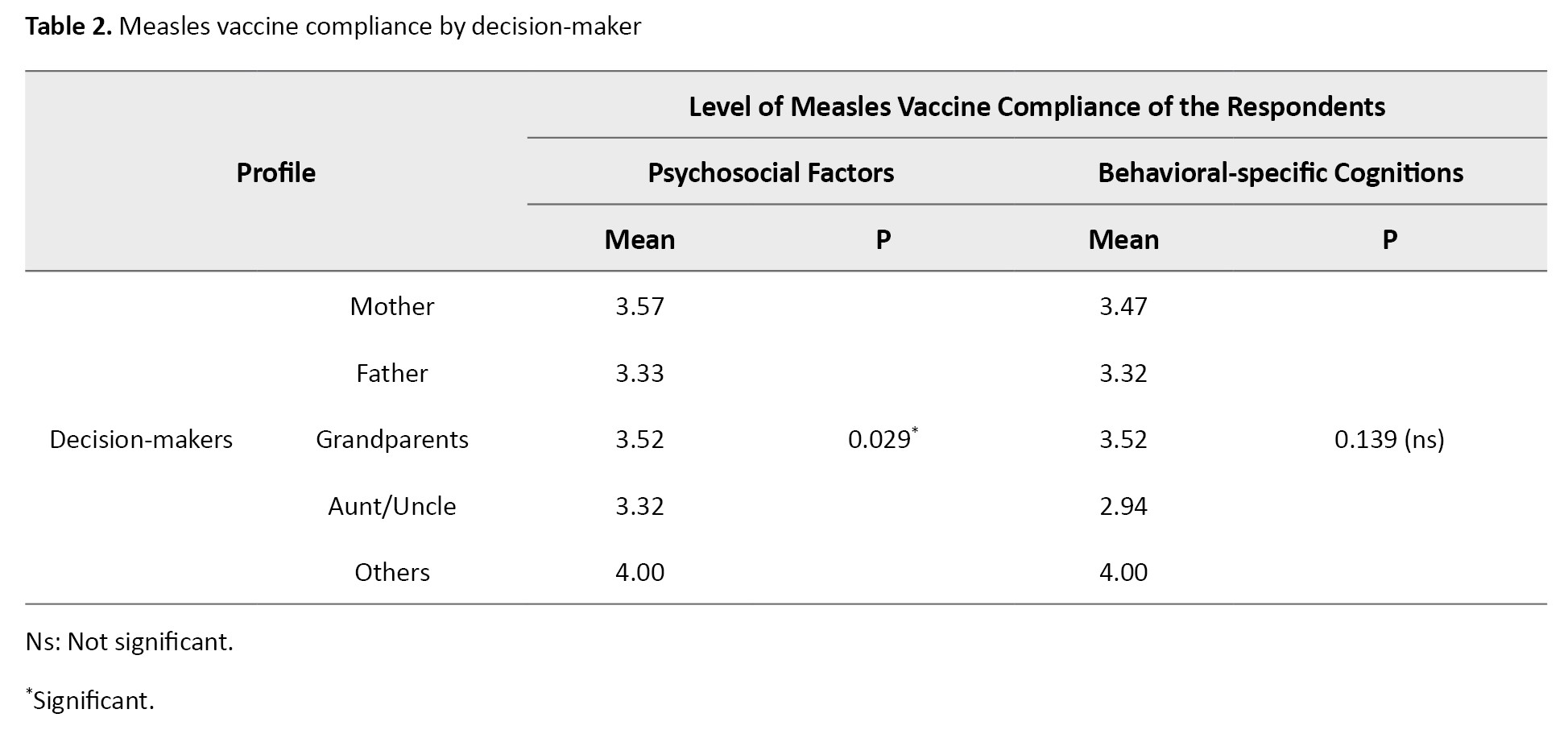
Mothers exhibited the highest compliance in psychosocial factors (mean=3.57) compared to other decision-makers. This condition highlights the significant role that psychological factors and social-cultural contexts may play in mothers’ decisions regarding vaccination. The ANOVA showed a significant P of 0.029 for psychosocial factors, indicating a statistically significant difference between decision-makers. However, the P for behavioral-specific cognitions (0.139) was above 0.05, indicating no significant difference in this domain.
The assumptions for the ANOVA test were also checked. The data met the normality assumption, with the Shapiro-Wilk test indicating no significant departure from normality (P>0.05) for both psychosocial factors and behavioral-specific cognitions. Homogeneity of variances was confirmed using Levene’s test (P=0.617 for psychosocial factors and P=0.838 for behavioral-specific cognitions), supporting the validity of the ANOVA results.
Table 3 examines measles vaccine compliance by respondents’ highest educational attainment.
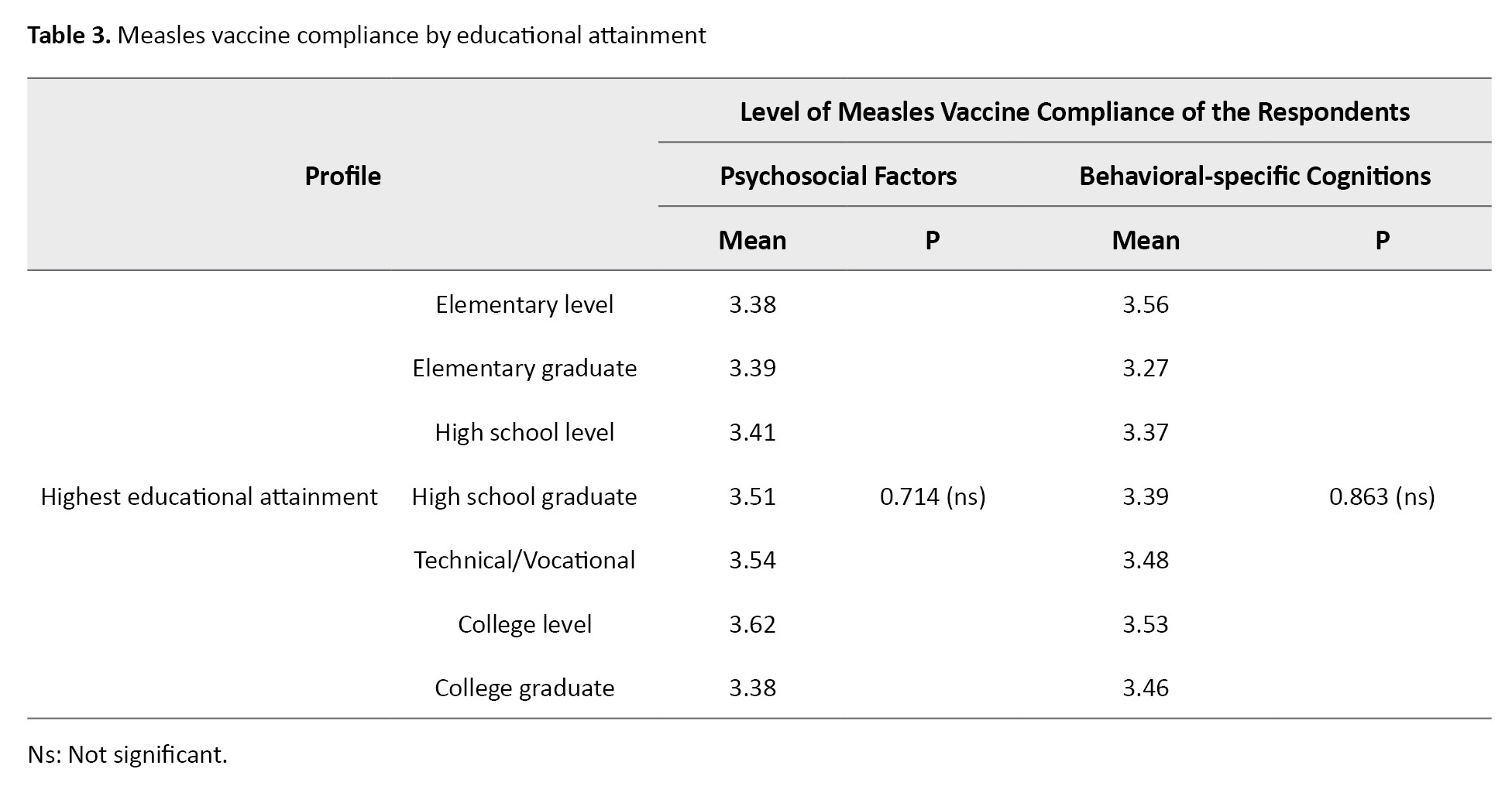
For psychosocial factors, individuals with some college education (mean=3.62) showed the highest compliance levels, suggesting that psychological and social contexts may be particularly influential at this education level. Interestingly, decision-makers with only elementary education (mean=3.56) had the highest compliance for behavioral-specific cognitions, possibly indicating that their perceptions, behavior, and motivation were influential in their vaccine compliance. ANOVA results for both psychosocial factors (P=0.714) and behavioral-specific cognitions (P=0.863) showed no significant differences across educational attainment groups, as both P exceeded 0.05.
As with Table 2, the assumptions for the ANOVA test were tested. Normality was confirmed through the Shapiro-Wilk test (P>0.05), and homogeneity of variance was validated with Levene’s test (P=0.746 for psychosocial factors and P=0.648 for behavioral-specific cognitions), ensuring that the assumptions of the test were met.
These findings suggest that factors such as the decision-maker’s role in the household and age may influence measles vaccine compliance, though differences in educational attainment did not significantly impact compliance levels. The lack of statistically significant differences in some areas calls for further exploration of additional variables that might affect vaccine uptake.
Discussion
A higher level of compliance concerning psychosocial factors was observed among younger adults, implying that self-motivation, perceived health status, definition of health, education, and cultural or religious beliefs greatly influence them. This result also indicated that younger adult respondents tended to rely more on their competence regarding measles vaccine adherence.
On the other hand, middle-aged individuals exhibited greater adherence to behavioral-specific cognitions, suggesting that factors such as perceived benefits of action, perceived barriers to action, perceived self-efficacy, activity-related effect, interpersonal influences, and situational influences significantly influenced their compliance with routine measles vaccination. This finding also implies that middle-aged respondents are more susceptible to the influence of their social circles when making decisions regarding measles vaccination compliance.
According to the study by Shati et al. [10], parents aged 20-30 believed that vaccination may not pose more risk to children than adults, leading to higher vaccine compliance among children with younger adult parents. However, Lampkin [11] stated that more than half of persons over 50 reported not knowing whom to believe regarding vaccine information. Additionally, Migriño et al. [12] supported the findings from this Table, which stated no significant associations between reasons for vaccine refusal and the respondents’ demographic data, such as their age.
The high level of compliance regarding psychosocial factors among the respondents, specifically the mothers, can be attributed to the nature of Filipino households. Filipino culture often strongly emphasizes the role of mothers as caregivers and nurturers. This cultural expectation further contributed to mothers’ heightened awareness and responsibility regarding their children’s health, including vaccine compliance. The pressure to fulfill societal expectations has increased vigilance and motivation among the respondents to ensure their children’s well-being, including adherence to vaccination schedules.
Moreover, Filipino mothers tended to have strong social support networks, including extended family members, friends, and fellow mothers in their communities. These networks play a significant role in shaping attitudes, beliefs, and behaviors related to vaccines. Social support provided validation, information sharing, and reinforcement of vaccine compliance practices. The influence of social networks on mothers’ compliance was pronounced due to their active engagement in the community or their close relationship with fellow mothers.
These findings are consistent with the results of a cross-sectional survey of parents in Italy by Della Polla et al. [13]. The study found that mothers were more likely to have positive attitudes toward HPV vaccination than fathers, which predicted their children’s vaccination status. Moreover, this study observed that parents’ attitudes toward the vaccine tended to be affected by their knowledge and awareness of the HPV vaccine, indicating the significant role of psychosocial factors in affecting adherence to vaccinations.
Another study supporting the importance of psychosocial factors is the review by Balgovind and Mohammadnezhad [14]. From the 44 studies they reviewed, factors affecting childhood immunization were identified and summarized into four themes: Parental knowledge, attitudes, and beliefs about vaccines. Furthermore, it shows that parents with limited knowledge about vaccines are less likely to be compliant or have a positive attitude toward vaccines, which is similar to the findings of this study, except that the respondents in this study displayed a more positive attitude, hence a higher level of compliance.
Regarding Nola Pender’s Health Promotion Model [15], the findings agree that a person’s psychological traits and sociocultural characteristics can significantly shape their health-promoting behaviors, which, in this study, involved compliance or adherence to vaccination recommendations. Mothers’ characteristics, such as their knowledge, beliefs, attitudes, and past experiences, influence their vaccine compliance. Their social environment and interactions with others also played a crucial role, as supported by Nola Pender’s propositions [16]. Psychosocial factors indeed played a role in the health-promoting behaviors of mothers.
Although the results indicated no significant difference in the respondents’ measles vaccine compliance level when grouped according to decision-makers regarding behavioral-specific cognitions, it showed that grandparents had the highest mean. This finding indicated that overall perceptions, behavior, and motivation were significant factors in the measles vaccine compliance of grandparents as decision-makers.
Similarly, in a study by Skitarelić et al. [16], wherein attitudes about childhood vaccinations between parents and grandparents were investigated and compared, it was observed that grandparents preferred children’s health benefits as a reason for vaccination by 9.19% more than parents. Furthermore, grandparents displayed less fear and suspicion toward vaccines than younger parents.
Upon examining the results, it was found that guardians who attended college but did not graduate exhibited higher compliance toward immunizing their children than those who graduated, particularly regarding psychosocial factors. Maybe these individuals spent much more time at home, whereas those who graduated pursued job opportunities, resulting in their time being occupied.
According to a study by Nguyen et al. [17], vaccine compliance hesitancy was higher among mothers who completed high school than those who attained a college education level. This trend was attributed to the higher educational exposure of college-aged individuals. College students typically have better access to information and possess enhanced health literacy, motivating them to make informed health decisions, particularly regarding their children’s health [18]. This finding is supported by the research of Thomas and Darling [18], which revealed a 43% increase in the likelihood of compliance with vaccination among college graduates, extending to their children as well. Furthermore, due to their lack of income sources and remote residency, these individuals heavily relied on the free medical assistance provided at the barangay health center, which prompted them to adhere rigorously to their children’s immunizations. Bryden et al. [19] concluded that remote areas with lower socioeconomic statuses in Australia demonstrated better vaccination compliance than significant cities. This outcome suggests that respondents in the chosen sitio exhibited higher levels of vaccination compliance, particularly among individuals who attended college but did not graduate, as income opportunities are limited.
Moreover, behavioral-specific cognitions display the highest mean among respondents who completed elementary education. A possible explanation for this is that parents with lower educational levels need more knowledge regarding health management, prompting them to rely on information provided by their barangay. A study conducted in India by Singh et al. [20] supported this claim by advocating for awareness and information dissemination among community leaders to improve vaccine compliance among individuals with lower levels of educational attainment.
It is important to acknowledge several limitations of this study. The sample size, while adequate, may not fully represent the broader population, especially considering factors like regional or socioeconomic disparities that could influence vaccine attitudes. Additionally, the cross-sectional nature of the research design limits the ability to infer causal relationships between psychosocial factors and vaccine compliance. The data collection method, a self-reported survey, could also introduce biases, such as social desirability bias, which might have influenced the accuracy of respondents’ answers regarding vaccine compliance. Future studies could benefit from larger, more diverse samples and longitudinal designs to better capture the dynamic relationship between psychosocial factors and vaccine adherence. Despite these limitations, the findings underscore the critical role of psychosocial and behavioral factors in shaping vaccination behaviors and highlight the need for targeted interventions to address these influences. It is also essential to consider how research design, sample size, and data collection methods may impact results, as these factors can affect the generalizability of the findings and our understanding of the psychosocial determinants of vaccine compliance.
Conclusion
The study findings reveal that the respondents’ profiles in barangay C contributed to their compliance with measles vaccination. Regarding age, it was found that younger adults were also decision-makers compared to middle-aged adults in the barangay. Meanwhile, concerning the decision-maker of the family and educational attainment, the majority happened to be mothers, and most respondents were high school graduates, respectively.
On the other hand, the study also found that more respondents strongly agreed to comply with the recommended age and number of doses of the measles vaccine for their children, influenced by both psychosocial factors and behavioral-specific cognitions. Additionally, among all the demographic profiles of the respondents, only the decision-maker in terms of psychosocial factors had a significant relationship with measles vaccine compliance, wherein mothers exhibited the highest level of adherence. This finding demonstrates that the psychosocial factors mentioned under Nola Pender’s Health Promotion Model influence mothers’ vaccine compliance through a complex interplay of individual beliefs, social interactions, and contextual factors. Thus, recognizing and addressing these factors through tailored health promotion interventions, targeted education campaigns, and supportive healthcare systems can increase vaccine compliance among mothers and promote public health.
Furthermore, our study findings should be included in improving platforms or campaigns that promote adherence to routine measles vaccination. In creating such programs, it is essential to emphasize awareness and vigilance regarding false information on social media and encourage family members to conduct further research about measles vaccination using reliable sources.
Overall, the research findings suggest that several factors must be considered when discussing measles vaccine compliance for children. These factors should be focused on promoting better health outcomes and preventing vaccine-preventable diseases from spreading. As future healthcare providers, we must emphasize the role of vaccinations, especially measles vaccination, in the community. This study would pave the way for a more compliant and healthier community in future generations.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Xavier University-Ateneo de Cagayan, Research Ethics Board, Cagayan de Oro, Philippines (Code: XU REC Package No. NSG-2024001281). Informed consent was obtained from all participants before their inclusion in the study.
Funding
The paper was extracted from the thesis of undergraduate students in the College of Nursing of Xavier University-Ateneo de Cagayan, Cagayan de Oro, Philippines.
Authors contributions
Conceptualization, data analysis, writing the manuscript: Rhy Kenji Enguio, Zenju Espinosa, Paolo Araune, and Ivy Go; Study design, data collection, review and editing: Ashley Jenn Fallarna, Ferdinand Gabriel Galarrita, Justine Jean Gullermo, Jasimah Gutoc, Rhea Mae Janolino, and Aleks Jimenez; Data interpretation and the literature review: Kayle Mae Labasano, Jade Godwin Lagua, Ariel Lacdo-O, and Edmund Zheen Regor Moreno; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all participants in this study for their time and cooperation.
References
- World Health Organization (WHO). UNICEF and WHO warn of perfect storm of conditions for measles outbreaks, affecting children. Geneva: WHO; 2022. [Link]
- UNICEF. UNICEF, protecting every child in the Philippines now and then through the power of vaccines. Manila: UNICEF; 2021. [Link]
- Hotez PJ, Nuzhath T, Colwell B. Combating vaccine hesitancy and other 21st century social determinants in the global fight against measles. Current Opinion in Virology. 2020; 41:1-7. [DOI:10.1016/j.coviro.2020.01.001] [PMID]
- Domai FM, Agrupis KA, Han SM, Sayo AR, Ramirez JS, Nepomuceno R, et al. Measles outbreak in the Philippines: Epidemiological and clinical characteristics of hospitalized children, 2016-2019. The Lancet Regional Health. Western Pacific. 2021; 19:100334.[DOI:10.1016/j.lanwpc.2021.100334] [PMID]
- Orias PJ. City Health Office urges parents to immunize kids [Internet]. 2019 [Updated 5 Feb 2019]. Available from: [Link]
- Kurukkal A. South Africa’s measles outbreak part of a global issue. Epicentre [Internet]. 2022. [Updated 2024 Feb 11].
- eCampusOntario. Psychologists use descriptive, correlational, and experimental research designs to understand behaviour [Internet]. 2024 [Updated2024 Feb 11]. Available from: [Link]
- PhilAtlas. Cagayan de Oro [Internet]. 2022. [Updated 2024 Feb 11]. Available from: [Link]
- Thomas L. Simple random sampling | definition, steps & examples. Amsterdam: Scribbr; 2020. [Link]
- Shati AA, Al-Qahtani SM, Alsabaani AA, Mahmood SE, Alqahtani YA, AlQahtani KM, et al. Perceptions of parents towards COVID-19 vaccination in children, Aseer Region, Southwestern Saudi Arabia. Vaccines. 2022; 10(8):1222. [DOI:10.3390/vaccines10081222] [PMID]
- Lampkin C. 2020 Vaccine Survey Topline Overview. Washington, DC: AARP Research; 2021. [Link]
- Migriño J Jr, Gayados B, Birol KRJ, De Jesus L, Lopez CW, Mercado WC, et al. Factors affecting vaccine hesitancy among families with children 2 years old and younger in two urban communities in Manila, Philippines. Western Pacific Surveillance and Response Journal. 2020; 11(2):20-6. [DOI:10.5365/wpsar.2019.10.2.006] [PMID]
- Della Polla G, Pelullo CP, Napolitano F, Angelillo IF. HPV vaccine hesitancy among parents in Italy: a cross-sectional study. Human Vaccines & Immunotherapeutics. 2020; 16(11):2744-51. [PMID]
- Balgovind P, Mohammadnezhad M. Factor’s affecting childhood immunization: thematic analysis of parents and healthcare workers’ perceptions. Human Vaccines & Immunotherapeutics. 2022; 18(6):2137338. [DOI:10.1080/21645515.2022.2137338] [PMID]
- Gonzalo A. Nola Pender: Health promotion model. London: Nurseslabs; 2023. [Link]
- Skitarelić N, Vidaić M, Skitarelić N. Parents’ versus grandparents’ attitudes about childhood vaccination. Children (Basel). 2022; 9(3):345. [PMID]
- Nguyen KH, Srivastav A, Lindley MC, Fisher A, Kim D, Greby SM, et al. Parental vaccine hesitancy and association with childhood diphtheria, tetanus toxoid, and acellular pertussis; measles, mumps, and rubella; rotavirus; and combined 7-series vaccination. American Journal of Preventive Medicine. 2022; 62(3):367-76. [DOI:10.1016/j.amepre.2021.08.015] [PMID]
- Thomas K, Darling J. Education is now a bigger factor than race in desire for COVID-19 vaccine. Los Angeles: The University of Southern California; 2021. [Link]
- Bryden GM, Browne M, Rockloff M, Unsworth C. The privilege paradox: Geographic areas with highest socioeconomic advantage have the lowest rates of vaccination. Vaccine. 2019; 37(32):4525-32. [DOI:10.1016/j.vaccine.2019.06.060] [PMID]
- Singh SK, Sahu D, Singh IP, Vashi MD. Perceptions of childhood vaccination practices among beneficiaries and healthcare service providers in slums under the national immunization program of India: a qualitative study. Journal of Health Research. 2021; 36(4):629-40. [DOI:10.1108/JHR-06-2020-0211]
Type of Study: Original Article |
Subject:
Community Health
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






